SUMMARY Bisphosphonate-related osteonecrosis of the jaw (BRONJ) as one serious side-effect of bisphosphonate therapy has been known for more than ten years since it was first reported in 2003. In the majority of the cases BRONJ occurs more commonly in the mandible. Those involving the maxilla are relatively few. This paper reported a case that a patient with multiple myeloma developed bilateral maxillary BRONJ after tooth extraction. The patient had used bisphosphonates for more than three years meanwhile with uncontrolled diabetes mellitus. The patient recovered completely after surgical treatment in combination with diabetes disease control and antibiotics application. Two key factors to ensure the success of surgical treatment are as follows: sufficient removal of infected and necrotic tissue and good blood-supply for the local flap to help completely close the wound. The literature was reviewed to analyze the reasons why bone necrosis related to bisphosphonates was most likely to occur in the jaw especially in the mandible according to the pathogenesis of this disease. Furthermore the related risk factors of BRONJ presented in this case were discussed such as tooth extraction oral infection and diabetes mellitus etc. We summarized adjuvant prophylaxes for prevention of BRONJ after tooth extraction for example drug holiday that could be used in the dental clinic. This case report reminds us that it’s of great importance to establish the awareness that the osteonecrosis of the jaw may be related to the use of some bone-stabilizers. As for patients with a history of exposure to antiresorptive or antiangiogenic agents; dentists are supposed to be cautious. It’s recommended to take appropriate measures in perioperative period of oral surgical treatment to prevent BRONJ.
二膦酸盐类(bisphosphonates, BP)药物作为一种强效骨吸收抑制剂已用于临床30余年, 广泛用于控制与骨代谢改变相关的疾病, 如:骨质疏松症、恶性肿瘤骨转移、恶性肿瘤引起的高钙血症、多发性骨髓瘤和Paget骨病。自2003年Marx[1]首次报道二膦酸盐类药物可导致颌骨坏死的现象以来, 相关病例报道逐渐增多。根据2014年美国口腔颌面外科医师协会(American Association of Oral and Maxillofacial Surgeons, AAOMS)发布的最新临床指南[2]:由于越来越多患者的颌骨坏死与使用包括二膦酸盐类药物在内的抗骨吸收药物及其他抗血管生成药物(如地诺单抗)相关, 推荐把二膦酸盐相关性颌骨坏死(bisphosphonate-associated osteonecrosis of the jaw, BRONJ)更名为药物相关性颌骨坏死(medication-related osteonecrosis of the jaw, MRONJ)。该指南将MRONJ定义为:以往或目前正在应用抗骨吸收或抗血管生成药物; 在口内骨暴露或经过口内、外瘘口可以探及骨面, 骨不愈合的时间超过8周; 颌骨未曾接受过放疗, 或无明确的颌骨转移灶。
本文报道1例拔牙术后出现双侧上颌骨二膦酸盐相关性颌骨坏死的病例, 通过手术治疗, 效果满意。
患者, 男, 55岁。因双侧上颌后牙松动不适伴疼痛, 半年前于外院分次拔除。术后出现拔牙创不愈合伴肿胀、流咸味液体, 未经诊治。
患者5年前因腰部多发性骨髓瘤行腰部病灶放射治疗27次。化学治疗:初期静脉注射硼替佐米(商品名万珂)2年; 后改为静脉滴用帕米磷酸二钠(第二代二膦酸盐类药物, 商品名博宁)3.5年, 就诊时已停用2个月。定期在血液科复查, 多发性骨髓瘤病情稳定。同时患有糖尿病5年, 采用皮下注射胰岛素治疗, 血糖控制不满意, 空腹血糖水平8~9 mmol/L。
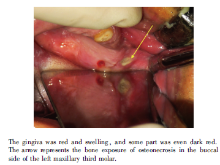
临床检查:面部外形对称, 开口度三指, 开口型无异常。上颌仅存13、23残根, 边缘齐牙龈水平。左上颌后部牙龈红肿, 局部呈暗红色, 触压不适, 25、27牙位颊侧牙龈可见瘘口, 触压有脓液溢出, 28对应颊侧可见死骨暴露(图1)。右上颌后部牙龈红肿, 局部呈暗红色, 触压不适, 14、17牙位牙龈可见瘘口, 触压有脓液溢出。下颌牙列缺损。
曲面体层片示:双侧上颌骨后部骨密度不均匀降低, 上颌窦底不清晰。
锥形束CT(cone beam computer tomography, CBCT)示:左上颌磨牙区牙槽突及结节处不规则骨破坏, 牙槽嵴顶凹凸不平, 可见多块死骨, 病变累及上颌窦底, 左上颌窦黏膜增厚(图2A~C); 右上后牙区骨嵴顶虫蚀样不规则骨破坏, 其中可见多块死骨(图2D~F); 符合双上颌骨骨坏死表现。
患者以“ 双侧上颌骨后部二膦酸盐相关性颌骨坏死” 收入院, 行进一步诊治。入院后, 完善各项术前准备。内分泌科会诊制定合理降糖方案, 控制血糖。取病灶脓液细菌涂片:G(-)杆菌、G(+)球菌、大量白细胞、白细胞胞浆内有细菌, 根据细菌涂片结果使用相应抗生素。
患者血糖调整至正常水平后, 全身麻醉下行“ 双侧上颌二膦酸盐相关性颌骨坏死刮治术” 。根据病变及瘘口位置, 设计左上颌梯形切口, 切口范围为23至上颌结节, 切至骨面, 自骨膜下翻瓣, 显露牙槽嵴骨质, 牙槽骨破坏明显, 局部骨质蜂窝状, 质硬, 可见脓液渗出(图3A)。咬骨钳扩大去除坏死骨质, 动力打磨, 去除尖锐骨尖。大量生理盐水冲洗, 充分止血, 可吸收线牙龈对位缝合(图3B)。同法行右侧上颌手术。手术过程顺利, 历时75 min, 术中出血100 mL。
术后患者恢复平稳, 复查曲面体层片及CBCT提示, 双侧上颌骨后部可见骨密度减低区, 与术前(图2A~F)相比死骨消失, 双侧上颌窦底骨质未穿通(图4A, B)。术后继续监测控制血糖, 全身使用相应抗生素, 2 d后出院。嘱患者继续保持口腔卫生, 避免外力刺激, 注意控制血糖水平。随访至术后2个月, 伤口愈合良好。
BP类药物引起骨坏死的发病机制尚无定论, 目前普遍认为其主要作用是抑制破骨细胞的活性, 并诱导破骨细胞凋亡, 破坏正常骨组织中成骨细胞与破骨细胞间的动态平衡。当BP类药物在骨组织中的浓度过高, 则对骨组织中的其他细胞同样具有毒性作用。研究表明, 通过静脉途径给药, 约一半剂量的BP类药物最终将被骨组织吸收[3], 而上、下颌骨尤其是牙槽突区域由于频繁的咀嚼和言语活动, 相对轴状骨和四肢骨血运更丰富、骨代谢更快, 因而BP类药物被吸收后在上、下颌骨中浓度最高[4]。此外, 由于颌骨是高度可塑性的组织, 也是人体骨代谢最活跃的部分, 因此其对BP类药物引起的成骨细胞与破骨细胞间的平衡失调及其对骨组织的毒性作用更为敏感[4]。
与上颌骨相比, BRONJ较多发生于下颌骨。最近一篇关于BRONJ的系统性综述统计了2004— 2014年全部文献报道的BRONJ病例的发病部位, 在6 199个病例中, 下颌骨65.0%、上颌骨28.4%、上颌骨和下颌骨6.5%[5]。下颌骨发病最多可能与其血供单一、骨皮质厚、侧支循环不易建立有关。但上颌骨血供丰富、骨松质多、侧支循环容易建立, 却仍有包括本病例在内的部分BRNOJ发生于上颌骨, 这说明除了BP的抗血管形成作用, 其他风险因素(如拔牙等创伤性操作、感染、糖尿病等)也可能在BRONJ的发生、发展中起到重要作用。
临床和流行病学研究发现, 在出现BRONJ的临床表现之前常有创伤性牙科操作[6]。我院自2009年3月至2013年12月诊治的24个BRONJ患者中19例均有拔牙史, 不难得出牙槽骨创伤后易引发相关临床症状的结论[7]。也有文献报道, 在乳腺癌发生BRONJ的患者中, 拔牙本身与颌骨坏死的严重程度并没有直接关系[8]。目前, 人们普遍认为拔牙是BRONJ的触发因素(trigger event)。在AAOMS 2014年发布的最新临床指南中将拔牙称为BRONJ发生的“ 独立局部危险因素” [2]。一些指南甚至建议:在使用二膦酸盐类药物期间应避免拔牙操作[9]。
与此同时, 人们也在临床工作中不断摸索和总结避免拔牙后发展为BRONJ的措施。有学者建议在进行拔牙等有创性操作前暂停药物应用(drug holiday), 直至软组织愈合再开始重新用药[5]。但因为BP会在骨内沉积很多年, 目前并没有任何证据支持这个建议可以改善口腔有创操作后的结局。2011年, 美国牙科协会指导意见明确:使用低剂量BP治疗骨质疏松的患者发生BRONJ的风险极低, 没有必要为预防颌骨坏死而在牙科有创操作前暂停BP用药[10]。而对于静脉使用高剂量BP抗肿瘤的患者, 如果需要创伤很大的口腔操作, 同时伴有多个发生颌骨坏死的危险因素(如:吸烟、糖尿病、使用激素), 最好在拔牙前暂停抗骨吸收药物的应用[5]。
其他预防措施还包括:在拔牙前3天预防性使用抗生素; 术前每天用0.2%(质量分数)氯己定含漱, 若能检测到菌斑则进行口腔洁治; 使用微创拔牙器械(如超声骨刀)[11], 拔牙后用富含生长因子的血浆充满拔牙窝[11], 促进拔牙窝愈合; 用黏膜瓣覆盖拔牙窝[12], 以隔离外界细菌。有研究表明, 用颊脂垫黏膜瓣覆盖上颌后牙区的开放创口可加速坏死性病变的愈合, 因为颊脂垫富含血管和脂肪组织干细胞[13]。
然而也有研究认为, BRONJ的触发因素并非拔牙本身, 而是拔牙后的局部感染状态[14]。有些研究已证实, 许多细菌有刺激骨吸收、抑制骨形成的作用[15, 16], 一些动物实验也支持感染在BRONJ的发生中具有重要作用。Aguirre等[17]在牙周炎进展期的小鼠中分别给予阿仑膦酸钠、低剂量唑来膦酸和高剂量唑来膦酸, 结果在给予高剂量唑来膦酸的小鼠中诱导出类似BRONJ的颌骨病变; Aghaloo等[18]在腹腔内注射唑来膦酸达3周的小鼠中, 通过丝线结扎牙颈部诱导其发生进展性牙周病, 随后小鼠出现了类似BRONJ的病变。由此推测, 强力的BP用药加上进展性牙周病足以引发BRONJ。本例患者上、下颌多颗牙齿多年来因松动相继拔除或脱落, 结合其口腔卫生差, 不难猜测其之前可能患有牙周炎, 患者入院后的病灶脓液细菌涂片结果也证实其病灶区正处于急性感染状态。由此可见, 感染在该患者BRONJ的发生中可能也起到一定促进作用。因此, 除了术前使用相应抗生素, 术后仍需继续使用抗生素, 并嘱患者注意保持口腔卫生。
最近有研究认为, 糖尿病也是BRONJ的危险因素之一[19], 糖尿病对骨转化和骨重建具有抑制作用, 并增加成骨细胞和破骨细胞的凋亡, 从而降低骨代谢水平。此外, 糖尿病患者常伴有微血管缺血和免疫细胞功能改变, 这些都对BRONJ起到促进作用。本例患者患糖尿病多年, 血糖控制不佳, 或许也促使其BRONJ的发生, 因此, 血糖控制需贯穿其整个围手术期。
本病例提示, 口腔医生接诊患者时采集病史要全面, 重视患者的全身情况(如肿瘤、骨质疏松、糖尿病等)及用药史(尤其是抗血管生成药及抗骨吸收药物)对口腔健康的影响, 在没有病灶牙及颌面部放疗史时, 建立颌骨坏死可能与使用某些药物相关的意识。对于使用过抗血管生成药物及抗骨吸收药物的患者, 拔牙需谨慎, 应综合考虑手术创伤程度、患者自身危险因素、内科医生意见等多个方面, 在拔牙术围手术期采取措施预防术后出现颌骨坏死。对于内科医生, 在给患者使用抗血管生成药物及抗骨吸收药物之前, 应建议患者先接受全面的口腔检查, 预先处理牙齿疾病, 尽可能降低发生药物相关性颌骨坏死的风险。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|