目的 研究使用种植体支抗整体远中移动下颌牙列治疗骨性Ⅲ类错牙合畸形的疗效。方法 选择轻到中度骨性Ⅲ类错牙合患者20例,男性8例,女性12例,年龄16~38岁,平均(21.5±5.6)岁。采用直丝弓矫治技术,使用下颌外斜线区种植体支抗整体远中移动下颌牙列。患者在治疗前后拍摄X线头颅定位侧位片,对共计26个软硬组织测量项目进行测量分析。结果 矫治结束后患者磨牙关系均达到中性关系,侧貌改善。治疗后ANB角增大(0.80±1.02)°, P<0 .05,Wits值增大(1.67±1.74) mm, P<0.05;L1-NB距离减小(2.64±1.50) mm, P<0.05;下颌第一磨牙近中颊尖远中移动(3.26±1.95) mm, P<0.05;下颌第一磨牙近中根尖远中移动(0.79±1.27) mm, P<0.05;下颌第二磨牙近中颊尖远中移动(3.06±1.80) mm, P<0.05。下颌牙齿与下颌平面的夹角:L1/MP角度减小(6.37±8.53)°,L5/MP角度减小(10.59±8.50)°,L6/MP角度减小(11.48±7.22)°,L7/MP角度减小(15.72±7.16)°,差异均有统计学意义( P<0.05);下唇和审美平面距离减小(1.70±1.59) mm, P<0.05。结论 种植体支抗整体远中移动下颌牙列能够有效治疗恒牙期骨性Ⅲ类错牙合,侧貌改善良好;下颌牙齿发生有控制的倾斜移动。
Objective: To evaluate the clinical effect of distalizing mandibular dentition with micro-implant in patients with skeletal classⅢmalocclusion.Methods: In the study, 20 patients with skeletal class Ⅲmalocclusion were selected. They are consist of 8 males and 12 female with an age range from 16 to 38 years old and an average age of (21.5±5.6) years.They were treated with straight wire technique and the implant were inserted into the mandibular external oblique line to distlize the lower dentition to a class Ⅰmolar relationships.Cephalometrics films were taken before and after treatment. The changes of hard tissue and soft tissue were analyzed by evaluating 26 measurement measurements.Results: ClassⅠmolar relationships were achieved, and the profile were improved after treatment. ANB increased by(0.80±1.02)°,Wits increased by (1.67±1.74) mm,after treatment( P<0.05).The lower dentition were significantly retracted after treatment with L1-NB distance decreased by(2.64±1.50) mm, P<0 .05; the mesial buccal cusp and mesial root of the lower first molars were retracted by (3.26±1.95) mm and (0.79±1.27) mm respectively ( P<0.05); the mesial buccal cusp of the lower second molars were retracted by (3.06±1.80) mm ( P<0.05). After treatment, mandibular teeth got up-righted distally. From incisors to molar, L1/MP, L5/MP, L6/MP, L7/MP angle decreased by(6.37±8.53)°, (10.59±8.50)°, (11.48±7.22)°, (15.72±7.16)°on average respectively ( P<0.05), all of those changes had the statically significant effects. Soft tissue change after treatment, the distance from lower lip to esthetic plane were decreased by (1.70±1.59) mm on average ( P<0.05).Conclusion: Distalizing mandibular dentition with micro-implant can get an satisfying result in patients with skeletal class Ⅲmalocclusion, the lower teeth were retracted by controlled tipping movement.
骨性Ⅲ 类错牙合畸形是临床常见但矫治难度较大的一类错牙合畸形, 患者表现为前牙反牙合、侧貌凹面型, 严重影响了患者的颜面美观、牙牙合功能甚至心理健康及社会交往[1, 2]。据Chan[3]的研究显示, 我国Ⅲ 类错牙合畸形的发病率为12.8%, 远高于西方国家的1%。
多年来, 许多学者对骨性Ⅲ 类错牙合的非手术矫治方法进行了不懈的探索。早期矫形矫治[4]能够利用患者的生长潜力行生长改良治疗, 改善患者的骨型。然而临床上很多患者初次就诊便已错过前方牵引的最佳治疗时机, 或随生长发育骨性Ⅲ 畸形加重使得前牙反牙合复发[5], 因此, 恒牙期骨性Ⅲ 错牙合畸形的掩饰性矫治成为临床治疗的难点, 也是正畸研究的热点。
近年来, 随着种植体支抗技术的不断发展, 种植体支抗强大的支抗力拓宽了正畸治疗的适应证, 实现了下颌磨牙甚至整个下颌牙列的远中移动。本文通过较大样本的临床研究探寻使用种植体支抗整体远中移动下颌牙列治疗骨性Ⅲ 类错牙合的疗效, 并探寻在这种加力方式下下颌磨牙、前磨牙、切牙的移动方式, 为临床应用提供参考。
本研究经过北京大学口腔医院生物医学伦理委员会审批(批准号:PKUSSIRB-2012023), 并取得患者知情同意。选择轻到中度骨性Ⅲ 类错牙合患者20例, 男性8例, 女性12例, 年龄16~38岁, 平均(21.5± 5.6)岁。病例纳入标准:(1)轻中度骨性Ⅲ 类错牙合, 下颌不能后退, 患者及其家长坚持非手术治疗(-4° < ANB< 0° ); (2)磨牙关系近中, 且不超过完全近中; (3)下颌牙弓轻至中度拥挤, 无严重上颌发育不足; (4)根据Baccetti的生长发育颈椎分析法, 入选病例在治疗开始时均至少已处于颈椎骨骨龄5期; (5)经全牙弓分析, 拔除第三磨牙后能提供足够间隙用以回收下颌牙列及解除牙列拥挤。病例排除标准:(1)严重骨性安氏Ⅲ 类错牙合, ANB< -4° , 明显正颌手术指证; (2)患者不愿植入种植体或外斜线区皮质骨过薄; (3)上下牙列严重拥挤; (4)下颌宽度明显不调; (5)颞下颌关节病严重患者; (6)牙周疾病未控制者; (7)其他相关系统疾病患者。
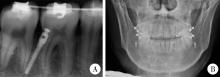
植入术前常规拍摄植入部位的根尖片; 口内黏膜消毒后在下颌第一、第二磨牙间的颊侧黏膜处行局部浸润麻醉, 消毒铺巾; 于第一、第二磨牙间颊侧膜龈联合附近行2~3 mm的切口, 抵达骨面(图1A); 应用探针于切口下探明骨面形态。先锋钻呈与磨牙长轴平行的角度穿透骨皮质(图1B), 用专业螺刀旋入微螺钉至适宜深度(图1C), 拍摄术后X线片。术后嘱患者注意维护口腔卫生, 尤其注意种植体周围软组织的清洁(图2)。
(1)所有患者粘接MBT直丝弓矫治器。使用镍钛圆丝(横截面直径0.35 mm、0.40 mm)、镍钛方丝(横截面0.40 mm× 0.56 mm, 0.48 mm× 0.64 mm)逐步排齐整平牙列, 如患者存在下颌第三磨牙则在排齐后拔除; (2)双侧下颌第一、第二磨牙颊侧植入微螺钉种植体, 换用横截面0.48 mm× 0.64 mm 不锈钢方丝; (3)种植体植入术后两周后种植体加力, 牵拉下颌侧切牙与尖牙间牵引钩, 力值每侧200~300 g(图3); (4)下颌牙列远中移动到位, 尖窝关系良好后停止牵引精细调整; (5)拆除全口矫治器, 进入保持阶段。
X线头影测量分析:每位患者在治疗前(T1)、治疗后(T2)拍摄X线头颅定位侧位片。应用Dolphin软件进行共计16项软硬组织测量项目的定点和测量分析。应用Photoshop CS5软件对10项牙性角度、线距测量项目进行测量(图4)。
采用SPSS 17.0统计包进行统计学分析, 使用配对t检验评价所有测量项目正畸治疗前(T1), 治疗后(T2)的测量值变化, P< 0.05为差异有统计学意义。
临床观察发现20例患者共计植入40颗微螺钉种植体, 1颗种植体发生脱落, 脱落率为2.5%; 有4例患者, 共计5 颗种植体周围软组织增生盖过种植体头部, 但种植体并未发生松动; 其余患者种植体周围的软组织健康, 无感染、肿胀发生。所有患者均未感明显不适, 能良好配合治疗。
治疗前后ANB角均值增大(0.80± 1.02)° , 差异具有统计学意义(P< 0.05); Wits值增大(1.67± 1.74) mm, 差异有统计学意义(P< 0.05), 见表1。
| 表1 20例患者正畸治疗前(T1)、治疗后(T2)骨性变化 Table 1 Skeletal changes of pre-treatment(T1) and post-treatment(T2) of 20 patients /(° ) |
牙性矢状向线距改变:治疗前后, L1-NB距离平均减小(2.64± 1.50) mm, 差异有统计学意义(P< 0.05), 表明下颌前牙发生了有效的回收移动。下颌第一磨牙近中颊尖平均远中移动(3.26± 1.95) mm, 下颌第一磨牙近中根尖平均远中移动(0.79± 1.27) mm, 差异均具有统计学意义(P< 0.05); 下颌第二磨牙近中颊尖平均远中移动(3.06± 1.80) mm, 表明下颌磨牙均发生有效远中移动。
牙性垂直向改变:治疗前后, L1-MP垂直距离平均减小(0.89± 1.39), 差异具有统计学意义(P< 0.05); L6-MP垂直距离平均减小(0.62± 1.07)mm, 差异具有统计学意义(P< 0.05); L7-MP垂直距离平均减小(1.58± 1.40)mm, 差异具有统计学意义(P< 0.05), 见表2。
| 表2 20例患者正畸治疗前(T1)、治疗后(T2)牙性线距改变 Table 2 Distance changes of pre-treatment(T1) and post-treatment(T2)of the tooth of 20 patients /mm |
治疗前后, L1/MP角度平均减小(6.37± 8.53)° , 差异具有统计学意义(P< 0.05); L5/MP角度平均减小(10.59± 8.50)° , 差异具有统计学意义(P< 0.05); L6/MP角度平均减小(11.48± 7.22)° , 差异具有统计学意义(P< 0.05); L7/MP角度平均减小(15.72± 7.16)° , 差异具有统计学意义(P< 0.05), 表明治疗前后, 下颌前、中、后段牙齿均发生了代偿性远中倾斜。
治疗前后, 上下切牙间角度及上前牙角度差异无统计意义, 表明本研究中的治疗过程并未对上颌造成进一步唇倾作用, 代偿主要由下颌牙弓实现。牙合平面变化亦无统计学意义, 并未发生牙合平面的逆时针旋转(表3)。
| 表3 20例患者正畸治疗前(T1)治疗后(T2)牙性角度改变 Table 3 Angular changes of pre-treatment(T1) and post-treatment(T2)of the tooth of 20 patients /(° ) |
治疗前后, 下唇距审美平面距离平均减小(1.70± 1.59) mm, 差异具有统计学意义(P< 0.05), 上唇相对于审美平面位置变化差异无统计学意义(表4)。
| 表4 20例患者正畸治疗前(T1)、治疗后(T2)软组织变化 Table 4 Distance changes of pre-treatment(T1) and post-treatment(T2)of the soft tissue of 20 patients /mm |
患者, 男, 初诊年龄26岁。主诉:“ 地包天” 求治。临床检查:口外:凹面型; 口内:恒牙列, 4颗第一磨牙釉质发育不全; 右侧磨牙关系完全近中, 左侧磨牙关系近中尖对尖, 前牙反覆牙合, 反覆盖3.5 mm; 上牙列拥挤1 mm, 下牙列拥挤1.5 mm; 下中线左偏约3 mm, 上中线正。矫治设计:减数四颗第三磨牙, 直丝弓矫治技术; 下颌外斜线区种植体支抗整体回收下颌牙列; 总疗程27个月。矫治结果:上下牙列齐, 上下中线正, 双侧磨牙关系中性, 前牙反牙合解除; 软组织侧貌改善; X线头影测量:治疗前后ANB角由-1.1° 变为0.1° , 增大1.2° ; 治疗前后下颌角点在前颅底平面投影均位于蝶鞍中心点后方, 治疗前距离为15.0 mm, 治疗后为14.6 mm; L1-NB距离减小4.6 mm; L6近中颊尖、根尖分别远中移动6.6 mm、2.6 mm, L7近中颊尖、根尖分别远中移动4.8 mm、0.2 mm, 下颌切牙、下颌第一磨牙、下颌第二磨牙分别远中直立1° 、6.8° 、14.4° ; 下唇距审美平面距离减小5 mm(图5~12)。
 | 图5 治疗前面像Figure 5 Pre-treatment facial photograph A, pre-treatment front facial photograph; B, pre-treatment front-smiling facial photograph; C, pre-treatment profile photograph. |
 | 图7 治疗中面像Figure 7 During treatment facial photograph A, during treatment front facial photograph; B, during treatment front-smiling facial photograph; C, during treatment profile photograph. |
 | 图9 治疗后面像Figure 9 Post-treatment facial photograph A, post-treatment front facial photograph; B, post-treatment front-smiling facial photograph; C, post-treatment profile photograph. |
骨性Ⅲ 类错牙合的正畸治疗一直以来都是正畸临床研究的难点和热点, 许多学者[6, 7, 8, 9, 10, 11]提出了不同的骨性Ⅲ 类错牙合掩饰性治疗的方法。本研究使用植于下颌外斜线区的种植体支抗成功实现了下颌牙列的整体远中移动达到理想的临床效果, 具体讨论如下。
本研究治疗前后ANB角及Wits值均减小, 差异具有统计学意义, 表明种植体支抗整体远中移动下颌牙列能改善患者Ⅲ 类骨面型。本研究中下颌弓丝采用横截面0.48 mm× 0.64 mm不锈钢方丝, 适当控制下颌前牙牙轴, 利于下颌前部唇侧骨质发生吸收性改建而舌侧骨质发生增生性改建, 进而ANB角减小, 骨面型改善。但治疗后ANB角均值仍处于骨性畸形范围内, 说明代偿性矫治对骨面型的改善仍有限。
下颌牙齿移动方式为下颌磨牙实现整体远中移动伴一定程度的远中直立, 许多学者[12, 13, 14, 15]曾报道了使用各种方法实现上颌磨牙远中移动, 然而, 下颌磨牙的远中移动要远比上颌磨牙的远中移动困难, 这大多是由于下颌磨牙区骨质密度远高于上颌, 舌体运动限制了复杂装置的安放以及作用于下颌的过大的口外力可能会对颞下颌关节造成不良影响等。传统的远中移动下颌磨牙方法如唇挡、下颌延伸舌弓[16]、多曲方丝弓[17]等多数是实现了远中竖直下颌磨牙, 其移动量有限且很难实现牙根的远中移动。本研究中, 下颌磨牙同时实现了牙根及牙冠的远中移动, 治疗前后下颌牙齿均发生了远中倾斜直立, 直立角度由近中向远中呈依次增大的趋势。
上颌前牙唇倾度变化为上颌前牙未发生进一步唇倾, 上颌前牙位置对患者面容美观有重要影响, Cao等[18]的研究显示人们更偏爱直立甚至略微舌倾的上颌前牙。对于过于唇倾的上颌切牙, 即使切牙切缘在前后向并不突出亦不利于患者获得微笑时的颜面美观[19, 20]。传统矫治方法代偿治疗骨性Ⅲ 类错牙合时往往需要使用Ⅲ 类牵引, 而Ⅲ 类牵引作用在上牙弓的近中方向的力使本已代偿性唇倾的上颌前牙更加唇倾。由于并未使用Ⅲ 类牵引, 本研究治疗前后上颌前牙唇倾差异无统计学意义, 表明本研究的治疗过程并未对上颌造成进一步唇倾作用, 基本维持了原有的唇倾度。
牙性垂直向改变为下颌牙齿发生轻度压低, 研究发现[21, 22], 骨性安氏Ⅲ 类垂直骨面型多表现为高角, 可能是Ⅲ 类患者代偿的一种表现, 以尽量减小下颌骨前突造成的矢状向不调, 因此在部分高角骨性Ⅲ 类错牙合患者矫治过程中注意垂直向控制也是矫治中需要注意的问题。传统治疗方法中Ⅲ 类牵引造成的磨牙伸长可能会使下颌平面顺时针旋转, 加重高角面型。本研究中治疗前后下颌牙齿发生轻度压低, 抵消了磨牙远中移动过程中的“ 楔状效应” , 表明了种植体在远中移动牙列的过程中对下颌牙列产生了合适的垂直向控制。
本研究中治疗前后, 下唇距审美平面距离平均减小(1.70± 1.59) mm, 最多回收量5.0 mm, 这一结果略优于传统骨性Ⅲ 类错牙合代偿性矫治[7, 22]报道的1.36~1.40 mm, 表明本研究中的矫治方法能够有效改善患者软组织面型。
利用种植支抗远中移动下颌磨牙或整个下颌牙列时种植体植入部位很重要, 种植体的位置不能妨碍牙齿的远中移动。下颌骨外斜线区骨皮质厚度较其他部位增厚, 锥形束CT研究中下颌磨牙颊侧骨皮质厚度2.81~3.82 mm[23], 选用下颌骨外斜线区作为本研究中种植体植入部位能保证种植体的稳定性。除此之外, 外斜线区增厚的骨皮质也使得种植体的植入方向能够沿磨牙长轴方向, 种植体不进入磨牙牙根之间, 而是位于磨牙牙根颊侧, 因此不会妨碍磨牙在近远中方向上的较大幅度移动, 无需在磨牙移动到位后重新植入种植体。
保留了牙弓的完整性:本研究中的治疗方法无需拔除牙列中段的牙齿, 保留了牙弓的完整性, 这种不拔牙治疗对于仍处于生长发育期的骨性Ⅲ 类患者尤为重要。患者在青少年期可通过非拔牙代偿性治疗纠正咬合关系, 改善侧貌。若随生长发育上下颌骨间不调加重, 错牙合畸形复发或患者对面型有了更高要求, 由于未拔除牙齿, 患者仍可以选择正畸-正颌联合治疗, 不会因拔除了前磨牙而为术前去代偿带来困扰。
需选择合适的适应证:种植体支抗虽能实现下颌牙列的整体远中移动, 但这种移动也是有限度的。间隙分析时需注意第二磨牙远中移动的限度为距下颌升支前缘距离大于或等于黏膜组织厚度。若磨牙远中移动量过大超过了限度则会使磨牙牙冠进入软组织中, 出现第二磨牙“ 阻生” 现象, 患者会出现局部黏膜红肿等不适反应。此外, 治疗前患者下颌前牙区舌侧骨皮质厚度评估也是适应证选择的一个重要方面。若患者治疗前下颌前牙区骨皮质较薄, 且骨性不调较严重, 下颌前牙需要较大回收量, 则在牙列回收过程中有出现下颌前牙舌侧骨开窗、骨开裂的风险。
适当的时机拔除下颌第三磨牙:本研究中所选取的时机是牙列排齐后, 下颌种植体加力之前。之所以选择此时机出于两方面考虑:一是利用拔牙初期骨质愈合代谢加快的时机加速磨牙的远中移动。二是及时为磨牙远中移动提供间隙。如果没有在种植体加力前及时拔除第三磨牙, 则会影响第二磨牙的远中移动, 特别是第二磨牙牙根的远中移动。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|