北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (3): 549-554. doi: 10.19723/j.issn.1671-167X.2021.03.018
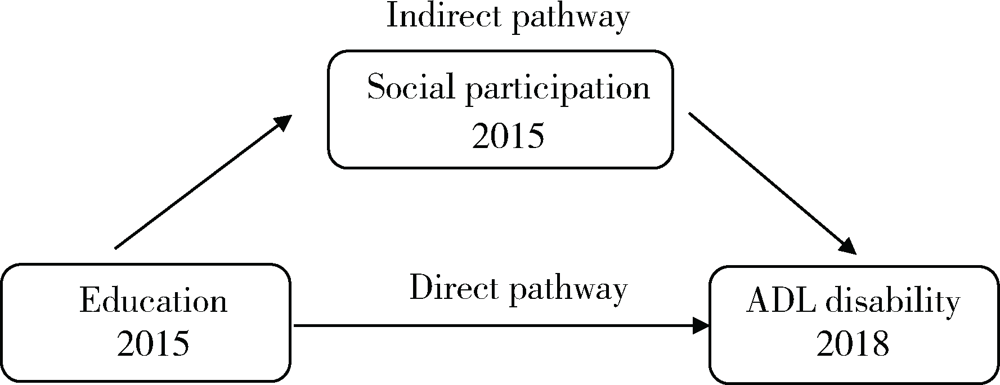
中国中老年居民教育程度与失能发生:社会参与的中介作用
- 北京大学公共卫生学院卫生政策与管理系,北京 100191
Association between education and the onset of disability in activities of daily living in middle-aged and older Chinese adults: The mediator role of social participation
PENG Shun-zhuang,FU Xi-xi,FENG Xing-linΔ( )
)
- Department of Health Policy and Management, Peking University School of Public Health, Beijing 100191, China
摘要:
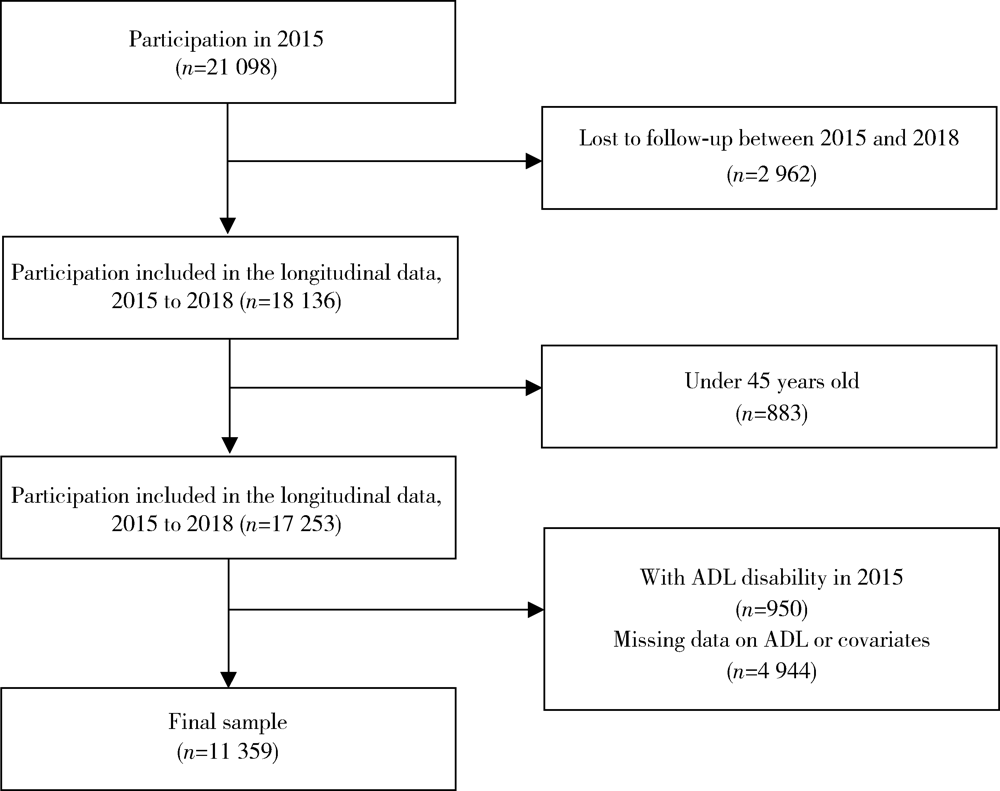
目的: 探究中老年人群教育程度与失能发生的关系及社会参与的中介作用。方法: 样本来源于中国健康与养老追踪调查(China Health and Retirement Longitudinal Study, CHARLS)2015年和2018年的追踪数据。教育程度、社会参与及其他变量采用2015年数据进行测量,失能则来源于2018年数据。采用卡方检验比较未受过教育(文盲)和受过教育(非文盲)组的个人特征和社会参与情况,采用Logistic回归分析教育程度及社会参与和失能发生之间的关系,并利用中介效应分析验证社会参与的中介作用。结果: 共纳入11 359名45岁及以上的中老年人,其中3 222人为文盲,文盲与非文盲人群失能的发生率分别为10.4%和6.2%。调查对象的社会参与度较低,仅为50%。在8项社交活动中,跟朋友交往(34.1%)比例最高,参加培训课程(0.6%)比例最低,文盲人群参与各项社交活动的比例均低于非文盲人群(P值均小于0.001)。与非文盲人群相比,文盲者失能发生的风险较高,调整后的比值比(adjusted odds ratio,aOR)为1.22(95%CI:1.02~1.45),且社会参与与失能的发生呈显著负相关(aOR=0.73,95%CI:0.63~0.85)。中介效应分析表明,社会参与可部分解释低教育程度对失能发生的不良影响,解释程度为12.22%。结论: 积极参与社交活动可缓解低教育水平对失能发生的不良影响,应鼓励中老年人,尤其是低教育水平的中老年人积极参与社交活动,可在一定程度上预防失能的发生。
中图分类号:
- R195
| [1] | 中华人民共和国国家统计局. 中国统计年鉴 [M]. 北京: 中国统计出版社, 2019: 9-24. |
| [2] | 中华人民共和国民政部. 三部门发布第四次中国城乡老年人生活状况抽样调查成果 [EB/OL]. (2016-10-09) [2021-02-10]. http://jnjd.mca.gov.cn/article/zyjd/xxck/201610/20161000886652.shtml. |
| [3] |
Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States[J]. N Engl J Med, 2006,355(7):695-703.
doi: 10.1056/NEJMsa044316 |
| [4] | 张文娟, 魏蒙. 中国老年人的失能水平和时间估计: 基于合并数据的分析[J]. 人口研究, 2015,39(5):3-14. |
| [5] | 尹志勤, 杨玉霞, 陈丽莉, 等. 浙江省农村老年人健康状况及影响因素分析[J]. 中国公共卫生, 2012,28(3):293-295. |
| [6] |
Zimmer Z, House JS. Education, income, and functional limitation transitions among American adults: contrasting onset and progression[J]. Int J Epidemiol, 2003,32(6):1089-1097.
doi: 10.1093/ije/dyg254 |
| [7] | 朱春燕, 郭晴, 田庆丰, 等. 河南省老年人综合能力失能现况及影响因素研究[J]. 中国全科医学, 2021,24(12):1500-1505. |
| [8] |
Ma X, Piao X, Oshio T. Impact of social participation on health among middle-aged and elderly adults: evidence from longitudinal survey data in China[J]. BMC Public Health, 2020,20(1):502.
doi: 10.1186/s12889-020-08650-4 |
| [9] |
Aida J, Kondo K, Kawachi I, et al. Does social capital affect the incidence of functional disability in older Japanese? A prospective population-based cohort study[J]. J Epidemiol Community Health, 2013,67(1):42-47.
doi: 10.1136/jech-2011-200307 pmid: 22760221 |
| [10] |
Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function[J]. JAMA, 1963,185(12):914-919.
doi: 10.1001/jama.1963.03060120024016 |
| [11] |
Liu N, Cadilhac DA, Kilkenny MF, et al. Changes in the prevalence of chronic disability in China: evidence from the China Health and Retirement Longitudinal Study[J]. Public Health, 2020,185:102-109.
doi: S0033-3506(20)30104-9 pmid: 32603874 |
| [12] |
Liu GG, Xue X, Yu C, et al. How does social capital matter to the health status of older adults? Evidence from the China Health and Retirement Longitudinal Survey[J]. Econ Hum Biol, 2016,22:177-189.
doi: 10.1016/j.ehb.2016.04.003 |
| [13] |
Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models[J]. Stata J, 2011,11(3):420-438.
doi: 10.1177/1536867X1101100306 |
| [14] |
Xu X, Yang L, Miao X, et al. An investigation and analysis of the activities of daily living of older adults living at home in Ningxia Hui Autonomous Region of China: A cross-sectional study[J]. BMC Geriatr, 2020,20(1):369.
doi: 10.1186/s12877-020-01765-8 |
| [15] |
Enroth L, Veenstra M, Aartsen M, et al. Are there educational disparities in health and functioning among the oldest old? Evidence from the Nordic countries[J]. Eur J Ageing, 2019,16(4):415-424.
doi: 10.1007/s10433-019-00517-x pmid: 31798367 |
| [16] | 林雁, 董正娇, 许传志, 等. 昆明市社区60岁以上老年人失能状况、影响因素及与健康效用的关系[J]. 昆明医科大学学报, 2020,41(4):44-50. |
| [17] |
Xin Y, Ren X. Social capital as a mediator through the effect of education on depression and obesity among the elderly in China[J]. Int J Environ Res Public Health, 2020,17(11):3977.
doi: 10.3390/ijerph17113977 |
| [18] | Eikemo TA, Bambra C, Huijts T, et al. The first pan-European sociological health inequalities survey of the general population: The European social survey rotating module on the social determinants of health[J]. Eur Sociol Rev, 2016,33(1):137-153. |
| [19] | Feng Z, Cramm JM, Jin C, et al. The longitudinal relationship between income and social participation among Chinese older people[J]. SSM Popul Health, 2020,11:100636. |
| [20] |
Scheffler RM, Brown TT. Social capital, economics, and health: new evidence[J]. Health Econ Policy Law, 2008,3(Pt 4):321-331.
doi: 10.1017/S1744133108004593 pmid: 18793475 |
| [21] | 中华人民共和国中央人民政府. 中共中央国务院印发《“健康中国2030”规划纲要》 [EB/OL]. (2016-10-25) [2021-02-10]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm. |
| [22] | 中华人民共和国中央人民政府. 健康中国行动(2019—2030年) [EB/OL]. (2019-07-15) [2021-02-10]. http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm. |
| [1] | 李志昌,侯云飞,周之伟,姜龙,张舒,林剑浩. 影响全膝关节置换术患者术前预期的患者因素[J]. 北京大学学报(医学版), 2022, 54(1): 170-176. |
| [2] | 李佳,徐钰,王优雅,高占成. 老年流感肺炎的临床特征及D-二聚体与疾病严重程度的相关性[J]. 北京大学学报(医学版), 2022, 54(1): 153-160. |
| [3] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [4] | 陈家丽,金月波,王一帆,张晓盈,李静,姚海红,何菁,李春. 老年发病类风湿关节炎的临床特征及其心血管疾病危险因素分析:一项大样本横断面临床研究[J]. 北京大学学报(医学版), 2020, 52(6): 1040-1047. |
| [5] | 宋逸,罗冬梅,胡佩瑾,闫晓晋,张京舒,雷园婷,张冰,马军. 1985--2014年中国汉族13~18岁中学生体质健康达标优秀率趋势分析[J]. 北京大学学报(医学版), 2020, 52(2): 317-322. |
| [6] | 陈健,左才红,张财义,杨明,张培训. 解剖型髓内钉和股骨近端防旋髓内钉治疗老年股骨转子间骨折的疗效比较[J]. 北京大学学报(医学版), 2019, 51(2): 283-287. |
| [7] | 徐小凤,陈茜,赵艺璞,胡秀英. 我国西部地区居家老年人生活自理能力调查分析[J]. 北京大学学报(医学版), 2018, 50(3): 457-462. |
| [8] | 魏滨,张华,徐懋,李民,王军,张利萍,郭向阳,赵一鸣,周方. 不同麻醉方法对髋部骨折老年患者术后转归的影响[J]. 北京大学学报(医学版), 2017, 49(6): 1008-1013. |
| [9] | 冯雪茹,刘梅林,刘芳,范琰,田清平. 阿司匹林剂量对高龄老年患者血小板功能的影响[J]. 北京大学学报(医学版), 2016, 48(5): 835-840. |
| [10] | 孟一森,王宇,范宇,苏杨,刘振华,虞巍,谌诚,周利群,张骞,何志嵩,金杰. 根治性膀胱全切手术及尿流改道方式对高龄患者围手术期并发症的影响[J]. 北京大学学报(医学版), 2016, 48(4): 632-637. |
| [11] | 李宁,刘昊楠,龚晓峰,朱仕文,吴新宝,贺良. 北京某三甲医院股骨颈骨折住院患者现状的流行病学分析[J]. 北京大学学报(医学版), 2016, 48(2): 292-296. |
| [12] | 陈茜,张雪梅,胡秀英. 芦山地震6个月后老年人可疑创伤后应激障碍调查研究[J]. 北京大学学报(医学版), 2015, 47(6): 1046-1049. |
| [13] | 潘小川. 关注中国大气灰霾(PM2.5)对人群健康影响的新常态[J]. 北京大学学报(医学版), 2015, 47(3): 377-379. |
| [14] | 陈红涛, 姬爱平. 口腔急诊患者全身健康状况的临床分析[J]. 北京大学学报(医学版), 2015, 47(2): 344-348. |
| [15] | 李侗桐, 方任飞, 谢铮. 北京市老年人生命质量的社会决定因素[J]. 北京大学学报(医学版), 2014, 46(3): 450-454. |
|