目的:分析T2N0M0上尿路尿路上皮癌(upper tract urothelial carcinoma, UTUC)患者长期生存情况以及预后相关因素。方法:回顾性分析2000年1月至2013年12月于北京大学第一医院行手术治疗的T2N0M0 UTUC患者的临床和随访资料,应用Kaplan-Meier法计算生存率,Log-rank方法进行单因素分析,对单因素分析中有统计学差异的变量采用Cox模型进行多因素生存分析。结果:共235例T2N0M0 UTUC患者纳入研究,中位随访时间53(3~142)个月。入组患者中男性95例(40.4%),女性140例(59.6%);患者平均年龄(66.73 ±10.49)岁,末次随访时共有74例(31.5%)患者因肿瘤死亡,96 例(40.9%)患者出现膀胱复发,中位死亡时间及复发时间分别为35个月和19.5个月。患者的3年和5年肿瘤特异性生存率分别为89.1%和85.9%;3年和5年无复发生存率分别为85.5%和80.2%。多因素分析发现,年龄大于55岁 ( HR=3.138, 95% CI: 1.348~7.306, P=0.008)和肿瘤直径大于5 cm ( HR=3.320, 95% CI: 1.882~5.857, P<0.001)是T2N0M0 UTUC患者术后肿瘤特异性死亡的独立危险因素;肿瘤发生在输尿管( HR=1.757, 95% CI: 1.159~2.664, P=0.008)和肿瘤低分级( HR=1.760, 95% CI: 1.151~2.692, P=0.009) 是T2N0M0膀胱复发的危险因素。结论:T2N0M0 UTUC患者肿瘤特异性生存预后较好,肿瘤复发率同非浸润性UTUC相当,但复发较早。肿瘤直径大于5 cm和年龄大于55岁是T2N0M0 UTUC肿瘤特异性死亡的独立危险因素;肿瘤发生在输尿管和肿瘤低分级是T2N0M0 UTUC膀胱复发的危险因素。
Objective:To evaluate the impacts of the prognostic factors of T2N0M0 upper tract urothelial carcinoma (UTUC) for Chinese patients.Methods:A retrospective study was conducted including 235 patients who were diagnosed with T2N0M0 UTUC in our hospital and received radical nephroureterectomy (RNU) or partial ureterectomy during January 2000 and December 2013. The 3 and 5-year can-cer-specific survival rates and bladder recurrence-free survival rates of all the patients were valued using Kaplan-Meier method, and the survival curves with statistical significance between the two were compared using the Log-rank test. Variables with significant differences in the univariate analysis were subjected to the multivariate analysis by Cox regression model.Results:A total of 235 patients were included in this study, including 95 (40.4%) male patients and 140 (59.6%) female patients. The mean age was 66.73±10.49 years.The median follow-up time was 53 (rang: 3-142) months, and during the follow-up, 74 (31.5%) patients died of UTUC after a median of 35 months,and 96 (40.9%) patients developed intravesical recurrence after a median of 19.5 months. The 3 and 5-year cancer-specific survival rates of all the patients were 89.1% and 85.9%, respectively; the bladder recurrence-free survival rates were 85.5% and 80.2%, respectively. The independent prognostic factors of cancer-specific mortality were tumor age elder than 55 years ( HR=3.138, 95% CI: 1.348-7.306, P=0.008) and diameter larger than 5 cm ( HR=3.320, 95% CI: 1.882-5.857, P<0.001). The independent prognostic factors of bladder recurrence-free survival were ureter tumor ( HR=1.757, 95% CI: 1.159-2.664, P=0.008) and lower tumor grade ( HR=1.760, 95% CI: 1.151-2.692, P=0.009).Conclusion:T2N0M0 UTUC has a better cancer-specific survival. The intravesical recurrence was equivalent to non-muscle invasive UTUC but earlier. The tumor diameter larger than 5 cm and the patient age elder than 55 years were independently associated with cancer-specific mortality; the primary tumor located in ureter and lower tumor grade were more likely to develop intravesical recurrence.
上尿路尿路上皮癌(upper tract urothelial carcinoma, UTUC)是发生于肾盂和/或输尿管的恶性肿瘤, 约占全部尿路上皮肿瘤的5%[1, 2]。由于UTUC发病率较低, 国内外对其临床特点的大样本报道尚不多见。目前UTUC最常用的评价方法仍是TNM分期和肿瘤分级[2, 3], 两者分别反映了肿瘤的解剖特征和分化特征, 不同临床特征的患者能够表现出显著不同的预后特点, 现在尚未见针对T2N0M0这一特定分期的UTUC的研究报道。T2N0M0 UTUC是指肿瘤侵及肌层, 但未超过肌层到达肾盂和/或输尿管周围脂肪[3]。本研究对T2N0M0的UTUC患者的临床病理数据及预后信息进行回顾性分析, 探讨该类患者的长期生存情况及预后影响因素。
选择2000年1月至2013年12月于北京大学第一医院泌尿外科就诊的T2N0M0 UTUC患者共235例, 所有患者术前均有完整的辅助检查资料(腹部超声、泌尿系CT、胸部X线片等以及实验室检查项目), 患者术前影像学检查及术后组织病理检查均未发现淋巴结转移及远处转移, 且组织病理类型均为上尿路尿路上皮癌。排除标准:(1)既往膀胱癌病史; (2)临床资料不完整; (3)失访患者。
本研究回顾分析的患者临床病理数据包括性别、年龄、组织病理亚型、肿瘤分级、肿瘤部位、肿瘤最大径、肿瘤位置、手术类型(开放性手术及腹腔镜手术)、手术方式(肾输尿管全长切除术[(radical nephroureterectomy, RNU)及输尿管部分切除术(segmental ureter resection)]等。组织病理学亚型根据2004年世界卫生组织(World Health Organization, WHO)标准分类, 肿瘤分级根据1997年WHO推荐标准评估[4], TNM分期参照2002年美国癌症分期手册(American Joint Committee on Cancer AJCC)分期标准进行[5]。
患者随访策略为术后2年内每3个月随访1次, 2年以后为每半年到1年随访1次。以患者的肿瘤特异性死亡和膀胱肿瘤复发为终点指标, 分析患者的肿瘤特异性生存率(cancer specific survival, CSS)和膀胱无复发生存率(bladder recurrence-free survival, BRFS), 及其相关预后因素。
使用SPSS20.0软件进行统计学分析, 用Kaplan-Meier法绘制曲线及生存率的估计, Log-rank检验进行单因素分析, 因素分析中有统计学差异的变量, 进行Cox多因素回归模型分析, 以逐步向前法得到CSS及BRFS的独立危险因素, P< 0.05认为差异有统计学意义。
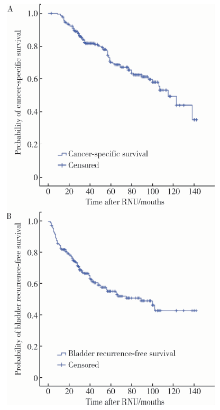
本组235例, 术后随访3~142个月, 中位随访时间53个月。入组患者中男性95例(40.4%), 女性140例(59.6%); 患者平均年龄(66.73 ± 10.49)岁(表 1)。末次随访时共有74例患者(31.5%)因肿瘤死亡, 96 例患者(40.9%)出现膀胱复发, 中位死亡时间及复发时间分别为35个月和19.5个月。患者的3年和5年肿瘤特异性生存率分别为89.1%和85.9%; 3年和5年无复发生存率分别为85.5%和80.2%(图1)。
| 表1 患者一般临床特征及肿瘤特异性生存和膀胱无复发生存的单因素及多因素分析结果 Table 1 Clinicopathologic characteristics of the patients and univariate and multivariate analysis of prognostic factors for cancer-specific survival and bladder recurrence-free survival |
采用Log-rank检验对可能影响T2N0M0 UTUC CSS预后的因素(性别、年龄、左右侧、大小、多灶性、最大肿瘤发生的位置、肾积水、慢性肾病(ehronic kidney disease, CKD)、手术方式、手术类型、输尿管检查史、肿瘤分级、原位癌、肿瘤形态、出血坏死及亚型)进行单因素和多因素分析。年龄大于55岁 (HR=3.138, 95%CI: 1.348~7.306, P=0.008)和肿瘤直径大于5 cm (HR=3.320, 95%CI: 1.882~5.857, P< 0.001)是T2N0M0 UTUC患者术后肿瘤特异性死亡的独立危险因素; 肿瘤发生在输尿管(HR=1.757, 95%CI: 1.159~2.664, P=0.008)和肿瘤低分级(HR=1.760, 95%CI 1.151~2.692, P=0.009) 是T2N0M0膀胱复发的危险因素(表1)。
由于UTUC发病率较低, 目前对UTUC预后及危险因素的研究多数未对肿瘤分期进行分层分析[3, 6, 7, 8], 少数针对中晚期UTUC(advanced UTUC)及非肌层浸润性UTUC(non muscle-invasive UTUC)进行研究, T2N0M0患者的预后因素的研究较少。Abouassaly等[9]的研究发现, T2 UTUC患者3年及5年无进展生存约为78%和76%, 而本中心数据显示为89.1%和85.9%, 短期生存较好。本中心前期研究发现[10], 3年和5年非浸润性UTUC CSS分别为91.5%和86.1%, 两者相较, T2N0M0预后稍差。Lughezzani等[3]报道T2/T3的5年肿瘤特异性生存率为50%, T4小于10%。与T2N0M0患者良好的CSS不同, 其术后膀胱复发率高达 40.9%, 中位复发时间为19.5个月, 而文献报道UTUC的术后膀胱复发率为20%~50%[8, 11, 12], 中位复发时间为15个月, 非肌层浸润性UTUC的术后膀胱复发率为33.2%, 中位复发时间为39个月, 提示肿瘤分期对膀胱复发率并没有显著的影响, 但是复发时间随着肿瘤分期的升高而缩短。
UTUC的预后因素可以分为术前临床因素、术后及病理因素和分子标记物3类。2015年欧洲泌尿外科学会UTUC指南综合文献资料[13], 认为术前预后因素主要包括肿瘤大小、多灶性、肿瘤分级、年龄、吸烟史、肾积水、肿瘤位置、诊断距离手术时间、BMI等。术后预后因素主要包括肿瘤分期、分级、原位癌、淋巴结转移、淋巴血管侵袭、肿瘤形态、肿瘤坏死、组织学亚型等。UTUC预后相关的分子标志物主要包括组织生物标志物(PTP4A3、FGF7、COX2、MMP-11等)、血液生物标志物(贫血、C反应蛋白、淋巴粒细胞比、纤维蛋白原等)和尿液生物标志物(尿沉渣涂片及荧光原位杂交)[3, 13]。本研究发现T2N0M0 UTUC肿瘤特异性生存的预后因素仅与肿瘤大小和患者年龄相关, 此结果与前人研究相符, Kobayashi等[14]发现年龄是男性UTUC患者的独立预后因素, Petrelli等[15]通过meta分析发现年龄是患者术后总生存的预后因子, Kim等[16]发现年龄是肿瘤特异性生存的重要影响因素, 多项研究证实[15, 17, 18, 19], 肿瘤体积越大, 其预后越差。
此外, 有研究报道[20, 21, 22], 肿瘤发生坏死和肿瘤预后相关, 但本研究在T2N0M0 UTUC肿瘤中, 并没有发现两者有相关关系, 这可能和肿瘤分期较低和根治性的手术方式有关。早期研究表明[23, 24], 肿瘤发生在输尿管的患者预后较差, 但近来一些研究认为[25, 26, 27], 肿瘤位置和患者预后并不相关, 与UTUC预后的关系尚存在争议。本研究肿瘤位置并不是患者预后生存的独立预测因素, 其可能与肾盂癌恶性程度较高有关。
Leow等[28]通过meta分析发现UTUC膀胱癌病史或UTUC合并膀胱癌是UTUC患者的术前预后因素, Nuhn等[29]一项多中心研究发现膀胱癌病史是UTUC患者肿瘤特异性死亡的危险因素。本研究通过分析膀胱复发和患者预后的关系, 发现患者膀胱复发和预后并没有相关关系(数据未提供), 表明T2N0M0 UTUC患者膀胱复发和患者生存可能没有相关关系。2015年欧洲泌尿外科学会UTUC指南认为, 肿瘤高分级是UTUC患者预后的独立危险因素, 但在本研究T2N0M0患者中, 肿瘤分级和患者预后没有关系, 这可能暗示肿瘤分级不影响该类患者预后。本研究结果对T2N0M0 UTUC患者的治疗和预后有一定的指导意义, 但尚待多中心大数据验证。
本研究发现肿瘤原发灶发生于输尿管和肿瘤低分级会增加膀胱复发的概率, 本课题组前期研究发现在整体UTUC患者中[8], 肿瘤低级别且肿瘤发生在低位输尿管容易复发, 本研究结果与其相符合, 但具体机制尚不清楚, 可能与中国的马兜铃酸中草药服用史有关[30], 然而, 已有文献报道术前的输尿管镜检查可以增加膀胱复发的风险[31]。本研究输尿管镜检查和肿瘤多灶性对BRFS无显著相关性, 这可能与本研究组患者进行输尿管镜检的病例数较少有关。
本研究的局限性:(1)为回顾性研究, 虽然在入组患者时设置了严格的纳入标准, 排除了失访人群, 但仍无法避免选择偏倚; (2)筛选出的术后膀胱复发的预后因素较少, 提示本中心T2N0M0 UTUC样本量较小, 需进一步扩大样本进行研究; (3)本研究为单中心研究, 研究结果有待其他研究者进行外部验证。
综上所述, T2N0M0期UTUC患者肿瘤特异性生存较好, 其膀胱复发率与各期UTUC相当, 但复发的时间间隔随着肿瘤分期而改变。本研究筛选出的预后相关因素中肿瘤大于5 cm和年龄大于55岁是肿瘤特异生存的独立危险因素; 肿瘤低分级和肿瘤位置在输尿管是T2N0M0 UTUC患者术后膀胱内复发的独立危险因素。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|