目的 评估颈基底型股骨粗隆部骨折的特点和发生率,探究其诊断及治疗方式。方法 选择北京大学第三医院骨科2005年1月至2016年5月收治的832例粗隆部骨折病例,其中28例(3.37%)为颈基底型骨折患者,对其进行回顾性分析,分别采用空心钉、动力髋螺钉(dynamic hip screw,DHS)、髓内钉固定系统3种内固定方法治疗,记录手术时间、术中出血量、隐性失血量、围术期失血总量、术后住院日、骨折愈合时间、Harris评分等数据并进行比较。结果 髓内钉组16例,手术时间为55(20,120) min,术后平均住院日3(2,7) d,术中出血量为50(5,100) mL,隐性失血量为533.37(376.19,987.15) mL,失血总量为627.35(406.19,1037.16) mL,骨折平均愈合时间及最终Harris评分分别为6(3,9) 个月 和90.25(74,100)分;DHS组8例,手术时间为87.5(65,115) min,术后住院日5.5(2,17) d,术中出血量为100(50,300) mL,隐性失血量为278.11(202.43,849.97) mL,失血总量为580.19(368.55,899.97) mL,骨折平均愈合时间及最终Harris评分分别为5.5(4,12)个月和85.5(84,87)分;空心钉组4例,手术时间为47.5(35,75) min,术后住院日5(2,12) d,术中出血量为20(2,70) mL,隐性失血量为150(100.00,412.01) mL,失血总量为195.00(120.00,414.01) mL,骨折平均愈合时间及最终Harris评分分别为4(4,6)个月和80(61,97)分。髓内钉组和空心钉组手术时间明显少于DHS组,但前两组间差异无统计学意义( P=0.367)。3组患者术后住院日差异无统计学意义( P=0.053)。DHS组术中出血量明显高于另两组,而髓内钉组和空心钉组术中出血量差异无统计学意义( P=0.100)。隐性失血量髓内钉组显著增多,另两组间差异无统计学意义( P=0.134)。围术期失血总量空心钉组与其他两组比较相对较少,髓内钉组与DHS组差异无统计学意义( P=0.483)。患者平均随访时间4.74年(1~10年),采用空心钉治疗的一名患者术后3个月出现内固定失败。3组患者平均骨折愈合时间及最终随访时Harris评分差异无统计学意义( P>0.05)。结论 颈基底型骨折的发生率较低,无移位骨折患者可通过术前X线片确诊,对于骨折移位患者,建议完善术前CT+三维重建以确诊;闭合复位手术内固定治疗应作为首选治疗方式;采用DHS或髓内固定系统治疗效果较好。
Objective: To evaluate the rate of basicervical fractures and document their diagnosis and treatment.Methods: From January 2005 to May 2016, 28 basicervical fractures of the 832 trochanteric fractures were collected and evaluated. The patients were treated with multiple screws, dynamic hip screw (DHS), intramedullary nail. Via the operation time, postoperative hospitalization, loss of blood duration the operation, hidden blood loss, total blood loss, mean union time and the final follow-up Harris hip score, the characteristics of different internal fixations were compared and analyzed.Results: The incidence of basicervical fractures was 3.37% (28/832) in our study. In the intramedullary nail group (16 patients), the operation time was 55 (20,120) min, the postoperative hospitalization was 3(2, 7) d, the intraoperative blood loss was 50(5,100) mL, the hidden blood loss was 533.37 (376.19, 987.15) mL, and the total blood loss 627.35 (406.19, 1037.16) mL . The union time and final follow-up Harris score were 6 (3, 9) months and 90.25 (74,100) min. In the DHS group (8 patients), the operation time was 87.5 (65,115) min, the postoperative hospitalization was 5.5 (2, 17) d, the intraoperative blood loss was 100 (50,300) mL, the hidden blood loss was 278.11 (202.43, 849.97) mL, and the total blood loss 580.19 (368.55, 899.97) mL . The union time and final follow-up Harris score were 5.5 (4, 12) months and 85.5 (84, 87) min. In the multiple screws group (4 patients), the operation time was 47.5 (35, 75) min, the postoperative hospitalization was 5 (2, 12) d, the intraope-rative blood loss was 20 (2, 70) mL, the hidden blood loss was 150 (100.00, 412.01) mL, and the total blood loss 195.00 (120.00, 414.01) mL. The union time and final follow-up Harris score were 4 (4, 6) months and 80 (61, 97) min. The patients treated with multiple screws and intramedullary nail had a shorter operation time than the DNS group, but no obvious difference was found between the other two groups ( P=0.367). Postoperative hospitalization had no significant difference among the three groups. The intraoperative bleeding was more in the DHS group, the other two groups had no significant difference ( P=0.100). However, the hidden blood loss was more in the intramedullary nail group, the other two groups had no significant difference ( P=0.134). The total blood loss in the intramedullary nail group was more than multiple screw group, similar to the DHS group ( P=0.483). One patient treated with multiple screws underwent internal fixation failure three months after operation. The mean union time and final follow-up Harris scores had no significant difference among the three groups ( P>0.05).Conclusion: Through this study, we found that the incidence of basicervical fractures is low. Fractures with no shift can be confirmed by preoperative X-ray. For displaced fractures, preoperative CT + 3D reconstruction is recommended. Surgical treatment by closed reduction and internal fixation with DHS or intramedullary nail is shown to be very effective.
颈基底型粗隆部骨折较为少见, 其骨折线恰好位于股骨颈和粗隆区的交界线, 即转子间线[1], 是一种介于股骨颈骨折和股骨粗隆间骨折的特殊类型, 既往研究表明颈基底型骨折占股骨近端骨折的1.8%~3.3%[2, 3], 根据其骨折线的位置, 颈基底型骨折属于囊外骨折[4], 在目前常用的股骨近端骨折分型系统中, 没有将其列为单独的一种骨折类型。关于颈基底型骨折的治疗方式, 目前尚没有定论[1, 2, 5]。本研究回顾性分析2005年1月至2016年5月北京大学第三医院骨科收治的颈基底型骨折患者病例资料, 旨在评估颈基底型粗隆部骨折的特点及发生率, 并探究其诊断及治疗方式。
选择2005年1月至2016年6月北京大学第三医院骨科收治的股骨粗隆部骨折行内固定治疗患者共832例, 严格按照颈基底型骨折定义, 通过患者术前的髋部正侧位X线片、术前髋部CT+三维重建或术后髋部X线片, 找出颈基底型骨折患者, 如果患者骨折线向粗隆部或者股骨颈延伸, 则按非颈基底型骨折处理, 初次筛选病例共55例, 对55例患者全部进行第2次评估, 确保所有入选病例严格符合颈基底型骨折的定义, 二次评估分为无移位组41例和移位组14例。无移位组中, 通过术前X线片确诊粗隆间骨折19例及颈基底型骨折18例, 结合术前CT/术后X线片确诊粗隆间骨折1例和颈基底型骨折3例。有移位组中, 通过术前X线片确诊粗隆间骨折2例, 结合术前CT/术后X线片确诊粗隆间骨折5例, 颈基底型骨折7例。无移位组通过X线确诊37例(颈基底型18例+粗隆间骨折19例), 有移位组通过术前CT/术后X线确诊12例(颈基底型7例+粗隆间骨折5例), 经卡方检验P< 0.01(表1), 即骨折无移位患者多数可通过术前X线确诊, 对于骨折移位患者需结合术前CT/术后X线检查以确诊。二次评估后确诊颈基底型骨折28例, 占股骨近端粗隆部骨折的 3.37%(28/832)。
| 表1 二次评估确诊方法比较 Table 1 Diagnosis method comparison in the second evaluation |
将28位患者分为3组, 采用髓内钉(Gamma 3或PFNA、PFNA2)固定16例(Ⅰ 组), 采用动力髋螺钉(dynamic hip screw, DHS)固定8例(Ⅱ 组), 采用3枚空心钉固定4例(Ⅲ 组)。28例患者男11例, 女17例, 全部为低能量损伤, Ⅰ ~Ⅲ 组患者平均年龄分别为67.56岁(52~89岁)、73.36岁(49~87岁)和63.25岁(39~74岁); 术前合并心脑血管疾病、肾功能不全等严重合并症分别为3例、1例和1例, 合并高血压、糖尿病的患者分别为4例、2例和1例。
麻醉满意后, 患者仰卧于可透X线牵引床上, 行闭合牵引复位, 全部患者均闭合复位成功。髓内钉组及动力髋螺钉组(DHS组)分别按照标准的操作流程, DHS使用2~4孔板, 空心钉组采用股骨外侧小切口, 呈三角形打入3枚空心钉[6], 记录从切皮开始到切口缝合完毕的手术时间及术中失血量。
计算3组患者围术期失血量, 应用Gross方程[7]计算红细胞的容量, 进一步计算3组患者围手术期失血量及隐性失血量。测量患者身高(m)、体重(kg)、术前及术后红细胞压积(hematocrit, HCT), 通过Nadler等[8]方法计算患者术前血容量(patient blood volume, PBV), PBV=k1× h3+k2× w+k3, 其中h为身高, w为体重(体质量), k为常数, 男性 k1=0.3669, k2=0.03219, k3=0.6041, 女性k1=0.3561, k2=0.0331, k3=0.1833。总红细胞丢失量=术前PBV× (HCT术前-HCT术后), 失血总量=总红细胞丢失量/HCT术前。失血总量+输血量=隐性失血量+显性失血量, 显性失血量=术中出血量+术后引流量[9]。
记录3组病例的一般资料, 平均手术时间、术后平均住院日、术中平均出血量、隐性失血量、失血总量、平均骨折愈合时间及Harris评分, 进而比较不同内固定方式的优缺点。
所有数据均采用SPSS 23.0软件分析, 计量性资料以M(min, max)表示, 3组数据之间以秩和检验进行统计学分析(Kruskal-Wallis H检验), P< 0.05认为差异有统计学意义。
分析3组患者基本资料, 发现年龄、性别、身高、体重、伤侧等, 差异均无统计学意义(P> 0.05)。3组患者平均手术时间、术后平均住院日、术中平均出血量、隐性失血量、失血总量统计见表2, Ⅱ 组术后出现右侧股总静脉、股浅静脉血栓1例, Ⅲ 组术后发生心律失常1例。
| 表2 不同内固定方式比较 Table 2 Internal fixation method comparison |
对3组数据进行统计学分析, 髓内钉组和空心钉组手术时间明显少于DHS组, 但差异无统计学意义(P=0.367); 3组患者术后住院日差异无统计学意义(P=0.053); DHS组术中出血量明显高于另两组, 而髓内钉组和空心钉组术中出血量差异无统计学意义(P=0.100); 隐性失血量髓内钉组显著增多, 另两组差异无统计学意义(P=0.134); 围术期失血总量空心钉组与其他两组比较相对较少, 髓内钉组与DHS组差异无统计学意义(P=0.483)。
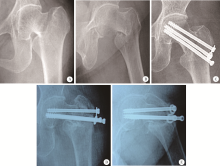
28例患者获得随访23例, 随访率为82.1%, Ⅰ 组13例, Ⅱ 组6例, Ⅲ 组4例。平均随访时间为4.74年(1~10年)。Ⅲ 组1例患者术后3个月发现内固定失败(图1), 其余患者均未见内固定物失败、断钉等现象, 未见股骨头坏死并发症。3组骨折预后见表3, 3组患者平均骨折愈合时间及最终随访时Harris评分差异无统计学意义(P> 0.05)。
| 表3 不同内固定方式预后比较 Table 3 Prognosis comparison of the three internal fixation methods |
颈基底型粗隆部骨折是介于股骨颈和粗隆间骨折之间的一种特殊骨折类型。与股骨颈基底型骨折不同, 其骨折线不累及股骨颈侧[10], Blair等[1]强调其骨折线恰好位于股骨颈与粗隆交界处。颈基底型骨折属于囊外骨折, 常发生于老年人, 多由低能量损伤所致, 其发生率较低, 大约占股骨近端骨折的1.8%~3.3%[2, 3]。本研究颈基底型骨折占股骨近端粗隆部骨折的3.37%(28/832), 平均年龄68.61岁(28~89岁)。
Saarenpä ä 等[2]分析1 624例病例, 通过X线两次筛选, 第1次共筛选出108例, 通过第2次严格筛查最终确诊30例(排除股骨颈骨折51例+粗隆间骨折27例), 可见单纯通过术前X线片诊断颈基底型骨折存在困难, 主要原因为股骨近端前后位X线片中, 颈基底型骨折的骨折线容易显示不清。 Saarenpä ä 等[2]的研究中2/3的错误分类是由于术前X线骨折线显示不清造成的, 研究发现, 对于骨折无移位患者, 可通过术前X线确诊。本研究颈基底型骨折无移位患者中, 85.7%患者(18/21)可通过术前X线确诊。对于骨折移位患者, 需结合术前CT诊断以确诊, 本研究7例骨折移位患者均需要术前CT或术后X线确诊。
颈基底型骨折作为一种囊外骨折, 对股骨头血运影响较小, 近端骨折块无肌肉附着, 生物力学特性与粗隆间骨折相似, 存在轴向和旋转的不稳定[11]。目前的研究多推荐颈基底型骨折治疗应参考粗隆间骨折, 采用内固定治疗[12, 13, 14, 15, 16], 但内固定方式尚无统一观点。Chen等[3]分析了8 079例股骨近端骨折病例, 其中269例(3.3%)颈基底型骨折患者均采用DHS治疗, 取得较好效果。Tasyikan 等[17]采用髓内钉治疗28例颈基底型骨折患者, 均取得较好效果。
本研究采用3枚空心钉作为内固定方法之一, 手术时间、术中出血量、隐性失血量及围术期失血总量较其他两组低。髓内钉组平均手术时间及术后平均住院日均优于DHS组, 虽然髓内钉组术中显性失血量较少, 但围术期隐性失血量较多, 两组失血总量无明显差别。两组患者隐性失血量分别占失血总量的90.61%和63.72%, 可见采用髓内钉作为内固定时, 存在大量隐性出血, 考虑可能与髓内固定开放髓腔、扩髓有关[9]。
本研究3组患者骨折平均愈合时间及最终的Harris评分无明显差异, 但是空心钉治疗颈基底型骨折的稳定程度有待考证, 本研究唯一1例内固定失败病例为采用3枚空心钉固定患者。2002年Saarenpä ä 等[2]使用空心钉治疗7例颈基底型骨折患者, 其中3例术后发生内固定失败。Blair等[1]进行体外生物力学研究发现, 空心钉固定后股骨近端轴向负荷能力较DHS差, 因为颈基底型骨折近侧骨折块有内翻的趋势, 多枚空心钉固定时, 由于缺乏股骨颈的对抗, 导致股骨外侧的入点应力较大, 易出现空心钉固定失败。采用DHS加空心钉固定或髓内钉治疗均可取得较好效果(图2), 两者在骨折预后上无明显差异, 此结果与既往研究相符[2, 18, 19]。
本研究颈基底型骨折的术后并发症发生率较低, 其中未见股骨头缺血坏死病例, 而粗隆部骨折股骨头缺血坏死的发生率约为0.3%~0.5%[20, 21, 22], 但有研究提示该骨折术后出现并发症及需要再次手术的概率较高[2, 11, 23]。笔者认为, 关于该骨折并发症发生率需更多病例资料分析。
综上所述, 颈基底型粗隆部骨折发生率较低, 常发生于老年人, 多由低能量损伤所致, 多数患者骨折无移位。无移位患者大多可通过术前X线片确诊, 对于骨折移位的患者, 建议完善术前CT+三维重建以确定诊断。治疗颈基底型骨折, 应采用闭合复位内固定治疗。髓内钉或DHS加空心钉固定均可获得良好效果, 不推荐单纯空心钉固定, 尽管3枚空心钉固定具有创伤小、出血少等优势, 但是其生物力学稳定性较差, 失败率高。
(本文编辑:王 蕾)
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|