目的 探讨超声在髋关节前上盂唇撕裂中的诊断价值。方法 连续收集102例临床拟诊髋关节盂唇撕裂患者的超声检查、磁共振检查(magnetic resonance imaging,MRI)和关节镜手术资料,其中男性42例,女性60例,平均年龄(35.14±9.16)岁(13~60岁), 左侧髋关节44例,右侧髋关节58例。以关节镜手术为金标准,评估超声诊断髋关节前上盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值和准确性,并与MRI比较。结果 所有病例均经关节镜手术证实,其中91例为髋关节前上盂唇撕裂,11例髋关节盂唇无撕裂。超声正确诊断69例,包括髋关节前上盂唇撕裂60例和髋关节盂唇无撕裂9例;其余33例中,超声误诊2例,漏诊31例;超声评估髋关节前上盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值和准确性分别为65.93%、81.82%、96.77%、22.50%和67.65%。MRI正确诊断77例,包括髋关节前上盂唇撕裂70例和髋关节盂唇无撕裂7例;其余的25例中,误诊4例,漏诊21例;MRI评估髋关节前上盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值和准确性分别为76.92%、63.64%、94.59%、25.00%和75.49%。超声检查与MRI检查结果相比,在评估髋关节前上盂唇撕裂的准确性上,超声检查低于MRI,差异有统计学意义( P<0.01)。结论 超声诊断髋关节前上盂唇撕裂的敏感性略低于MRI,但超声检查的特异性高,动态评估是超声检查的优势,可以作为一种有效的检查方法。
Objective: To explore the value of ultrasound in the diagnosis of anterosuperior acetabular labral tear.Methods: A total of 102 patients [(42 males and 60 females, age from 13 to 60 years, average age was (35.14±9.16) years] with suspected anterosuperior acetabular labral tear were included in this study, including 44 left hip joints and 58 right hip joints. All the patients received hip joint ultrasound and magnetic resonance imaging (MRI) evaluation before arthroscopy surgery. Using arthroscopy as golden standard, the sensitivity, specificity, positive predictive value, negative predictive value and accuracy between ultrasound and MRI were calculated and compared.Results: There were 91 antero-superior acetabular labral tears of 102 patients which were confirmed during arthroscopy surgery. Sixty-nine patients were diagnosed correctly by ultrasound, including 60 anterosuperior acetabular labral tears and 9 with no acetabular labral tears, whereas 2 were false-positive and 31 were found to be false-negative. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy by ultrasound were respectively 65.93%, 81.82%, 96.77%, 22.50% and 67.65%. In contrast, seventy-seven patients were diagnosed correctly by MRI, including 70 anterosuperior acetabular labral tears and 7 with no acetabular labral tears, whereas 4 were false-positive and 21 were found to be false-negative. For MRI, the sensitivity, specificity, positive predictive value, negative predictive value and accuracy were respectively 76.92%, 63.64%, 94.59%, 25.00% and 75.49%. The results of ultrasound and MRI were in accordance in 68 of the 102 patients. There were 51 anterosuperior acetabular labral tears of the 68 patients who were diagnosed by both ultrasound and MRI, whereas there were 17 with no acetabular labral tears of the 68 patients who were diagnosed by both ultrasound and MRI. The results of ultrasound and MRI were inconsistent in 34 of the 102 patients. In 11 of the 34 patients, in which case ultrasound diagnosed anterosuperior acetabular labral tear, MRI found no acetabular labral tear. Whereas, in 23 of the 34 patients, in which case MRI diagnosed anterosuperior acetabular labral tear, ultrasound found no acetabular labral tear. As compared with MRI findings, ultrasound had a lower accuracy for anterosuperior acetabular labral tear than MRI, there was statistical difference on the accuracy for anterosuperior acetabular labral tear ( P<0.01).Conclusion: Although ultrasound had a slightly lower sensitivity for anterosuperior acetabular labral tear, it had a higher specificity than MRI. Dynamic evaluation of antero-superior acetabular labral tear is an advantage of ultrasound. Ultrasound could be used as a feasible me-thod to evaluate anterosuperior acetabular labral tear.
髋关节盂唇撕裂是引起髋部疼痛的常见原因[1], 在髋部和腹股沟区疼痛患者中的发生率高达22%~55%[2]。磁共振检查(magnetic resonance imaging, MRI)对于盂唇分辨率高, 已经成为评估髋关节盂唇损伤的重要影像学方法[3], 特别是磁共振关节造影(magnetic resonance arthrography, MRA)诊断髋关节盂唇撕裂具有很高的敏感性和特异性。然而, MRI以及MRA成像技术要求高, 操作费时且费用昂贵。与之相比, 高分辨率超声同样具有良好的组织分辨率, 并能进行实时动态观察, 使术前超声诊断髋关节前上盂唇撕裂成为可能。
选取2014年7月至2016年5月因髋部疼痛就诊北京大学第三医院运动医学门诊, 临床拟诊髋关节盂唇撕裂欲行手术修补患者为本研究对象。患者共102例, 其中男性42例, 女性60例, 平均年龄(35.14± 9.16)岁(13~60岁), 左侧髋关节44例, 右侧髋关节58例。所有患者在关节镜手术以前均进行临床体格检查、超声检查、MRI或MRA检查。本研究获得北京大学第三医院伦理委员会批准, 所有研究对象均签署知情同意书。
采用美国GE Logiq E9彩色多普勒超声诊断仪, 根据情况选取C1-5凸阵探头或9L线阵探头。超声检查时, 患者仰卧位, 下肢轻度外旋、外展。探头首先沿股骨颈长轴方向进行髋关节斜矢状面扫查(clock-face分区法3点方向), 识别髂骨髋臼顶、关节囊、盂唇及股骨头、颈部, 然后探头向外侧及内侧平行移动, 评估髋关节前方(clock-face分区法12点至5点方向)区域盂唇形态及回声。静态评估后, 于髋关节被动屈曲0° ~90° 、内收0° ~20° 、内旋0° ~30° [4, 5]活动状态下再次评估盂唇形态, 并动态观察股骨头、头颈交界处与盂唇间的相互位置关系。单侧髋关节超声检查时间大约5~10 min。
全部患者由同一名具有8年以上肌骨超声工作经验的超声医师进行检查, 所有髋关节手术由同一名具有8年关节镜手术经验的运动医学科医师实施。
所有数据采用SPSS 21.0统计软件进行相关统计分析, 以关节镜手术为金标准, 比较超声检查与MRI检查在诊断髋关节盂唇撕裂中的价值。计数资料两组间比较采用配对卡方检验, 统计学指标包括敏感性、特异性、阳性预测值、阴性预测值和准确性, 以P< 0.05为差异有统计学意义。
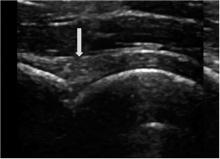
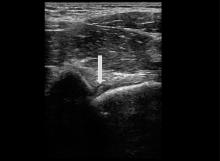
扫查髋关节纵断面时, 正常盂唇显示为边缘平滑、锐利的三角形结构, 内部呈相对均匀的高回声(图1), 凸阵探头扫查或受扫查角度影响, 盂唇可呈低回声。
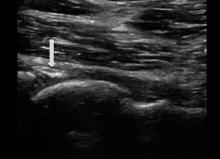
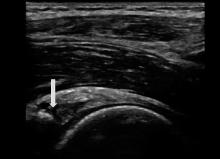
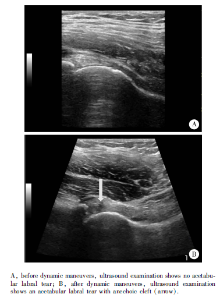
髋关节盂唇撕裂时, 声像图可以表现为:(1)盂唇形态饱满, 内部回声不均匀(图2); (2)盂唇结构缺失, 局部可见斑片样强回声; (3)盂唇内不同形态的低回声或无回声裂隙, 典型者可位于盂唇基底部, 贯穿整个盂唇附着缘(图3), 裂隙也可位于盂唇内部, 形态不规则; (4)盂唇旁囊肿, 表现为紧邻盂唇的无回声结构, 无回声往往形态欠规则, 边界清晰(图4)。以上声像图表现可单独出现或合并出现, 符合任一条时即可诊断为髋关节盂唇撕裂[6]。此外, 部分患者静息状态下扫查, 盂唇内的异常声像图改变可不典型, 在髋关节动态活动过程中或活动后, 往往盂唇内的裂隙显示的更清晰, 可以增加诊断信心(图5)。
102例髋部疼痛病例中, 经关节镜手术证实91例髋关节前上盂唇撕裂, 11例髋关节盂唇无撕裂。超声正确诊断69例(其中动态观察后获得诊断者20例), 包括髋关节前上盂唇撕裂60例和髋关节盂唇无撕裂9例; 其余33例中, 超声误诊2例, 漏诊31例。超声评估髋关节前上盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值和准确性分别为65.93%、81.82%、96.77%、22.50%和67.65%, 见表1。
| 表1 超声检查和关节镜手术结果的比较(n=102) Table 1 The comparison of findings between ultrasound and arthroscopy(n=102) |
102例髋部疼痛病例中, 经关节镜手术证实91例髋关节前上盂唇撕裂, 11例髋关节盂唇无撕裂。MRI正确诊断77例, 包括髋关节前上盂唇撕裂70例和髋关节盂唇无撕裂7例; 其余的25例中, 误诊4例, 漏诊21例。MRI评估髋关节前上盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值和准确性分别为76.92%、63.64%、94.59%、25.00%和 75.49%, 见表2。
| 表2 MRI检查和关节镜手术结果的比较(n=102) Table 2 The comparison of findings between MRI and arthroscopy(n=102) |
102例髋部疼痛病例中, 超声检查与MRI检查结果一致68例, 其中51例二者均提示髋关节前上盂唇撕裂, 17例二者均提示髋关节盂唇无撕裂; 34例二者检查结果不一致, 其中超声检查提示前上盂唇撕裂而MRI提示盂唇无撕裂11例(图6、7), MRI提示前上盂唇撕裂而超声提示盂唇无撕裂23例。超声检查与MRI检查结果相比, 在评估髋关节前上盂唇撕裂的准确性上, 超声检查低于MRI, 差异有统计学意义(χ 2=7.483, P=0.006), 见表3。
| 表3 超声检查和MRI检查结果的比较(n=102) Table 3 The comparison of findings between ultrasound and MRI(n=102) |
髋部及腹股沟区非急性创伤性疼痛的病因很多, 骨盆X线片及CT检查可以显示髋关节骨性结构异常。然而, 大部分髋关节原因引起的病变, 关节骨性结构异常时, 病变往往已属晚期。随着对髋关节运动方式认识的深入、影像学的发展以及关节镜的广泛应用, 越来越多的早期病变得到诊断和治疗, 其中髋关节盂唇撕裂是较为常见的病变, 也是髋部疼痛的常见重要原因[7]。
关节镜术中探查是诊断髋关节盂唇撕裂的最终金标准, 但很难作为单纯诊断手段。MRI特别是MRA是评估髋关节盂唇撕裂敏感性比较高的一种影像学检查方法, 但MRI价格相对昂贵, 并且在某些情况下不能使用, 如患有幽闭恐怖症、放置起搏器或体内有金属异物的患者。相比较而言, 超声是一种价格低廉、快速、无创的检查方法, 特别是高频超声的软组织分辨率佳, 可以清晰显示髋关节周围软组织情况。与MRI检查相比, 超声的局限性在于不能提供髋关节整个环周盂唇的完整信息, 无法显示关节软骨和骨髓水肿。不过, 多项研究显示, 几乎所有与髋关节发育不良或撞击综合征相关的盂唇撕裂, 包括急性运动创伤所致的盂唇撕裂都发生在髋关节盂唇的前上部位[8, 9, 10], 而这一区域恰好能充分被超声显示。本研究结果也证实了这种情况, 表明超声在髋关节盂唇撕裂的诊断中具有临床应用价值。
国内外有关髋关节盂唇撕裂的超声研究较少, Troelsen等[6]的研究中, 超声评估髋关节盂唇撕裂的敏感性、特异性、阳性预测值、阴性预测值分别为44%、75%、88%、25%。Troelsen等[5]在两年后发表的另一份研究显示超声诊断的敏感性和阳性预测值均明显增高, 均达到94%。Troelsen的两次研究结果表明, 利用超声诊断髋关节盂唇撕裂需要较长的学习曲线, 超声诊断水平与超声医师的经验明显有关。本研究中, 超声检查评估髋关节盂唇撕裂的敏感性为65.93%, 高于Troelsen的第一次研究, 但低于他们第二次的结果, 其原因除与髋关节盂唇撕裂超声诊断的学习曲线有关外, 还可能与参考标准不同有关, Troelsen采用MRA为金标准, 而本研究以关节镜手术为金标准。另外, 本文选择经临床保守治疗无效、拟行手术的患者为研究对象, 大部分患者盂唇撕裂程度较重, 也使得超声易于检出, 病例的选择偏倚也是本文的不足之一。
本研究结果发现, 以髋关节关节镜手术为金标准, 超声诊断髋关节前上盂唇撕裂的敏感性低于MRI, 但超声评估髋关节前上盂唇撕裂的特异性和阳性预测值却高于MRI, 表明超声检查可以作为评估髋关节前上盂唇撕裂的一种可行方法。尤其当患者患有幽闭恐怖症无法进行MRI检查, 或者患者身体虚弱等原因不能进行MRI检查时, 超声检查可以作为一种可行的替代检查方法。
不过, 无论文献及我们的经验都表明, 髋关节盂唇撕裂的超声检查学习曲线较长并有一定的操作者依赖性。对于初学者而言, 我们的经验表明首先要深入理解髋关节的局部解剖结构, 掌握髋关节超声检查体位及扫查方法, 将髋关节声像图表现与髋关节解剖结构一一对应并熟悉正常声像图表现, 积累至少30例髋关节及前上盂唇超声检查的经验以后, 可以进行盂唇病变的超声评估。我们今后工作的重点在于如何规范髋关节的超声检查方法, 根据已有的经验建立起一套髋关节前上盂唇撕裂评估的超声检查程序, 推广超声在髋关节前上盂唇撕裂中的应用。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|