SUMMARY Tooth eruption is defined as the movement of a tooth from its site of development within the alveolar process to its functional position in the oral cavity. The process of tooth eruption can be divided into different phases: pre-eruptive bone stage alveolar bone stage mucosal stage preocclusal stage occlusal stage and maturation stage. Any disturbance in these phases can lead to eruptive anomalies. The incidence of unerupted teeth is usually higher among permanent teeth than among deciduous ones. Of the primary teeth reported as unerupted second deciduous molars are the teeth most frequently involved followed by primary central incisors. At present almost no coverage is seen about the impaction of the first deciduous molar. In this case a 4-year-old boy who presented with an impacted left maxillary first deci-duous molar came to the Department of Pediatric Dentistry Peking University School and Hospital of Stomatology. This tooth located higher to the left maxillary first premolar was well near to the maxillary sinus. The family and medical histories were noncontributory and his physical findings were within normal limits. The mother was reported as having experienced no illness or other complications and taken no medications during pregnancy. His clinical extraoral examination was noncontributory. His clinical intra-oral examination revealed that the maxillary left first primary molar was not present. No enlargement of the area was apparent visually or on palpation. The remaining primary dentition was well aligned and in good condition. His oral hygiene was good although there were incipient occlusal carious lesions in the mandibular second primary molars. There was no history or evidence of dental trauma. A diagnosis of a left maxillary first deciduous molar was made on the basis of the clinical and radiographic evidence. Numerous local etiologic factors have been described for impacted teeth. These include anomalous teeth malposition fusion with adjacent or supernumerary teeth odontoma dentigerous cysts tumors underdevelopment of the jaws keratinized epithelial lining hereditary conditions and trauma. In this case the reason for impaction was not clear. After the comprehensive clinical evaluation treatment consisted of placement of a space maintainer the periodic examination was indicated for the follow-up so that early interventions such as subsequent surgical intervention and orthodontic traction could be recommended timely to manage orofacial disfigurement and to avoid consequent problems with resultant proper functioning and good periodontal health.
牙阻生(impaction of teeth)是指超过了应该正常完全萌出的时间, 牙仍在颌骨内未萌出或者仅部分萌出。阻生可以是一颗牙或者数颗牙受累, 常对称性发生。牙阻生常见于恒牙列, 最常累及第三磨牙、下颌前磨牙和上颌尖牙, 乳牙列罕见[1, 2, 3, 4]。在乳牙阻生的报道中, 多为下颌第二乳磨牙阻生, 上颌第二乳磨牙少见[2, 3, 4, 5, 6, 7]。上颌第一乳磨牙及其继承恒牙易位埋伏阻生更为罕见, 本研究报道1例上颌第一乳磨牙与第一前磨牙异位埋伏阻生的患者, 对该病的发病机制和治疗进行探讨。
患者, 男, 2012年3月出生, 2016年8月因左侧上颌有一颗牙齿一直未萌出到北京大学口腔医院第三门诊部儿科就诊。患儿为足月剖宫产, 无重大疾病史, 无外伤、感染史。父母非近亲结婚, 母亲孕期无损伤、感染、服药史。家族中未见牙齿阻生。患者一般情况良好, 营养中等, 身高、体重正常。
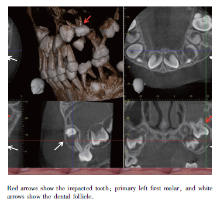
临床检查:面部发育正常, 面型左右对称; 口腔检查(图1):64缺失, 间隙无明显丧失, 牙槽嵴未见明显膨隆, 未扪及膨出物。其他乳牙正常萌出且排列正常, 口腔卫生情况良好, 口内没有龋坏牙齿, 没有牙齿外伤史及外伤迹象。通过全景曲面体层片(图2)观察患儿口腔整体发育情况, 除64外, 其余影像学表现与4岁正常发育男孩应有的影像学表现相符。64高位阻生, 位于继承恒牙胚24的左上方, 牙根已经发育完成, 根尖与窦底影像重叠, 未见明显的根周膜间隙, 提示牙骨粘连。锥形束CT(cone-beam computed tomography, CBCT)显示(图3):64牙根发育完成, 埋伏阻生于24牙胚根方, 牙囊影像增宽, 对应上颌窦底壁受压上抬, 上颌窦底壁尚连续, 左侧上颌窦腔内密度弥漫性增高, 气腔明显缩小, 提示上颌窦炎症可能, 24牙胚发育6期, 余未见异常高密度团块状影像。
 | 图1 口内上颌牙合面相, 左侧上颌第一乳磨牙未萌出Figure 1 Intraoral view of maxillary arch with primary left first molar unerupted |
与外科医师及正畸科医师会诊, 针对乳牙阻生存在的主要问题, 共识如下:(1)患儿年龄小, 无明显不适症状, 未发现牙囊组织生长发育方面的异常及对周围组织的不良影响, 又考虑到阻生牙齿的位置, 目前不宜拔除阻生齿; (2)对于该患儿应制作间隙保持器以维持间隙(图4), 预防因间隙丧失而引起的错牙合畸形等问题, 并且建议患儿家长带患儿于耳鼻喉科就诊, 治疗上颌窦疾病; (3)需要定期检查, 长期随访, 若出现牙囊不断膨大甚至引起颌骨膨大, 或者恒牙胚发育受到不良影响, 或者冠周纤维组织异常增生等, 应及时采取相应的治疗措施, 手术拔除阻生齿, 尽可能地避免后续颌面部发育畸形等的发生。
牙的萌出(eruption)是指牙突破口腔黏膜的现象, 而实际上牙萌出是牙冠形成后向牙合平面移动, 穿过骨隐窝和口腔黏膜, 达到功能位置的一个复杂过程, 这个过程可以被分为不同的时期, 包括萌出前期、牙槽骨期、牙槽黏膜期、咬合建立前期、咬合建立期和成熟期[8], 在这些阶段中有任何的干扰都可能导致萌出异常。
牙阻生常见于恒牙列, 最常累及的牙是第三磨牙、下颌前磨牙和上颌尖牙, 乳牙列罕见[1, 2, 3, 4]。在乳牙阻生的报道中, 多为下颌第二乳磨牙阻生, 上颌第二乳磨牙少见[2, 3, 4, 5, 6, 7], 上颌第一乳磨牙及其继承恒牙易位埋伏阻生更为罕见。
目前, 乳牙阻生准确的病因尚不明确, 既往研究其主要的相关因素是牙骨粘连, 这很可能与创伤或者感染有关[8, 9, 10, 11, 12, 13]。本病例通过影像学检查观察到患儿就诊期间存在上颌窦炎症, 但其与乳牙阻生之间的因果关系并不明确。一些研究支持在发育中萌出异常具有家族聚集性这一假说, 然而本病例患者家族中未发现类似现象, 其他可能引起乳牙阻生的因素包括牙瘤[2, 3, 14, 15]、冠周纤维组织异常增生、成釉细胞纤维瘤和含牙囊肿[3, 7]等。含牙囊肿又称滤泡囊肿, 是指包含一个未萌牙齿的牙冠并且附着于该牙牙颈部的囊肿, 是由于牙冠与缩余釉上皮之间积聚囊液而成, 本病例CBCT中观察到埋伏牙牙囊影像增宽, 不排除发展成含牙囊肿的可能, 需进一步观察其变化情况。
这类病例治疗方案的制定, 多为手术拔除阻生齿及相关异常组织, 如含牙囊肿、牙瘤等, 并进一步进行正畸治疗, 因为大多数的病例发现于5岁以上患儿, 已经出现了一些口颌畸形问题或者有明确的牙瘤或囊肿的存在[7, 8, 14, 16], 学者们认为这类病例治疗方案的制定需要考虑以下两点问题, 一是是否存在牙囊组织生长发育方面的异常, 如牙源性肿瘤、囊肿; 二是是否对周围组织有破坏, 如颌骨膨隆, 存在牙周袋, 使邻牙无法萌出, 位置不正或者妨碍正畸治疗等[4, 5, 7, 8, 14, 16, 17]。
本例患儿没有明显的不适症状, 阻生牙齿目前未见对周围组织产生破坏, 暂不具备拔除阻生齿的指征, 另外, 阻生齿位置较高, 紧邻上颌窦底壁, 阻生齿附近的恒牙胚还处于发育早期, 若手术拔除阻生齿, 引起上颌窦漏及恒牙胚受损的可能性较大。
研究显示乳牙的萌出异常常与恒牙的萌出异常及牙列发育异常相关[18], 所以本病例需要定期检查, 长期随访, 以及时采取相应的治疗措施, 尽可能地避免后续颌面部发育畸形等地发生。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|