A 57-year-old male was admitted to hospital for severe headache and seizure attacks on November 6th, 2016. After radiology and spinal fluid examination, he was diagnosed with viral encephalitis and treated with antiviral medicine, antibiotics and mannitol, but he was in sustained unconsciousness and weak in expectorating. The patient was given oxygen through artificial nasal after bedside tracheotomy. At 1:00 am on January 12th, 2016, there was a sudden drop in blood pressure, heart rate and oxygen saturation with left lung breath sounds slightly lower than the other side. The patient was connected to a ventilator with tidal volume of 300-500 mL and airway pressure of 16-24 cmH2O (1 cmH2O=0.098 kPa). In the meanwhile, the left side sponge of artificial nasal was found missing. Bedside chest X-ray showed no significant atelectasis. At that time the evidence of airway foreign body aspiration was not sufficient, so no urgent bronchoscopy was performed. At 9:00 am on January 14th, 2016, there was another sudden decline in oxygen saturation with diminished left lung breath sounds and decreased left thoracic activity. Since left atelectasis could not be ruled out, bedside bronchoscopy was performed. In the operation, two sponge-like objects were found at the left main bronchus and the opening of left upper lobe bronchial. Foreign body forceps were used to remove them. The foreign bodies were proved to be the left sponge of artificial nasal afterwards. Symptoms and signs caused by aspiration of foreign body in adults were widely various and depending on the nature of the foreign body, site, time and whether there was infection or not. Foreign body aspiration caused by artificial nasal sponge was rare in clinical practice. This case was a living reminder to perform bronchoscopy when foreign body aspiration was suspected. For the unconscious and elderly patient, whose history of foreign body aspiration usually could not be clearly provided, when atelectasis was suspected, bronchoscopy should be performed progressively, and more effective measures should be taken to prevent sponge of artificial nasal displacement.
患者男性, 57岁, 主因“ 头痛、发作性抽搐14天” 于2015年11月6日入住我院神经内科病房。患者入院14天前以咽痛起病, 后逐渐出现头痛、左面肌不自主抽动, 于当地医院抗感染治疗无好转, 10天前出现抽搐、四肢强直、意识丧失, 持续5 min后意识恢复, 但之后出现神志淡漠、行为异常, 于我院神经内科门诊就诊时再发抽搐伴喷射样呕吐, 经急诊转入神经内科进一步治疗。既往有2型糖尿病病史, 口服二甲双胍, 血糖控制欠佳, 否认手术、外伤史, 否认毒物、放射物接触史。
入院体格检查:血压130/85 mmHg(1 mmHg=0.133 kPa), 心率81次/min, 神志清楚, 表情淡漠, 反应迟钝, 感觉性失语, 定向力完整, 理解力、计算力、记忆力减退, 无明确神经系统定位体征。完善相关影像学及脑脊液检查后, 诊断为病毒性脑炎、症状性癫痫、2型糖尿病, 给予患者抗病毒、抗感染、降颅压、镇静、营养支持等对症治疗, 患者抽搐次数逐渐减少, 但意识始终未恢复, 呈昏睡状态。此后, 因患者持续意识障碍, 自主咳嗽、咳痰能力弱, 反复出现痰堵, 氧合指数下降, 且存在胃内容物反流, 2015年12月19日于呼吸内科重症监护室请耳鼻喉科医师床旁局部麻醉下行气管切开术, 术后维持人工鼻吸氧3 L/min, 血氧饱和度(blood oxygen saturation, SpO2)维持于99%~100%。
2016年1月12日凌晨1:00, 患者突然出现血压、心率、SpO2下降, 血压最低76/43 mmHg, 心率最低35次/min, SpO2最低降至38%, 听诊左肺呼吸音较对侧偏低, 无明显干、湿性啰音, 予积极翻身、拍背、吸痰后SpO2回升至80%~85%(球囊辅助通气10 L/min)。血气分析检查结果:pH 7.33, 二氧化碳分压(partial pressure of carbon dioxide, pCO2)41.3 mmHg, 氧分压(partial pressure of oxygen, pO2)51.3 mmHg, 乳酸(lactate, Lac)7.3 mmol/L。予连接呼吸机辅助通气, 容量控制+间歇同步指令通气模式, (volume control ventilation + synchronized intermittent mandatory ventilation, VCV+SIMV), 逐渐调整呼吸机参数, 维持于压力支持(pressure support, PS)14 cmH2O (1 cmH2O=0.098 kPa), 呼气末正压通气(positive end expiratory pressure, PEEP)6 cmH2O, 潮气量(tidal volume, Vt)450 mL, 频率(frequency, f)10次/min, 吸入氧浓度(fraction of inspire oxygen, FiO2)60%, 患者SpO2逐渐回升至94%~96%, 监测患者自主呼吸为20~25次/min, Vt为300~500 mL, 气道压力为16~24 cmH2O。体格检查气管居中, 左侧呼吸音较前略有好转, 但较对侧仍明显偏低。后发现患者人工鼻左侧海绵消失, 仔细寻找病床及附近地面均未寻得, 行床旁X线胸片提示:气管插管末端位于主气管内, 胸3椎体水平, 未见明确肺不张表现, 右肺少许新发渗出。考虑患者气道异物证据不充分, 且每次吸痰后SpO2、左肺呼吸音均有部分改善, 故未行床旁气管镜检查。
2016年1月13日上午9:00, 患者再次出现SpO2下降, 气道内吸出大量黏痰后SpO2回升至99%~100%, 但患者左肺呼吸音逐渐减低, 左侧胸廓运动逐渐减弱, 复查床旁X线胸片较前无明显变化。
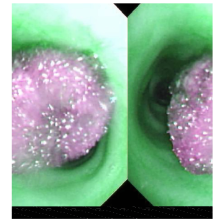
考虑患者不能完全除外左肺不张, 于2016年1月14日上午行床旁气管镜检查, 术中见左主支气管及左上叶支气管开口处各有一海绵状物体嵌顿, 以异物钳取出异物(图1)。术后患者持续呼吸机辅助通气, VCV+SIMV模式, PS 10 cmH2O, PEEP 6 cmH2O, Vt 450 mL, f 10次/min, FiO2 35%。体格检查:心率90~110次/min, 血压110~120/60~70 mmHg, SpO2 98%~100%, 患者意识仍未恢复, 左肺呼吸音较前恢复, 但较对侧仍偏低。
气道内异物为小儿常见急症, 成人因吞咽反射存在, 气管、支气管异物发生率较低, 但意识障碍的患者、老年人因吞咽反射减弱, 无法提供明确的异物吸入病史, 气道异物很容易被延迟诊断甚至误诊。回顾性研究提示, 成人气道异物常见诱因包括因酒精或镇静药使用而导致的意识改变、外伤所致的意识障碍、神经系统疾病所致的咽反射下降和牙科手术操作等[1]。
成人气道异物吸入后引起的临床症状和体征与吸入异物的性质、停留部位、停留时间和有无感染有关[2, 3], 可表现为咳嗽、呛咳、呼吸困难、发热甚至窒息。成人气道内异物多为食物源性[1], X线可穿过有机物, 这使得食物源性气道异物的诊断更为困难。X线直接征象表现为异物直接显影, 间接征象包括阻塞性肺炎、肺部肿块影、肺不张等。当X线表现不特异, 但仍高度怀疑气道异物时, CT检查可能帮助诊断与鉴别诊断。尽管相比较X线而言, CT检查具有更高的敏感性, 但特异性仍不高, 故CT仍不能确诊的病例应进行可视气管镜检查[4]。
本病例具有以下特点:(1)由于气管及主支气管解剖结构的特点, 异物多嵌顿于右主支气管及右肺下叶支气管, 但本病例经气管镜证实, 异物嵌顿于左主支气管, 临床较为少见。(2)本病例的异物最终证实为人工鼻海绵, 但该海绵本身的直径大于气管套管内径, 人工鼻海绵无外力作用而自行脱落至气道内的报道较为罕见。(3)本例人工鼻海绵误吸入气道内后断裂为两截, 分别嵌顿于左主支气管及左上叶支气管开口处。(4)本例患者仅存在左侧呼吸音降低及间断氧饱和度下降, 多次拍X线胸片未见阻塞性肺炎表现, 且连接呼吸机后气道压无异常升高, 无潮气量异常下降, 考虑原因如下:人工鼻海绵可完全透过X线, 故胸片未显影, 且海绵的透气性相对较好, 未能引起支气管完全堵塞, 故X线胸片未见肺不张表现, 气道压、潮气量未见明显改变。
总结本病例的特点提示:(1)目前人工鼻设计两侧海绵与人工气道直接相通, 可增加阻挡装置防止吸气时因气道负压导致海绵误吸入气道的发生。(2)可考虑在人工鼻两侧海绵内埋藏铅线, 以便误入体内时X线下可视。(3)具有误吸高风险的患者(如意识障碍、高龄等), 日常护理中应注意清理棉球、海绵等物品数量, 以防误吸入气道、食道。(4)由于成人气道的管径比儿童宽大, 气管及支气管随呼吸运动扩张度较大, 异物吸入后与气道壁间隙存在缝隙, 呼吸困难可能不明显。意识障碍患者气道敏感性差, 呛咳、哮鸣音的表现可能不突出[3]。对于异物吸入史不祥的意识障碍患者, 当怀疑阻塞性肺不张时, 可积极行气管镜明确气道病变情况。
支气管镜是目前诊治支气管异物的主要手段。纤维支气管镜不仅能直接发现气管内异物, 同时又能取出异物, 与传统外科开胸手术相比, 具有操作灵活简单、安全、并发症少、花费少、住院时间短等优点, 因此, 支气管镜应作为气道异物的首选治疗方法[1]。本例患者最终应用气管镜确诊海绵吸入并成功取出了异物。
目前, 支气管异物的个案报道屡见不鲜, 但人工鼻海绵误入气道的报道尚属罕见。随着纤维支气管镜技术的发展及广泛应用, 大多数患者得到了更为及时的救治。临床工作者应提高警惕, 结合临床表现及影像学特点提高对此类疾病的诊治水平, 尽量降低漏诊及误诊率。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|