There exist controversies in the surgical treatment of maisonneuve injury with regard to reduction and fixation of syndesmosis and management of proximal fibular fracture. It is very important for the orthopaedic surgeons to learn more techniques and avoid pitfalls from clinical practice. We summarized the clinical data of 1 failed case, a 20-year-old girl with big body weight who underwent a primary surgery for the treatment of maisonneuve fracture with minimally invasive reduction and fixation of ankle syndesmosis and posterior malleolus and open reduction and internal fixation of medial malleolus, then a revision surgery for the treatment of iatrogenic syndesmotic malreduction with open reduction and re-stabilization of ankle syndesmosis supplemented with open reduction and internal fixation of proximal fibular facture. The malreduction of distal fibula was not found until finishing the postoperative computed tomography (CT) scan 2 weeks after the primary surgery, then the patient experienced an revision surgery including removal of the screws installed primarily for fixation of ankle syndesmosis, and open reduction and internal fixation of proximal fibular fracture, and limited open reduction and re-stabilization of ankle syndesmosis. Then the patient rehabilitated regularly under the direction of the surgeon who performed these two operations, and the postoperative recovery was smooth, then the hardwares for fixation of ankle syndesmosis and fracture of proximal fibula and medial malleolus were removed at different postoperative time. The patient experienced an excellent outcome at the end of the 3-year follow-up. The reasons for the failure in this case might include the overemphasized minimally invasive technique in the process of reduction, inaccurate assessment of intraoperative fluoroscopy and postoperative radiographs, and inappropriate utilization of the reduction clamp. Attention should be paid to the fact that an obliquely placed clamp for closed reduction of diastasis of ankle syndesmosis could result in syndesmotic malreduction. The worsened alignment of the fracture end of proximal fibula observed by intraoperative fluoroscopy may alert surgeons to syndesmotic malreduction. Partial exposure of syndesmosis and anatomical reduction and fixation of proximal fibular fracture may be useful measurres to avoid malreduction of ankle syndesmosis in the surgical treatment of maisonneuve injury in some patient, especially the patient with critically destabilized ankle.
Maisonneuve损伤因涉及下胫腓联合韧带的损伤及腓骨近端骨折, 易造成踝关节对合关系及稳定性改变, 往往需要手术治疗, 手术虽不复杂却存在严重失误的风险。本文通过总结1例Maisonneuve损伤手术治疗失败的病例资料, 提醒医生在对该损伤进行手术治疗时注意避免类似的失误。
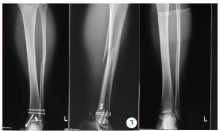
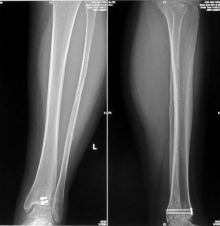
患者, 女, 20岁, 骑车倒地致踝部扭伤后12 h入院, 体格检查显示踝部及小腿肿胀明显, 压痛, 皮肤完整, 末端血液循环正常, 影像学检查显示腓骨近端骨折移位、下胫腓联合分离、内踝骨折移位、后踝骨折、距骨脱位(图1), CT图像显示下胫腓联合分离, 腓骨远端向后移位(图2)。
经完善术前准备, 于伤后24 h安排手术治疗。手术在全身麻醉下进行, 于踝关节外侧沿腓骨远端微创切口, 显露腓骨外侧骨皮质后使用复位钳内外方向挤压胫腓骨, 术中影像显示踝穴宽度恢复, 维持复位, 经腓骨远端切口安装2枚螺钉维持复位, 内踝处弧形切口显露内踝, 复位后使用2枚空心拉力螺钉固定, 踝关节前方切口, 显露胫骨远端, 透视下自前向后安装2枚空心拉力螺钉固定后踝(图3)。关闭手术切口, 术后2 d拍摄X线片出院。术后伤口愈合顺利, 小腿肿胀逐渐消退, 术后13 d复查再次拍摄X线片, 与术后2 d X线片相比无明显变化, 但影像显示的踝穴与正常影像有差别, 正常踝穴位X线片胫腓骨重叠部分局限于胫骨切迹部位, 而本例踝穴影像胫腓骨远端重叠部分增加(图3), 考虑可能存在复位不良问题。继而进行CT检查, 影像显示下胫腓联合在脱位状态下固定, 腓骨远端向后脱位, 未进入胫骨远端外侧的切迹内(图4), 因此, 二次入院手术治疗。
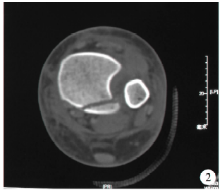
第二次手术在硬膜外麻醉下进行, 扩大原切口, 取出固定螺钉, 并部分显露胫骨切迹, 清理影响复位的软组织。于腓骨近端切口, 显露腓骨骨折端, 复位并固定腓骨骨折(图5), 探查下胫腓联合腓骨旋转得以矫正并复位至胫骨切迹内, 使用复位钳挤压恢复踝穴宽度, 再次平行胫骨远端关节面安装1枚螺钉维持下胫腓联合的对位。侧位X线片显示胫腓骨远端对合关系及腓骨骨折端复位良好(图6)。术后3 d出院休养, 定期门诊复查; 术后12周取出固定踝穴的1枚螺钉, 部分负重练习; 术后6个月恢复正常行走; 术后18个月腓骨骨折愈合良好, 再次手术取出腓骨骨折内固定钛板螺钉及内踝固定螺钉(图7), 手术切口愈合后恢复正常活动。术后3年随访, 美国矫形外科足踝协会(American Orthopaedic Foot & Ankle Society, AOFAS)评分100分。
因损伤累及的结构不同, 手术治疗Maisonneuve损伤的术式也不统一, 安装踝穴螺钉维持下胫腓联合的对合关系是经常采用的术式。手术时腓骨骨折可不处理, 但若合并内踝骨折则需要复位固定, 三角韧带损伤也可不做处理。安装踝穴螺钉时往往需要使用复位钳内外挤压, 以恢复踝穴正常宽度并复位移位的距骨, 然后有限切开或经皮安装踝穴螺钉。操作过程中术者不能直视下胫腓联合的恢复情况, 只能通过术中透视影像凭经验判断, 失误可能就发生在这一环节。
Maisonneuve损伤往往造成下胫腓联合韧带的断裂, 腓骨骨折远端的骨间膜部分撕裂, 腓骨远端部分不稳定, 可发生旋转或下胫腓联合脱位。若术前影像, 特别是CT确认已存在脱位, 术中则需要手法前后挤压腓骨实现复位, 然后再使用复位钳恢复踝穴宽度并固定。但复位钳的使用本身即可造成脱位, 因复位钳内外侧着力点位置不准确可造成腓骨承受向前或向后的应力, 在自身极不稳定的情况下可出现向前或向后移位甚至旋转, 对踝穴的结构产生严重影响, 正如本例所发生的情况。文献报道复位钳安放的角度影响复位效果, 水平方向挤压复位效果更好[1]。
 | 图2 术前CT显示后踝骨折及下胫腓联合分离Figure 2 Preoperative CT scan show fracture of posterior malleolus and syndesmotic diastasis |
 | 图4 术后CT显示腓骨远端脱离胫骨切迹向后方移位Figure 4 Postoperative CT scan show posterior dislocation of distal fibula from incisural notch of distal tibia |
 | 图5 翻修术后前后位X线片踝穴影像恢复正常, 腓骨骨折端恢复对合关系Figure 5 Anteroposterior view X-ray after revision surgery show restoration of ankle mortise, and good reduction of fracture end of fibula |
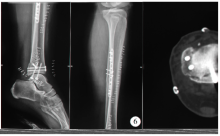 | 图6 翻修术后侧位X线片显示胫腓骨对合关系及腓骨骨折端的良好复位Figure 6 Lateral view X-ray after revision surgery show normal overlap of distal fibula and tibia, and good reduction of fracture end of fibula |
术中影像评估往往侧重于踝穴宽度的恢复, 对下胫腓联合的脱位或复位情况难以做出准确判断, 有经验者可通过影像显示的腓骨远端的外形及胫腓骨重叠程度间接做出判断, 但腓骨近端骨折的复位可提示腓骨长度的恢复, 还不足以就此判断胫腓骨远端的准确复位, 若怀疑下胫腓联合复位不良, 应切开直视下复位[2]。本例存在术者经验不足, 判断不准确的问题。术中旋转踝关节从不同角度观察踝穴影像、腓骨骨折部位的对合情况变化以及侧位腓骨与胫骨重叠影像的变化将有助于判断下胫腓联合的复位。文献报道下胫腓联合损伤手术治疗时, 术中透视影像显示胫腓骨远端复位良好, 但进一步三维影像检查显示复位不良的发生率约32.7%[3]。
术前影像资料要充分, 包括小腿全长正侧位X线片及踝关节CT, 以便评估骨折移位情况、下胫腓脱位程度、内踝及后踝可能伴随发生的细微骨折, 有助于术者制定手术计划及术中采取措施。本例术前CT资料显示下胫腓联合分离, 后踝骨折, 提示下胫腓联合的前后连接结构均已损伤, 腓骨骨折远端部分不稳定。术中缺乏足够重视, 未采取进一步确认的措施, 包括适度扩大切口自前方部分显露下胫腓联合部位或术中CT协助判断, 术后对影像的分析也欠仔细(图3), 没能及时准确判断脱位存在的可能性, 直至完善CT检查后才得以确认, 提示在普通X线片存在可疑处时应及时进行CT检查。
Maisonneuve损伤伴随发生的腓骨骨折往往不需要处理[4, 5], 术者在进行翻修手术时腓骨骨折经切开复位内固定后, 再次探查踝穴已恢复对合关系, 再行踝穴固定时腓骨已成一体, 前后移位或旋转的风险显著降低。一般认为远离胫距关节面的高位腓骨骨折不需要进行骨折端的切开复位处理, 前提是骨间膜完整, 腓骨远端不发生向近端移位的情况, 但Maisonneuve损伤往往发生骨间膜撕裂, 尽管骨折端远离胫距关节面, 但存在旋转及向近端移位的风险, 因此, 腓骨骨折是否需要复位固定还需要进一步观察, 至少应个性化处理。
综上, 本文报告了1例Maisonneuve损伤手术治疗失败的病例, 我们认为, 采取闭合复位踝穴螺钉固定手术治疗Maisonneuve损伤时存在下胫腓联合脱位状态下固定的风险, 术中复位钳的使用不当及术中影像分析不准确是可能的风险因素。
(本文编辑:赵 波)
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|