北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (2): 356-362. doi: 10.19723/j.issn.1671-167X.2022.02.025
颧骨缺损不同修复重建方法和预后的回顾性分析
- 北京大学口腔医学院·口腔医院口腔颌面外科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔生物材料和数字诊疗装备国家工程研究中心,口腔数字医学北京市重点实验室,北京 100081
Relationship between prognosis and different surgical treatments of zygomatic defects: A retrospective study
LAN Lin,HE Yang( ),AN Jin-gang,ZHANG Yi
),AN Jin-gang,ZHANG Yi
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
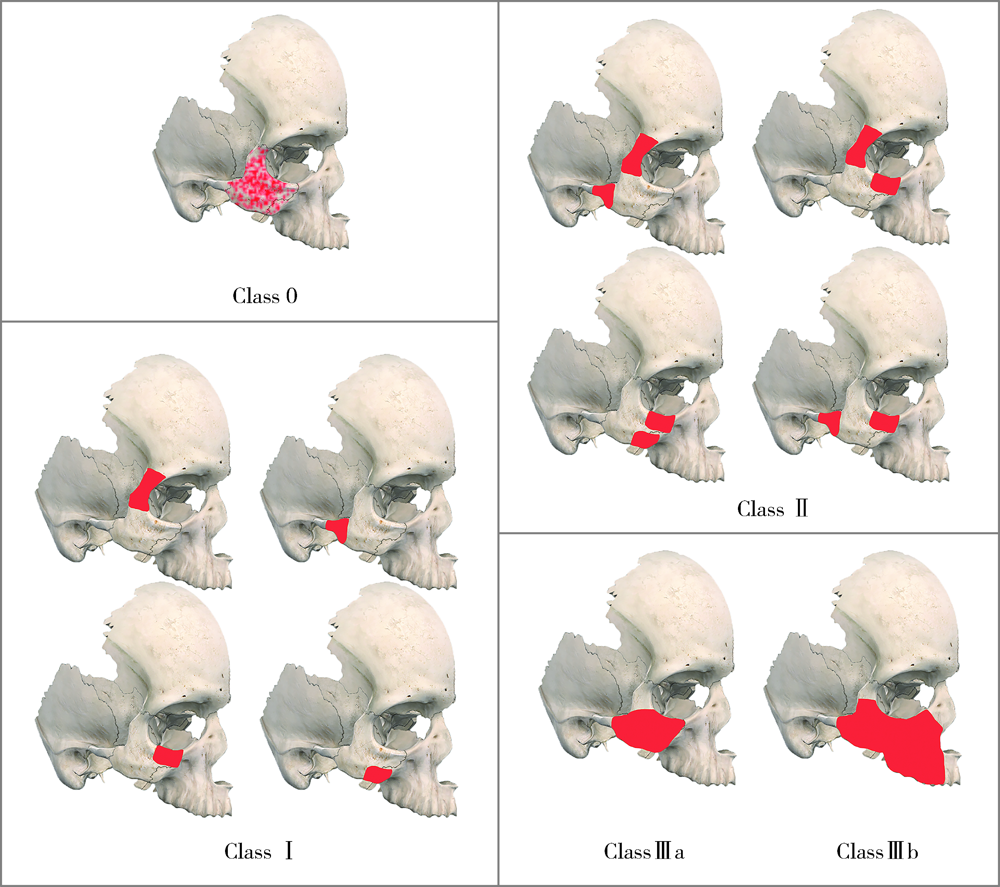
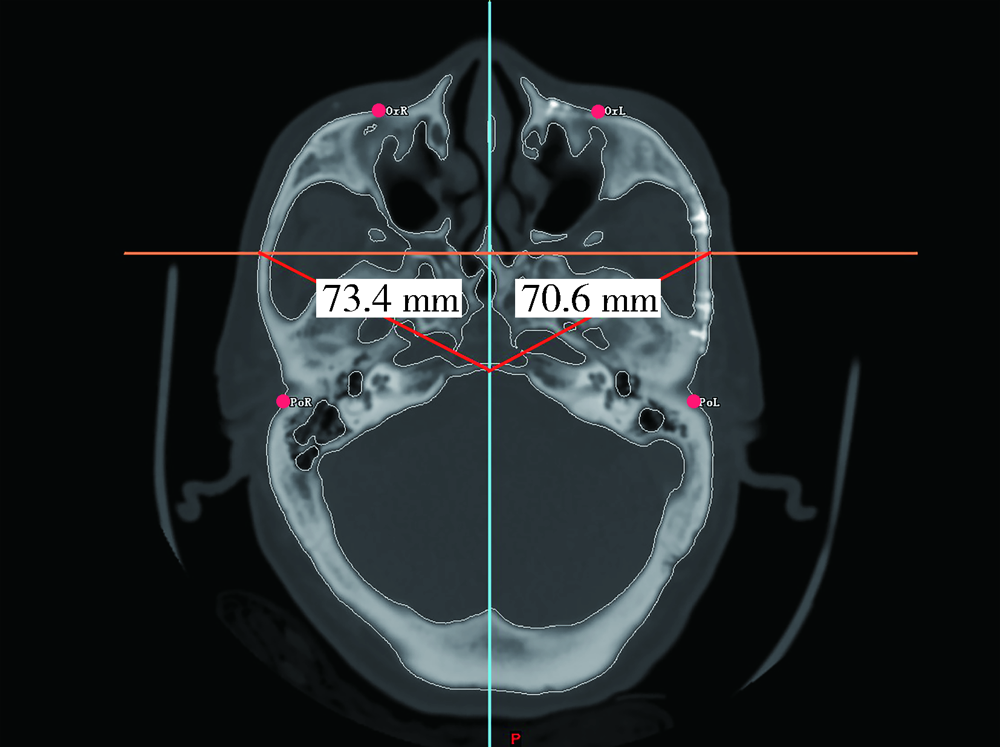
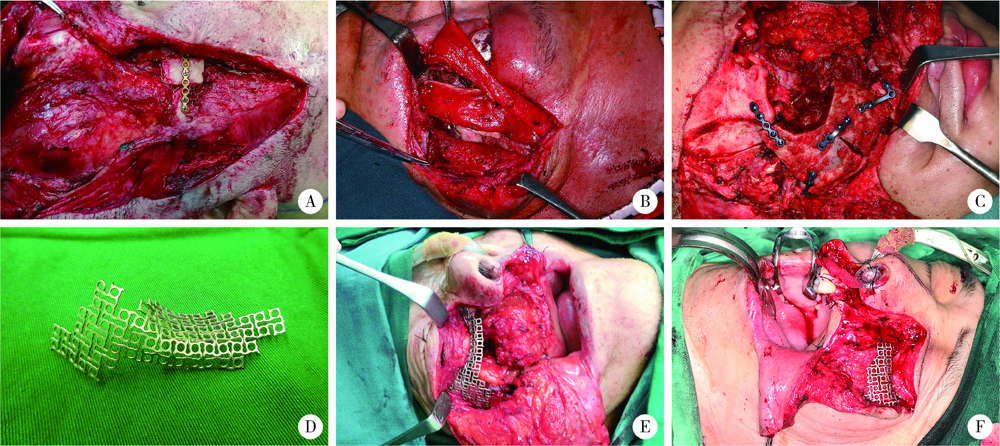
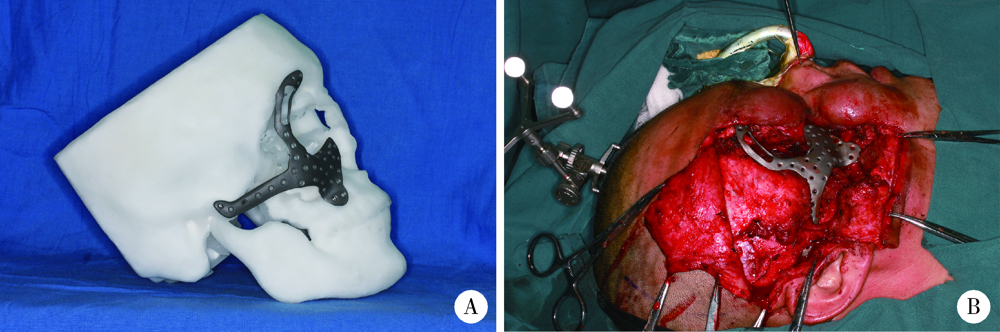
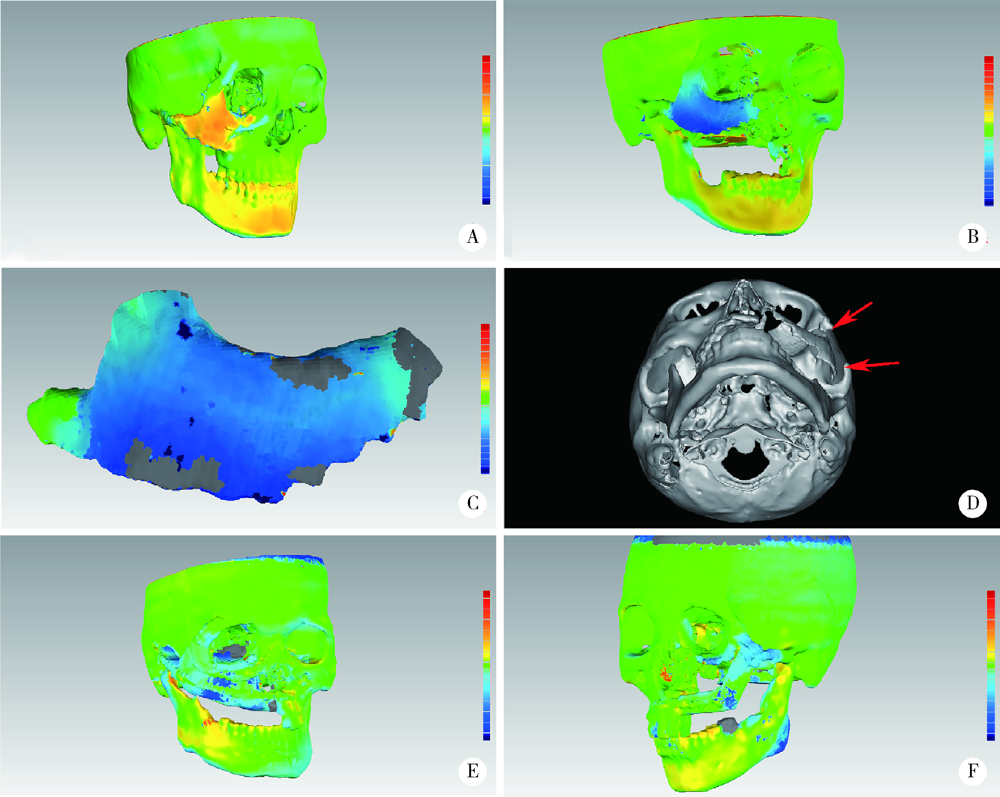
目的: 探讨颧骨缺损不同治疗方法的修复效果及特点。方法: 选择2012年8月至2019年8月于北京大学口腔医院口腔颌面外科就诊的颧骨缺损行修复重建的37例患者。根据颧骨缺损涉及的部位,将缺损分为四类:0类,缺损不涉及颧骨区段结构,仅为厚度(突度)变化;Ⅰ类,单个缺损位于颧骨体部或只涉及一个突起方向的缺损;Ⅱ类,单个缺损累及两个突起方向;Ⅲa类,单个缺损累及三个突起方向以上的缺损;Ⅲb类,颧骨缺损同时累及相应上颌骨的大范围缺损。统计分析各类颧骨缺损的病因、缺损时间、缺损大小及特点、采用的修复重建方式,并随访记录术后并发症等。术后CT评价颧骨突度及对称性恢复效果,进行色谱差值分析评价术后稳定效果。结果: 本组患者中,由创伤引起的颧骨缺损有25例(67.57%),肿瘤切除引起的颧骨缺损有11例(29.73%),另1例为骨发育畸形导致的颧骨缺损。19例患者行单纯自体骨移植修复,6例患者行血管化组织瓣修复,5例患者仅使用外植入物,另外7例患者使用血管化组织瓣联合外植入物修复。导航组和非导航组健、患侧颧骨突度差值中位数分别为0.45 mm(0.20~2.50 mm)和1.60 mm(0.10~2.90 mm),两组差值有统计学意义(P=0.045)。2例使用钛网结合股前外侧皮瓣修复的患者术后钛网发生明显变形或断裂,2例铸造个性化钛修复术后因感染而取出。结论: 对于无明显结构改变的颧骨缺损,可以用自体骨游离移植或异体材料修复。颧骨缺损存在骨支柱破坏、慢性炎症、口鼻腔相通或伴有明显软组织量不足时,建议带蒂颅骨骨膜瓣或血管化骨组织瓣修复。钛网可用于修复大量骨组织缺损的病例,同时建议联合血管化骨组织瓣移植修复。
中图分类号:
- R782.26
| [1] |
Kokemueller H, Tavassol F, Rücker M, et al. Complex midfacial reconstruction: A combined technique of computer-assisted surgery and microvascular tissue transfer[J]. J Oral Maxillofac Surg, 2008, 66(11):2398-2406.
doi: 10.1016/j.joms.2007.12.030 |
| [2] |
Zunz E, Blanc O, Leibovitch I. Traumatic orbital floor fractures: Repair with autogenous bone grafts in a tertiary trauma center[J]. J Oral Maxillofac Surg, 2012, 70(3):584-592.
doi: 10.1016/j.joms.2011.02.048 |
| [3] | 白萍, 刘和荣, 郝月军. Medpor在眼眶重建和眼球内陷复位手术中的应用[J]. 中国美容医学, 2004, 13(3):353-354. |
| [4] |
Butscher A, Bohner M, Hofmann S, et al. Structural and material approaches to bone tissue engineering in powder-based three-dimensional printing[J]. Acta Biomater, 2011, 7(3):907-920.
doi: 10.1016/j.actbio.2010.09.039 pmid: 20920616 |
| [5] |
Pensler J, McCarthy JG. The calvarial donor site: An anatomic study in cadavers[J]. Plast Reconstr Surg, 1985, 75(5):648-651.
pmid: 3983272 |
| [6] |
Markowitz NR. Cranial bone grafting in oral and maxillofacial surgery[J]. J Am Dent Assoc, 1992, 123(7):206-211.
pmid: 1619161 |
| [7] |
Tatum SA, Kellman RM. Cranial bone grafting in maxillofacial trauma and reconstruction[J]. Facial Plast Surg, 1998, 14(1):117-129.
pmid: 10371899 |
| [8] |
Kusiak JF, Zins JE, Whitaker LA. The early revascularization of membranous bone[J]. Plast Reconstr Surg, 1985, 76(4):510-516.
pmid: 4034769 |
| [9] |
Rogers GF, Greene AK. Autogenous bone graft: Basic science and clinical implications[J]. J Craniofac Surg, 2012, 23(1):323-327.
doi: 10.1097/SCS.0b013e318241dcba pmid: 22337435 |
| [10] |
Movahed R, Pinto LP, Morales-Ryan C, et al. Application of cranial bone grafts for reconstruction of maxillofacial deformities[J]. Proc (Bayl Univ Med Cent), 2013, 26(3):252-255.
doi: 10.1080/08998280.2013.11928973 pmid: 23814382 |
| [11] |
Vandervord JG, Watson JD, Teasdale GM. Forehead reconstruction using a bi-pedicled bone flap[J]. Br J Plast Surg, 1982, 35(1):75-79.
pmid: 7066592 |
| [12] |
He W, Gong X, He Y, et al. Application of a lateral pedicled cranial bone flap for the treatment of secondary zygomaticomaxillary defects[J]. J Craniofac Surg, 2019, 30(7):e661-e664.
doi: 10.1097/SCS.0000000000005776 |
| [13] |
Gerressen M, Pastaschek CI, Riediger D, et al. Microsurgical free flap reconstructions of head and neck region in 406 cases: A 13-year experience[J]. J Oral Maxillofac Surg, 2013, 71(3):628-635.
doi: 10.1016/j.joms.2012.07.002 |
| [14] |
Ghassemi A, Ghassemi M, Riediger D, et al. Comparison of donor-site engraftment after harvesting vascularized and nonvascularized iliac bone grafts[J]. J Oral Maxillofac Surg, 2009, 67(8):1589-1594.
doi: 10.1016/j.joms.2009.04.013 |
| [15] |
Takano M, Sugahara K, Koyachi M, et al. Maxillary reconstruction using tunneling flap technique with 3D custom-made titanium mesh plate and particulate cancellous bone and marrow graft: A case report[J]. Maxillofac Plast Reconstr Surg, 2019, 41(1):43.
doi: 10.1186/s40902-019-0228-y |
| [16] |
Ghanaati S, Al-Maawi S, Conrad T, et al. Biomaterial-based bone regeneration and soft tissue management of the individualized 3D-titanium mesh: An alternative concept to autologous transplantation and flap mobilization[J]. J Craniomaxillofac Surg, 2019, 47(10):1633-1644.
doi: S1010-5182(19)30459-7 pmid: 31420282 |
| [17] |
Zhang WB, Yu Y, Mao C, et al. Outcomes of zygomatic complex reconstruction with patient-specific titanium mesh using computer-assisted techniques[J]. J Oral Maxillofac Surg, 2019, 77(9):1915-1927.
doi: 10.1016/j.joms.2019.03.014 |
| [18] |
Mischkowski RA, Selbach I, Neugebauer J, et al. Lateral femoral cutaneous nerve and iliac crest bone grafts:Anatomical and clinical considerations[J]. Int J Oral Maxillofac Surg, 2006, 35(4):366-372.
doi: 10.1016/j.ijom.2005.08.010 |
| [19] |
Wei FC, Celik N, Yang WG, et al. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap[J]. Plast Reconstr Surg, 2003, 112(1):37-42.
doi: 10.1097/01.PRS.0000065911.00623.BD |
| [20] |
Hidalgo DA, Pusic AL. Free-flap mandibular reconstruction: A 10-year follow-up study[J]. Plastic Reconstr Surg, 2002, 110(2):438-449.
doi: 10.1097/00006534-200208000-00010 |
| [21] | Nickels L. World’s first patient-specific jaw implant[J]. Metal Powder Report, 2012, 67(2):12-14. |
| [22] |
Macheras G, Kateros K, Kostakos A, et al. Eight- to ten-year clinical and radiographic outcome of a porous tantalum monoblock acetabular component[J]. J Arthroplasty, 2009, 24(5):705-709.
doi: 10.1016/j.arth.2008.06.020 pmid: 18703310 |
| [23] |
Whitehouse MR, Masri BA, Duncan CP, et al. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years[J]. Clin Orthop Relat Res, 2015, 473(2):521-527.
doi: 10.1007/s11999-014-3861-x |
| [1] | 王飞,朱翔,贺蓓,朱红,沈宁. 自发缓解的滤泡性细支气管炎伴非特异性间质性肺炎1例报道并文献复习[J]. 北京大学学报(医学版), 2021, 53(6): 1196-1200. |
| [2] | 高伟波,石茂静,张海燕,吴春波,朱继红. 显著高铁蛋白血症与噬血细胞性淋巴组织细胞增多症的相互关系[J]. 北京大学学报(医学版), 2021, 53(5): 921-927. |
| [3] | 张梅香,史文芝,刘建新,王春键,李燕,王蔚,江滨. MLL-AF6融合基因阳性急性髓系白血病的临床特征及预后[J]. 北京大学学报(医学版), 2021, 53(5): 915-920. |
| [4] | 蒋艳芳,王健,王永健,刘佳,裴殷,刘晓鹏,敖英芳,马勇. 前交叉韧带翻修重建术后中长期临床疗效及影响因素[J]. 北京大学学报(医学版), 2021, 53(5): 857-863. |
| [5] | 肖若陶,刘承,徐楚潇,何为,马潞林. 术前血小板参数与局部进展期肾细胞癌预后[J]. 北京大学学报(医学版), 2021, 53(4): 647-652. |
| [6] | 于妍斐,何世明,吴宇财,熊盛炜,沈棋,李妍妍,杨风,何群,李学松. 延胡索酸水合酶缺陷型肾细胞癌的临床病理特征及预后[J]. 北京大学学报(医学版), 2021, 53(4): 640-646. |
| [7] | 赵勋,颜野,黄晓娟,董靖晗,刘茁,张洪宪,刘承,马潞林. 癌栓粘连血管壁对非转移性肾细胞癌合并下腔静脉癌栓患者手术及预后的影响[J]. 北京大学学报(医学版), 2021, 53(4): 665-670. |
| [8] | 陈怀安,刘硕,李秀君,王哲,张潮,李凤岐,苗文隆. 炎症生物标志物对输尿管尿路上皮癌患者预后预测的临床价值[J]. 北京大学学报(医学版), 2021, 53(2): 302-307. |
| [9] | 刘世博,高辉,冯元春,李静,张彤,万利,刘燕鹰,李胜光,罗成华,张学武. 腹膜后纤维化致肾盂积水的临床分析:附17例报道[J]. 北京大学学报(医学版), 2020, 52(6): 1069-1074. |
| [10] | 陈伟钱,戴小娜,余叶,王沁,梁钧昱,柯旖旎,易彩虹,林进. 原发性干燥综合征合并自身免疫性肝病的临床特点及预后分析[J]. 北京大学学报(医学版), 2020, 52(5): 886-891. |
| [11] | 程嗣达,李新飞,熊盛炜,樊书菠,王杰,朱伟杰,李子奡,丁光璞,俞婷,李万强,孙永明,杨昆霖,张雷,郝瀚,李学松,周利群. 机器人辅助腹腔镜上尿路修复手术:单一术者108例经验总结[J]. 北京大学学报(医学版), 2020, 52(4): 771-779. |
| [12] | 姜妮,乔国梁,王小利,周心娜,周蕾,宋雨光,赵艳杰,任军. 中性粒细胞与淋巴细胞比例对评估接受过继性细胞免疫治疗的晚期胰腺癌患者预后的临床意义[J]. 北京大学学报(医学版), 2020, 52(3): 597-602. |
| [13] | 马茹,李鑫宝,闫风彩,林育林,李雁. 肿瘤间质比评估阑尾来源腹膜假黏液瘤的临床价值[J]. 北京大学学报(医学版), 2020, 52(2): 240-246. |
| [14] | 王文鹏,王捷夫,胡均,王俊锋,刘嘉,孔大陆,李健. 结直肠间质瘤临床病理特征及预后分析[J]. 北京大学学报(医学版), 2020, 52(2): 353-361. |
| [15] | 王骁,李兆星,范焕芳,魏莉瑛,郭旭瑾,郭娜,王彤. 罕见小肠囊腺瘤1例报道[J]. 北京大学学报(医学版), 2020, 52(2): 382-384. |
|