北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (3): 560-565. doi: 10.19723/j.issn.1671-167X.2021.03.020
门诊患者健康素养对就医体验的影响及机制
王晓琪1,陈美君1,云青萍1,孙思伟1,2,王熙凯3,史宇晖1,纪颖1,管仲军3,常春1,Δ( )
)
- 1.北京大学公共卫生学院社会医学与健康教育学系,北京 100191
2.北京大学第六医院,北京 100191
3.首都医科大学卫生管理与教育学院,北京 100069
Impact of health literacy on patient experience of outpatients in China and its mechanism
WANG Xiao-qi1,CHEN Mei-jun1,YUN Qing-ping1,SUN Si-wei1,2,WANG Xi-kai3,SHI Yu-hui1,JI Ying1,GUAN Zhong-jun3,CHANG Chun1,Δ( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. Peking University Sixth Hospital, Beijing 100191, China
3. School of Health Management and Education, Capital Medical University, Beijing 100069, China
摘要:
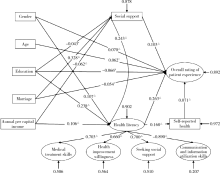
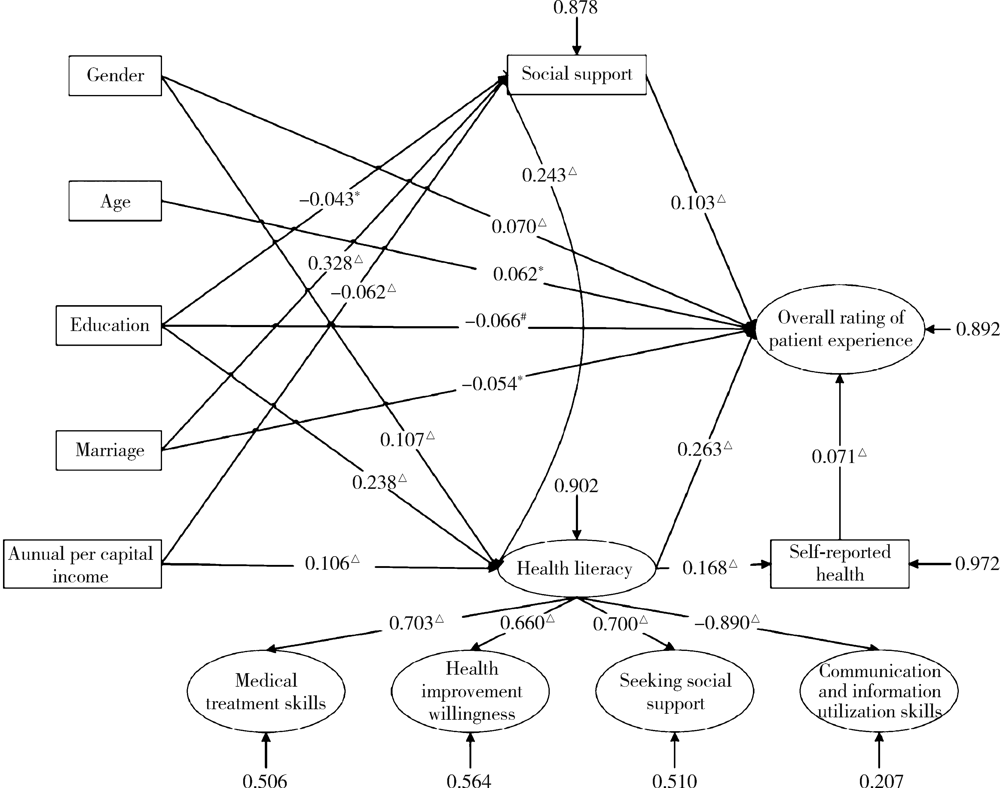
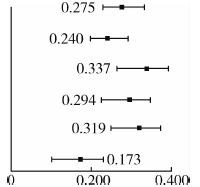
目的: 探究中国门诊患者的健康素养与就医体验之间的关联,分析其具体的影响机制。方法: 以安德森医疗卫生服务利用行为模型和健康素养技能模型为理论依据,构建患者层面的就医体验影响因素理论框架。采用滚雪球抽样法,通过线上电子问卷调查,利用自行设计的患者健康素养量表和北京协和医学院开发的中国门诊患者体验量表,评估门诊患者的健康素养和就医体验,构建结构方程模型探究两者之间的关系。结果: 最终纳入门诊患者2 773名,健康素养总得分的平均值为(90.72±12.90)分,就医体验综合评价的平均分为(3.71±0.74)分。结构方程模型分析结果表明,门诊患者的健康素养对其就医体验的综合评价产生积极影响,健康素养每提升一个标准差,就医体验增加0.275个单位。在就医体验的不同维度上,健康素养对就医体验总效应的标准化路径系数从高到低依次是:信息引导体验0.337,人文关怀体验0.319,诊疗行为体验0.294,流程效率体验0.240,环境设施体验 0.173。结论: 提升个体的健康素养水平,对于门诊患者的就医体验有显著促进作用,其中信息引导体验和人文关怀体验受健康素养影响最大。
中图分类号:
- R193
| [1] | Purcarea Th. V. Creating the ideal patient experience[J]. J Med Life, 2016,9(4):380-385. |
| [2] |
Male L, Noble A, Atkinson J, et al. Measuring patient experience: A systematic review to evaluate psychometric properties of patient reported experience measures (PREMs) for emergency care service provision[J]. Int J Qual Health Care, 2017,29(3):314-326.
doi: 10.1093/intqhc/mzx027 |
| [3] |
Gillespie H, Kelly M, Gormley G, et al. How can tomorrow’s doctors be more caring? A phenomenological investigation[J]. Med Educ, 2018,52(10):1052-1063.
doi: 10.1111/medu.13684 pmid: 30255523 |
| [4] | Yim CK, Shumate L, Barnett SH, et al. Health literacy assessment and patient satisfaction in surgical practice[J]. Ann Med Surg (Lond), 2018,35:25-28. |
| [5] |
Aoki T, Inoue M. Association between health literacy and patient experience of primary care attributes: A cross-sectional study in Japan[J]. PLoS One, 2017,12(9):e0184565.
doi: 10.1371/journal.pone.0184565 |
| [6] | 张建洁, 李金林, 曹雪丽. 患者就医满意度影响因素的实证分析[J]. 北京理工大学学报(社会科学版), 2018,20(1):102-109. |
| [7] |
Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter?[J]. J Health Soc Behav, 1995,36(1):1-10.
pmid: 7738325 |
| [8] | Andersen RM. Changing the U.S. Health Care System[M]. 3rd ed. New Jersey: John Wiley & Sons Inc., 2007: 1-30. |
| [9] | Squiers L, Peinado S, Berkman N, et al. The health literacy skills framework[J]. J Health Commun, 2012,17(3):30-54. |
| [10] |
Jordan J, Buchbinder R, Briggs A, et al. The health literacy ma-nagement scale (HeLMS): A measure of an individual’s capacity to seek, understand and use health information within the healthcare setting[J]. Patient Educ Couns, 2013,91(2):228-235.
doi: 10.1016/j.pec.2013.01.013 |
| [11] |
Hu G, Chen Y, Liu Q, et al. Patient experience of hospital care in China: Major findings from the Chinese patient experience questionnaire survey (2016-2018)[J]. BMJ Open, 2019,9(9):e031615.
doi: 10.1136/bmjopen-2019-031615 |
| [12] | 肖水源. 《社会支持评定量表》的理论基础与研究应用[J]. 临床精神医学杂志, 1994(2):98-100. |
| [13] | Wynia MK, Osborn CY. Health literacy and communication quality in health care organizations[J]. J Health Commun, 2010,15(2):102-115. |
| [14] | Schwartzberg JG, Cowett A, VanGeest J, et al. Communication techniques for patients with low health literacy: A survey of physicians, nurses, and pharmacists[J]. Am J Health Behav, 2007,31(1):S96-S104. |
| [15] |
Altin SV, Stock S. Impact of health literacy, accessibility and coordination of care on patient’s satisfaction with primary care in Germany[J]. BMC Fam Pract, 2015,16(1):148.
doi: 10.1186/s12875-015-0372-0 |
| [16] |
Altin SV, Stock S. The impact of health literacy, patient-centered communication and shared decision-making on patients’ satisfaction with care received in German primary care practices[J]. BMC Health Serv Res, 2016,16(1):450.
doi: 10.1186/s12913-016-1693-y |
| [17] |
Inoue M, Takahashi M, Kai I. Impact of communicative and critical health literacy on understanding of diabetes care and self-efficacy in diabetes management: A cross-sectional study of primary care in Japan[J]. BMC Fam Pract, 2013,14(1):40.
doi: 10.1186/1471-2296-14-40 |
| [1] | 蒋青,张雨. 新形势下运动损伤特点及细胞生物治疗的应用前景和挑战[J]. 北京大学学报(医学版), 2021, 53(5): 828-831. |
| [2] | 吴士艳,张旭熙,孙凯歌,胡康,刘思佳,孙昕霙. 慢性病高危人群和健康人群休闲类身体活动健康信念模式的多组结构方程模型分析[J]. 北京大学学报(医学版), 2018, 50(4): 711-716. |
| [3] | 曾庆奇, 常春, 蒋莹. 健康素养与高血压健康管理的关系[J]. 北京大学学报(医学版), 2014, 46(3): 492-497. |
| [4] | 郑迎东, 石建辉, 曹若湘. 中国居民健康素养调查问卷的验证性因子分析及其应用初探[J]. 北京大学学报(医学版), 2010, 42(3): 314-317. |
|