伴有交感神经症状颈椎病的治疗大多以保守治疗为主, 临床疗效不甚满意, 手术治疗在国内外更是鲜有开展[1, 2, 3, 4, 5]。北京大学第一医院骨科2000年3月至2007年5月, 采用前路椎间盘切除聚醚醚酮(polytheretherketone, PEEK)椎间融合器辅助的椎体间植骨融合术(anterior cervical discectomy and fusion, ACDF), 治疗伴有交感神经症状的颈椎病患者48例, 取得了很好的临床疗效。本组收集了ACDF手术后随访时间不少于1年资料完整的39例患者病例资料, 现报告如下。
选择北京大学第一医院骨科2000年3月至2007年5月, 手术治疗伴有交感神经症状的脊髓型或神经根型颈椎病患者共48例, 有完整随访资料(随访不少于1年)者39例, 其中男22例, 女17例, 年龄39~79岁, 平均56.6岁。
入选标准:(1) 均伴有交感神经症状, 由于交感神经症状目前尚缺乏公认的判断标准, 本研究根据仅有的文献确定交感神经症状[1, 2, 3, 4, 5]; (2) 颈椎MRI显示明确的脊髓压迫; (3) 排除神经内科、心内科、耳鼻喉科及眼科等相关科室的疾患; (4) 采用 ACDF 治疗; (5) 随访不少于1年。
1.2.1 手术方法及术后处理
1.2.1.1 手术适应证 伴有交感神经症状的脊髓或神经根型颈椎病, 诊断明确并排除其他科室疾患, 症状进行性加重或严重影响工作和生活者, 其中神经根型颈椎病需严格保守治疗1年以上无效。
1.2.1.2 手术方法 采用全身麻醉或颈丛麻醉, 前路横弧形小切口行椎间盘刮除, 1 mm椎板咬骨钳咬除钩椎关节骨刺, 椎间隙充分减压, 刮断后纵韧带并显露硬膜囊, 刮除软骨终板, 打磨粗糙面, 植入充满同种异体松质骨的PEEK椎间融合器(Solis, Stryker 公司, 法国)。根据MRI上显示的脊髓压迫水平, 以及颈椎过伸过屈X线片上显示颈椎不稳定的节段来确定减压节段, 其中单节段减压8例, 双节段23例, 三节段8例, 病变节段包括C34、C45、C56及C67。
1.2.1.3 术后处理 术后第2天拔除伤口引流管, 戴颈托下地, 术后3~4 d出院。术后2个月门诊复查后去除颈托。
1.2.2 影像学评估
分别于术后2个月、半年及1年拍颈椎正侧位及动力位X线片, 必要时复查颈椎CT或MRI。
融合成功的判定:(1)颈椎侧位X线片上融合器与椎体接触面无透亮带; (2)颈椎侧位X线片上有连续骨小梁通过; (3)颈椎动力位X线片上椎间角变化小于2° 或融合节段棘突间活动度小于2 mm。
如不能确定是否融合, 则拍CT二维重建以除外假关节形成[6, 7]。
1.2.3 临床疗效的评估
采用20分评分法[1], 分别对交感神经症状(包括头晕、恶心呕吐、头痛及枕颈部不适、心慌、胸闷憋气、阵发性高血压、耳鸣、视物模糊、记忆力下降、胃肠道不适及顽固性呃逆)进行评分(表1、2)。
| 表1 交感神经症状评分法 Table 1 Score of sympathetic symptoms |
| 表2 39例患者中交感神经症状发生率 Table 2 Incidence of sympathetic symptoms in 39 patients |
症状改善率(recover rate, RR)为:(术前评分-术后评分)/(术前评分)× 100%, 改善率在75%及以上为优, 50%~74%为良, 25%~49%为中, 25%以下为差, 改善率≥ 50%即达到优良为临床效果满意。
计算临床效果满意率(临床效果满意人数/总人数)× 100%。术前及术后2个月及末次随访时各评分1次, 计算末次随访时的改善率, 交感神经症状评分数据用F检验进行统计学分析, 两两比较用LSD法, P< 0.05认为差异有统计学意义。
所有患者经过1年及以上随访, 随访时间12~36个月, 平均15.6个月。术后交感神经症状均有不同程度改善, 术前交感神经症状评分为8.4± 1.0, 术后2个月评分为2.2± 0.3, 末次随访评分为2.4± 0.3, 差异有统计学意义(F=176.57, P< 0.001)。改善率为优22例, 良15例, 可1例, 差1例(表3), 临床效果满意率为95%。
| 表3 每名患者术前、术后评分及恢复率 Table 3 Preoperative and postoperative scores and recovery rates (RR) in each patient |
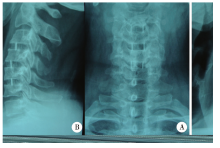
36例完全融合, 2例术后半年延迟愈合, 1例假关节形成, 但无临床症状, 融合率为97%, 平均融合时间为3.6个月(图1~4)。
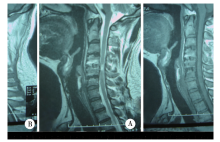
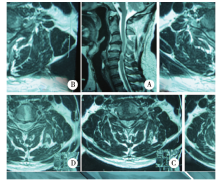 | 图2 术前MRIFigure 2 Preoperative MRI A, obvious preoperative spinal compression on the sagittal cervical T2W1 MRI; B, C34 axial MRI; C, C45 axial MRI; D, C56 axial MRI. |
本组中有1例因椎间盘钙化术后发生轻度脑脊液漏, 经换药及抬高床头, 1周后痊愈。2例患者出现轻度吞咽不适感, 分别于1周及1个月后消失。1例患者因术后引流管过细导致引流不畅, 伤口积血引起气管压迫, 术后第2天清除伤口积血, 症状消失。未见感染、融合器松动、脱出及神经症状加重等并发症。
伴有交感神经症状的颈椎病的诊断及治疗一直存在争议, 即使是其命名在文献中也有不同, 一些作者称为“ 后方交感神经综合征” 及“ Barré -Lié ou 症候群” [2, 3], 而有些称为“ 颈性眩晕” [8]或“ 颈性心绞痛” [9]。迄今为止, 由于伴有交感神经症状的颈椎病的病因及发病机制尚未清楚, 因此, 有关手术治疗鲜有报道, 保守治疗一直占统治地位, 然而保守治疗效果令人失望。近年来, 有学者尝试手术治疗伴有交感神经症状的颈椎病, 取得了良好的效果。吴广森等[5]采用前路椎体次全切除减压植骨融合术治疗23例患者, 优良率达82.6%。王新伟等[1]采用前路减压植骨内固定术治疗47例患者, 有效率达87.5%。但迄今为止, 国内尚未见PEEK辅助的ACDF术治疗伴有交感神经症状的颈椎病报道。本研究39例诊断为伴有交感神经症状的颈椎病的患者经过PEEK椎间融合器辅助的ACDF, 融合率达到97%, 这与之前的文献报道类似[10, 11]。本研究95%患者获得了优良的临床效果, 术前所有患者颈椎MRI显示明显的脊髓压迫, 基于本研究的结果可以认为, 头晕、眩晕、头痛、耳鸣、恶心呕吐、心悸、失眠及胃肠道功能失调等交感神经症状可以通过解除颈椎硬膜或后纵韧带的压迫或刺激而得到缓解。颈椎组织内富含交感神经纤维, Yamada等[12]报道颈椎硬膜及后纵韧带含有各种交感神经的支配, Kiray等[13]及Cannan等[14]发现, 颈交感干由一条主干及2~4个神经节组成, 位于横突前方, 神经节包括颈上、颈中、颈下及椎神经节, 椎神经节及其纤维包绕着椎动脉, 心脏也含有交感神经节后纤维。因此, 推测颈椎硬膜囊及后纵韧带的压迫或刺激可以引起交感神经反射, 这种反射可通过神经节和交感神经干传到节后纤维到达椎动脉及心脏等靶器官, 产生如头晕及心悸等交感神经症状。本研究患者经过ACDF 手术, 硬膜囊及后纵韧带的压迫得以解除, 交感神经症状随之缓解或消失。
关于交感神经症状的评分, 本研究采用了王新伟等[1]的20分评分法, 此评分法涵盖了几乎所有的交感神经症状, 目前应用比较广泛, 应用此评分系统评估术前及术后交感神经症状, 根据症状的严重程度及发生频率, 把交感神经症状分为20分, 这样容易比较术前及术后交感神经症状的严重性。
尽管本研究结果令人鼓舞, 但仍需要大样本手术病例的长期随访, 而且, 尚需包括动物实验及前瞻性的随机对照临床研究等大量工作来进一步研究伴有交感神经症状的颈椎病的确切病因及发病机制。
综上所述, 伴有交感神经症状的颈椎病的诊断确实存在, ACDF手术一定程度上是治疗此类病人的一种有效方法。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|