Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (1): 53-58. doi: 10.19723/j.issn.1671-167X.2019.01.010
Previous Articles Next Articles
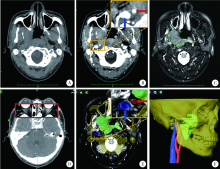
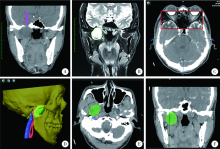
Multimodal image fusion technology for diagnosis and treatment of the skull base-infratemporal tumors
Rong YANG,Qing-xiang LI,Chi MAO,Xin PENG,Yang WANG,Yu-xing GUO( ),Chuan-bin GUO(
),Chuan-bin GUO( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R78
| [1] |
Choudhri AF, Parmar HA, Morales RE , et al. Lesions of the skull base: imaging for diagnosis and treatment[J]. Otolaryngol Clin North Am, 2012,45(6):1385-1404.
doi: 10.1007/978-3-642-35579-0_20 |
| [2] | 魏宏权 . 咽旁隙和颞下窝肿瘤的外科治疗进展[J]. 中国耳鼻咽喉颅底外科杂志, 2018,24(2):91-96, 102. |
| [3] |
郭玉兴, 彭歆, 刘筱菁 , 等. 导航技术在颅底-颞下区肿瘤手术中的应用[J]. 中华口腔医学杂志, 2013,48(11):645-647.
doi: 10.3760/cma.j.issn.1002-0098.2013.11.002 |
| [4] |
郭传瑸, 郭玉兴 . 外科导航技术引导的颅底肿瘤穿刺活检[J]. 中国实用口腔科杂志, 2014,7(6):321-324.
doi: 10.7504/kq.2014.06.001 |
| [5] |
Guo R, Guo YX, Feng Z , et al. Application of a computer-aided navigation technique in surgery for recurrent malignant infratemporal fossa tumors[J]. J Craniofac Surg, 2015,26(2):e126-132.
doi: 10.1097/SCS.0000000000001350 pmid: 25710743 |
| [6] |
Leong JL, Batra PS, Citardi MJ . CT-MR image fusion for the management of skull base lesions[J]. Otolaryngol Head Neck Surg, 2006,134(5):868-876.
doi: 10.1016/j.otohns.2005.11.015 pmid: 16647550 |
| [7] |
Guo Y, Guo C . Maxillary-fronto-temporal approach for removal of recurrent malignant infratemporal fossa tumors: Anatomical and clinical study[J]. J Craniomaxillofac Surg, 2014,42(3):206-212.
doi: 10.1016/j.jcms.2013.05.001 pmid: 23932542 |
| [8] |
Yacoub A, Anschuetz L, Schneider D , et al. Minimally invasive lateral endoscopic multiport approach to the infratemporal fossa: a cadaveric study[J]. World Neurosurg, 2018,112:e489-e496.
doi: 10.1016/j.wneu.2018.01.065 pmid: 29391297 |
| [9] | 李成才, 姚国杰, 杜威 , 等. 多模态影像融合在颅底肿瘤的诊断、治疗中的应用价值[J]. 中国临床神经外科杂志, 2018,23(3):145-148. |
| [10] |
O'Neill BE, Hochhalter CB, Carr C , et al.Advances in neuro-oncology imaging techniques[J]. Ochsner J, 2018,18(3):236-241.
doi: 10.31486/toj.17.0062 |
| [11] |
赵岩, 孙健, 杨学军 . 多模态影像融合技术在神经外科的应用及进展[J]. 中国现代神经疾病杂志, 2012,12(6):645-650.
doi: 10.3969/j.issn.1672-6731.2012.06.004 |
| [12] |
顾恒乐, 聂生东 . 多模医学图像配准和融合方法及其临床应用进展[J]. 中华放射肿瘤学杂志, 2016,25(8):902-906.
doi: 10.3760/cma.j.issn.1004-4221.2016.08.024 |
| [13] |
Inoue HK, Nakajima A, Sato H , et al. Image fusion for radiosurgery, neurosurgery and hypofractionated radiotherapy[J]. Cureus, 2015,7(3):e252.
doi: 10.7759/cureus.252 pmid: 26180676 |
| [14] |
Nemec SF, Donat MA, Mehrain S , et al. Ct-mr image data fusion for computer assisted navigated neurosurgery of temporal bone tumors[J]. Eur J Radiol, 2007,62(2):192-198.
doi: 10.1016/j.ejrad.2006.11.029 pmid: 17229539 |
| [15] |
Zhang SX, Han PH, Zhang GQ , et al. Comparison of spect/ct, mri and ct in diagnosis of skull base bone invasion in nasopharyngeal carcinoma[J]. Biomed Mater Eng, 2014,24(1):1117-1124.
doi: 10.3233/BME-130911 pmid: 24092081 |
| [16] |
Guo YX, Sun ZP, Liu XJ , et al. Surgical safety distances in the infratemporal fossa: three-dimensional measurement study[J]. Int J Oral Maxillofac Surg, 2015,44(5):555-561.
doi: 10.1016/j.ijom.2014.06.004 pmid: 25441861 |
| [17] |
吴东东, 卜博, 陈晓雷 , 等. 融合MRI与CT图像的多模态神经导航技术在颅底显微外科手术中的应用[J]. 解放军医学院学报, 2015, ( 5):411-414.
doi: 10.3969/j.issn.2095-5227.2015.05.002 |
| [18] |
Hayashi N, Kurimoto M, Hirashima Y , et al. Efficacy of navigation in skull base surgery using composite computer graphics of magnetic resonance and computed tomography images[J]. Neurol Med Chir (Tokyo), 2001,41(7):335.
doi: 10.2176/nmc.41.335 pmid: 11487996 |
| [1] | LI Jun,LIU Xu-hong,WANG Gong,CHENG Cheng,ZHUANG Hong-qing,YANG Rui-jie. Dosimetric effect of patient arm position on Cyberknife radiosurgery for spinal tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 182-186. |
| [2] | Duo YANG,Xin-na ZHOU,Shuo WANG,Xiao-li WANG,Yan-hua YUAN,Hua-bin YANG,Hui-zhen GENG,Bing PENG,Zi-bo LI,Bin LI,Jun REN. Assessment of lymphocytic function in vitro stimulated by specific tumor polypeptide combined with dendritic cells [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1094-1098. |
| [3] | Xue LOU,Li LIAO,Xing-jun LI,Nan WANG,Shuang LIU,Ruo-mei CUI,Jian XU. Methylation status and expression of TWEAK gene promoter region in peripheral blood of patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1020-1025. |
| [4] | Yu TIAN,Xiao-yue CHENG,Hui-ying HE,Guo-liang WANG,Lu-lin MA. Clinical and pathological features of renal cell carcinoma with urinary tract tumor thrombus: 6 cases report and literature review [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 928-932. |
| [5] | PANG Yong,ZHANG Sha,YANG Hua,ZHOU Rou-li. Serum LAPTM4B-35 protein as a novel diagnostic marker for hepatocellular carcinoma [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 710-715. |
| [6] | ZHAO Xun,YAN Ye,HUANG Xiao-juan,DONG Jing-han,LIU Zhuo,ZHANG Hong-xian,LIU Cheng,MA Lu-lin. Influence of deep invasive tumor thrombus on the surgical treatment and prognosis of patients with non-metastatic renal cell carcinoma complicated with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 665-670. |
| [7] | HONG Peng,TIAN Xiao-jun,ZHAO Xiao-yu,YANG Fei-long,LIU Zhuo,LU Min,ZHAO Lei,MA Lu-lin. Bilateral papillary renal cell carcinoma following kidney transplantation: A case report [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 811-813. |
| [8] | YANG Rong,LI Qing-xiang,WANG Yi-fei,ZHOU Wen,WANG Wen,GUO Chuan-bin,LIU Hao,GUO Yu-xing. Application of iodine staining technique for tumor identification in Micro-CT of mouse model with skull base-infratemporal fossa tumor [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 598-601. |
| [9] | ZHOU Chuan, MA Xue, XING Yun-kun, LI Lu-di, CHEN Jie, YAO Bi-yun, FU Juan-ling, ZHAO Peng. Exploratory screening of potential pan-cancer biomarkers based on The Cancer Genome Atlas database [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 602-607. |
| [10] | YANG Yang,XIAO Feng,WANG Jin,SONG Bo,LI Xi-hui,ZHANG Shi-jie,HE Zhi-song,ZHANG Huan,YIN Ling. One-stage surgery in patients with both cardiac and non-cardiac diseases [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 327-331. |
| [11] | Qi KANG,Ji-xin ZHANG,Ying GAO,Jun-qing ZHANG,Xiao-hui GUO. Analysis of diagnosis and treatment of 100 patients with Hürthle cell adenoma [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1098-1101. |
| [12] | Zu-nan TANG,Yuh SOH Hui,Lei-hao HU,Yao YU,Wen-bo ZHANG,Xin PENG. Application of mixed reality technique for the surgery of oral and maxillofacial tumors [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1124-1129. |
| [13] | Yong-wei HU,Rui LIU,Li LUO. Chronic multifocal osteomyelitis: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1140-1145. |
| [14] | Yi LIU,Zhi-jian LIU,Qi SHEN,Jing-yun WU,Yu FAN,De-run LI,Wei YU,Zhi-song HE. A clinical analysis of 14 cases of prostatic stromal tumor of uncertain malignant potential [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 621-624. |
| [15] | Hao WANG,Shu-kun JIANG,Ran PENG,Yi HUANG,Ming-qing WANG,Jun-jie WANG,Cheng LIU,Fan ZHANG,Lu-lin MA. Individual control of urine volume to improve stability of bladder volume in radiotherapy of urinary tumor [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 688-691. |