Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (3): 571-578. doi: 10.19723/j.issn.1671-167X.2019.03.029
Previous Articles Next Articles
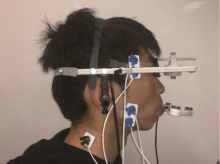
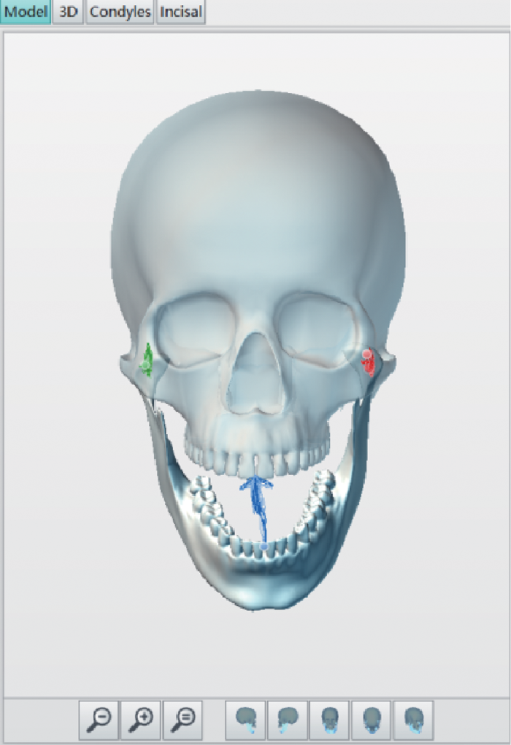
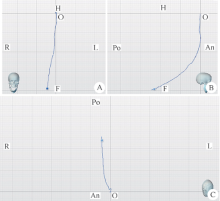
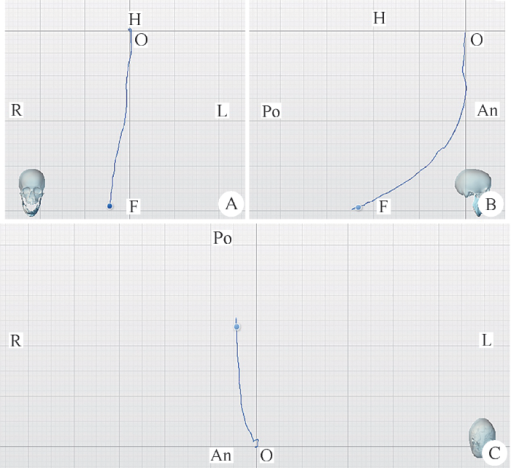
Application of digital mandibular movement record and masticatory muscle electromyography in the evaluation of stomatognathic function in patients with mandibular tumor
Jing WANG,Jun-peng CHEN,Yang WANG,Xiang-liang XU,Chuan-bin GUO△( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.13
| [1] | 袁道英, 杨佑成, 宋冰 . 下颌骨髁状突骨软骨瘤一例报告[J]. 中华肿瘤防治杂志, 2007,14(22):1759-1760. |
| [2] |
Krause I, Eisenstein B, Davidovits M , et al. Maxillomandibular brown tumor: a rare complication of chronic renal failure[J]. Pediatr Nephrol, 2000,14(6):499-501.
doi: 10.1007/s004670050803 |
| [3] |
Park SR, chung SM, Lim JY , et al. Giant cell tumor of the mandible[J]. Clin Exp Otorhinolaryngol, 2012,5(1):49-52.
doi: 10.3342/ceo.2012.5.1.49 |
| [4] | 徐保华, 史宗道 . 下颌髁突原发肿瘤:附12例报告[J]. 实用口腔医学杂志, 2001,17(3):249-250. |
| [5] |
Marunick MT, Mathog RH . Mastication in patients treated for head and neck cancer: a pilot study.[J]. J Prosthet Dent, 1990,63(5):566-573.
doi: 10.1016/0022-3913(90)90078-Q |
| [6] |
Hidalgo DA . Fibula free flap: a new method of mandible reconstruction[J]. Plast Reconstr Surg, 1989,84(1):71-79.
doi: 10.1097/00006534-198907000-00014 |
| [7] | Urken ML, Buchbinder D, Weinberg H , et al. Functional evaluation following microvascular oromandibular reconstruction of the oral cancer patient: a comparative study of reconstructed and nonreconstructed patients[J]. Laryngoscope, 1991,101(9):935-950. |
| [8] |
Lee R, Slevin N, Musgrove B , et al. Prediction of post-treatment trismus in head and neck cancer patients[J]. Br J Oral Maxillofac Surg, 2012,50(4):328-332.
doi: 10.1016/j.bjoms.2011.06.009 |
| [9] |
Kreeft AM, Krap M, Wismeijer D , et al. Oral function after maxillectomy and reconstruction with an obturator[J]. Int J Oral Max Surg, 2012,41(11):1387-1392.
doi: 10.1016/j.ijom.2012.07.014 |
| [10] |
Akashi M, Shibuya Y, Takahashi S , et al. Four-dimensional computed tomography evaluation of jaw movement following mandibular reconstruction: a pilot study[J]. J Cranio Maxill Surg, 2016,44(5):637-641.
doi: 10.1016/j.jcms.2016.01.027 |
| [11] | Haraguchi M, Mukohyama H, Reisberg DJ , et al. Electromyographic activity of masticatory muscles and mandibular movemet during function in marginal mandibulectomy patients[J]. J Med Dent Sci, 2003,50(4):257-264. |
| [12] |
Yen CI, Chou PY, Chen CH , et al. Kinematic, kinetic and surface electromyography analysis following zygomatic fracture reconstruction[J]. J Med Biol Eng, 2017,37(4):468-473.
doi: 10.1007/s40846-017-0271-z |
| [13] |
Ishida S, Shibuya Y, Kobayashi M , et al. Assessing stomatognathic performance after mandibulectomy according to the method of mandibular reconstruction[J]. Int J Oral Max Surg, 2015,44(8):948-955.
doi: 10.1016/j.ijom.2015.03.011 |
| [14] | 樊英显, 孙宏晨, 徐勇忠 . 颞下颔关节紊乱综合征患者咀嚼肌肌电分析[J]. 口腔医学研究, 1994(3):149-150. |
| [15] | Campillo B, Martín C, Palma JC , et al. Electromyographic activity of the jaw muscles and mandibular kinematics in young adults with theoretically ideal dental occlusion: reference values[J]. Med Oral Patol Oral Cir Bucal, 2017,22(3):e383-e391. |
| [16] | 黄超, 许向亮, 孙玉春 , 等. 下颌髁突功能面三维运动轨迹的初步推算和模拟[J]. 中华口腔医学杂志, 2018,53(10):669-673. |
| [1] | Mei-ge LIU,Pu FANG,Yan WANG,Lu CONG,Yang-yi FAN,Yuan YUAN,Yan XU,Jun ZHANG,Dao-jun HONG. Clinical, pathological and genetic characteristics of 8 patients with distal hereditary motor neuropathy [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 957-963. |
| [2] | FANG Shuo-bo,YANG Guang-ju,KANG Yan-feng,SUN Yu-chun,XIE Qiu-fei. Method and accuracy of determining the jaw position of repositioning splint with the aid of digital technique [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 76-82. |
| [3] | Guo-zhong LIN,Zhen-yu WANG,Jing-cheng XIE,Bin LIU,Chang-cheng MA,Xiao-dong CHEN. Clinical study of 21 cases of sacral cysts containing fila terminale [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 582-585. |
| [4] | Shu-dong YAN,Guang-ju YANG,Si-yi MO,Yun LIU,Qiu-fei XIE. Effect of long-term resistance exercise on masseter muscle mechanical hyperalgesia in rats [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 21-27. |
| [5] | LIU Cun-rui, XU Xiao-xiang, CAO Ye, XIE Qiu-fei. Influence of the occlusal interference time on masticatory muscle mechanical hyperalgesia in rats [J]. Journal of Peking University(Health Sciences), 2016, 48(1): 51-56. |
|