Journal of Peking University(Health Sciences) ›› 2020, Vol. 52 ›› Issue (1): 83-89. doi: 10.19723/j.issn.1671-167X.2020.01.013
Previous Articles Next Articles
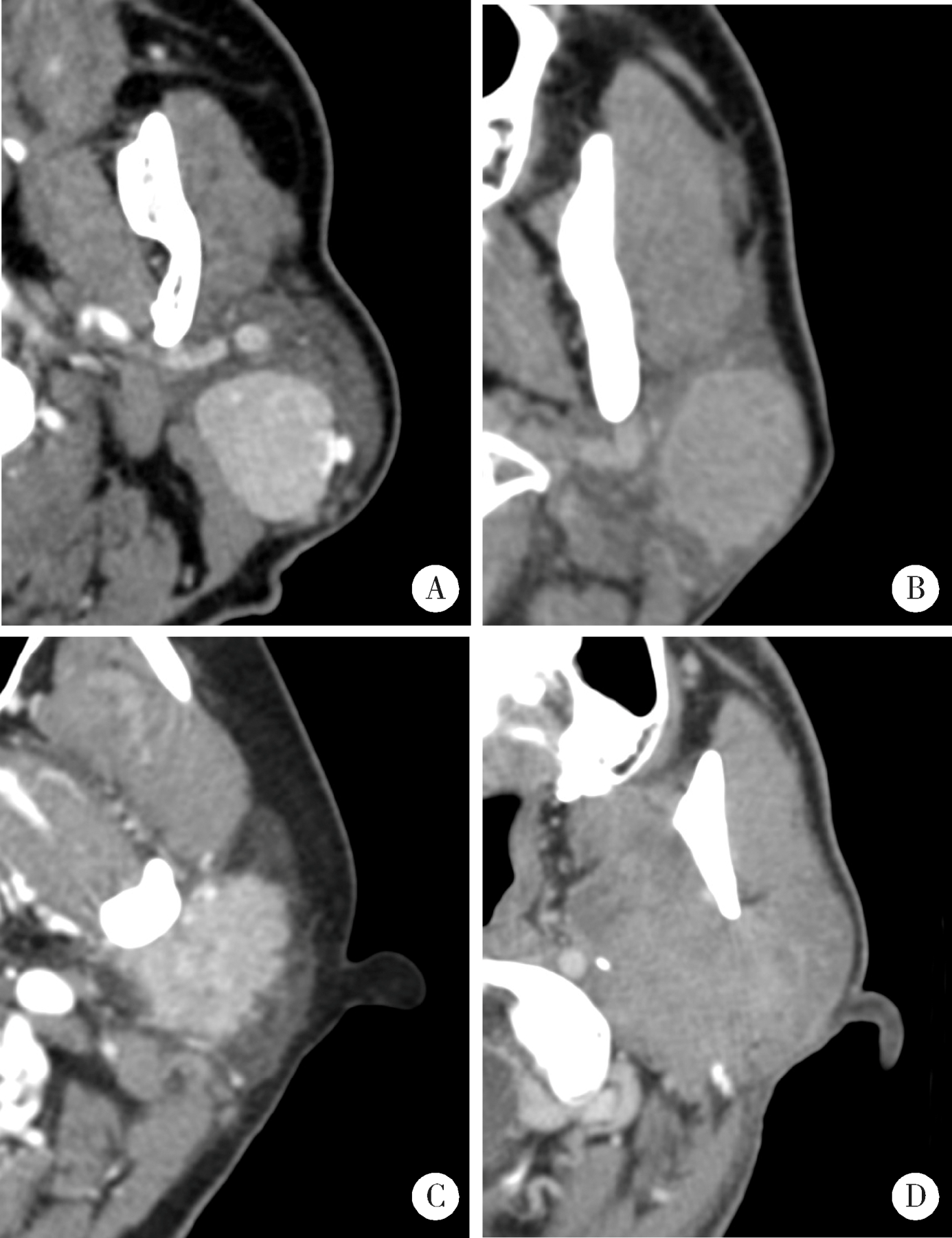
Parotid CT imaging reporting and data system: A preliminary study
Yu-bing LI1,Li-sha SUN2,Zhi-peng SUN1,△( ),Xiao-yan XIE1,Jian-yun ZHANG3,Zu-yan ZHANG1,Yan-ping ZHAO1,Xu-chen MA1
),Xiao-yan XIE1,Jian-yun ZHANG3,Zu-yan ZHANG1,Yan-ping ZHAO1,Xu-chen MA1
- 1. Department of Oral Pathology, Peking University School and Hospital of Stomatology & Department of Oral and Maxillofacial Radiology, Beijing 100081, China
2. Department of Oral Pathology, Peking University School and Hospital of Stomatology & Central Laboratory, Beijing 100081, China
3. Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R739.87
| [1] | 张震康, 俞光岩 . 口腔颌面外科学[M]. 2版. 北京: 北京大学医学出版社, 2013. |
| [2] | Abdullah A, Rivas FF, Srinivasan A . Imaging of the salivary glands[J]. Semin Roentgenol, 2013,48(1):65-74. |
| [3] | 俞光岩, 高岩, 孙勇刚 . 口腔颌面部肿瘤[M]. 北京: 人民卫生出版社, 2002. |
| [4] | Seethala RR, Stenman G . Update from the 4th edition of the World Health Organization classification of head and neck tumours: Tumors of the salivary gland[J]. Head Neck Pathol, 2017,11(1):55-67. |
| [5] | White SC, Pharoah MJ . Oral radiology principles and interpretation[M]. 3rd ed. St. Louis, Missouri: Mosby Elsevier, 2014. |
| [6] | 马绪臣 . 口腔颌面医学影像学[M]. 北京: 北京大学医学出版社, 2014. |
| [7] | 马绪臣, 李铁军 . 口腔颌面部疾病CT诊断与鉴别诊断[M]. 北京: 北京大学医学出版社, 2019. |
| [8] | Horvath E, Majlis S, Rossi R , et al. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical ma-nagement[J]. J Clin Endocrinol Metab, 2009,94(5):1748-1751. |
| [9] | Barentsz JO, Richenberg J, Clements R , et al. ESUR prostate MR guidelines 2012[J]. Eur Radiol, 2012,22(4):746-757. |
| [10] | Abdel Razek AA, Ashmalla GA, Gaballa G , et al. Pilot study of ultrasound parotid imaging reporting and data system (PIRADS): Inter-observer agreement[J]. Eur J Radiol, 2015,84(12):2533-2538. |
| [11] | 马大权, 俞光岩 . 唾液腺病学[M]. 2版. 北京: 人民卫生出版社, 2014. |
| [12] | Kim H, Kim SY, Kim YJ , et al. Correlation between computed tomography imaging and histopathology in pleomorphic adenoma of parotid gland[J]. Auris Nasus Larynx, 2018,45(4):783-790. |
| [13] | Ito FA, Jorge J, Vargas PA , et al. Histopathological findings of pleomorphic adenomas of the salivary glands[J]. Med Oral Patol Oral Cir Bucal, 2009,14(2):E57-61. |
| [14] | 黄敏娴, 马大权, 俞光岩 , 等. 复发性涎腺多形性腺瘤的临床与病理分析[J]. 现代口腔医学杂志, 2008,22(1):1-4. |
| [1] | Guang-yan MENG,Yun-xiao ZHANG,Yu-xin ZHANG,Yan-ying LIU. Clinical characteristics of central nervous system involvement in IgG4 related diseases [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1043-1048. |
| [2] | Li ZHAI,Nan QIU,Hui SONG. Multicentric reticulohistiocytosis: A case report [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1183-1187. |
| [3] | Gang YANG,Wen-jie HU,Jie CAO,Deng-gao LIU. Three-dimensional morphology analysis of the supraosseous gingival profile of periodontally healthy maxillary anterior teeth [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 990-994. |
| [4] | LI Xin-fei, PENG Yi-ji, YU Xiao-teng, XIONG Sheng-wei, CHENG Si-da, DING Guang-pu, YANG Kun-lin, TANG Qi, MI Yue, WU Jing-yun, ZHANG Peng, XIE Jia-xin, HAO Han, WANG He, QIU Jian-xing, YANG Jian, LI Xue-song, ZHOU Li-qun. Three dimensional nephrometry system for partial nephrectomy: Our initial exploration [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 613-622. |
| [5] | LIAO Xu-he,WANG Rong-fu,LIU Meng,CHEN Xue-qi,XIONG Yan,NONG Lin,YIN Lei,ZHANG Bing-ye,DU Yu-jing. Semiquantitative parameters of 18F-FDG PET/CT, gene mutation states of epidermal growth factor receptor and anaplastic lymphoma kinase in prognosis evaluation of patients with lung adenocarcinoma [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 246-254. |
| [6] | MENG Yuan,ZHANG Li-qi,ZHAO Ya-ning,LIU Deng-gao,ZHANG Zu-yan,GAO Yan. Three-dimentional radiographic features of 67 maxillary radicular cysts [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 396-401. |
| [7] | ZHOU Jing,LIU Yi. Cone-beam CT evaluation of temporomandibular joint in skeletal class Ⅱ female adolescents with different vertical patterns [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 109-119. |
| [8] | GAO Lu,GU Yan. Chinese morphological stages of midpalatal suture and its correlation with Demirjian dental age [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 133-138. |
| [9] | YUAN Yuan,LANG Ning,YUAN Hui-shu. CT spectral curve in differentiating spinal tumor metastasis and infections [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 183-187. |
| [10] | LI Peng,PIAO Mu-zi,HU Hong-cheng,WANG Yong,ZHAO Yi-jiao,SHEN Xiao-jing. Radiography study on osteotome sinus floor elevation with placed implant simultaneously with no graft augmentation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 95-101. |
| [11] | Qi KANG,Ji-xin ZHANG,Ying GAO,Jun-qing ZHANG,Xiao-hui GUO. Analysis of diagnosis and treatment of 100 patients with Hürthle cell adenoma [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1098-1101. |
| [12] | Gong CHENG,Xia ZHANG,Fei YANG,Jia-yu CHENG,Yan-ying LIU. Angioimmunoblastic T-cell lymphoma with fever, arthritis and skin pigmentation: A case report [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1150-1152. |
| [13] | Shuang HU,Li-ping YANG. Expression pattern of different serotypes of adeno-associated viral vectors in mouse retina [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 845-850. |
| [14] | Cai-nan LUO,Zheng-fang LI,Li-jun WU,Hai-juan CHEN,Chun-mei YANG,Wen-hui XU,Xiao-ling LIU,Wei TANG,Ping QIAO,Baihetiya Rena. Multicenter performance of the different classification criteria for rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 897-901. |
| [15] | Huan-bin YU,Wen-jie WU,Xiao-ming LV,Yan SHI,Lei ZHENG,Jian-guo ZHANG. 125I seed brachytherapy for recurrent salivary gland carcinoma after external radiotherapy [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 919-923. |