Pigmented extramammary Paget’s disease (PEMPD) is an uncommon intraepithelial adenocarcinoma and a rare variant of Paget’s disease, characterized as a superficial pigmented scaly macule clinically and an increased number of melanocytes scattered between the Paget’s cells histologically. So it may be confused clinically and histologically with melanocytic tumors, dermatitis and other dermatoses. Different therapeutic attitudes are required in this case of adenocarcinoma in situ as opposed to melanoma and dermatitis. Condyloma acuminatum (CA) is a common sexually transmitted disease caused by human papilloma virus infection, which is also called as genital warts. In this article, we first reported a case of a 65-year-old Chinese man who had pigmented extramammary Paget’s disease complicated with CA. This patient presented with verrucous papules on the scrotum for 3.5 years, infiltrative erythema with itch on the mons pubis for 3 years, and scrotum and penis involved gradually for 4 months. Physical examination showed a 8 cm×10 cm dark red patch on the upper part of the scrotum, penis and mons pubis, as well as few maculopapules and nodules. Histopathologic examination of the lesion on the scrotum revealed a focus of Paget’s disease, characterized by the presence of large round cells with abundant pale or granular/dusty cytoplasm, pleomorphic vesicular nuclei and prominent nucleoli (Paget’s cells), while the histology of the verrucous lesion was consistent with CA. Immunohistochemistry was performed, which showed diffuse positive staining with CK, CEA, PAS, CK20, EMA, CK7, and Ki-67 (40%), HER2 in Paget’s cells and negative with P53, P16, CK5/6, S100, MelanA, HMB45, estrogen receptor, progesterone receptor, and gross cystic disease flid protein 15 (GCDFP-15). Human papillomavirus-11 (HPV-11) was positive by genotyping using gene amplification in the lesion of scrotum. According to clinical features and laboratory findings, a diagnosis of PEMPD complicated with CA was made. Local excision of the lesion was performed and sent for histological examination, with all margins clear of tumor. Both aforementioned diseases often occur in the vulva. Even so, it has been rarely reported coexisting of the above two diseases, of which the clinical significance and association are also unclear. In this article, we also reviewed the literature relating to PEMPD, and on this basis, the profile of this disease is discussed including its pathogenesis, clinical manifestation, diagnosis, treatment and advances. Due to PEMPD occasionally accompanied with an underlying carcinoma, it’s essential to make an accurate diagnosis. Besides, review of the literature reveals that pigmented variant of Paget’s disease could be initially misdiagnosed as melanocytic tumors and other dermatoses unless the entity is considered in the differential diagnosis and additional confirmatory studies are performed.
乳房外Paget病(extramammary Paget’ s disease, EMPD)是一种低度恶性的表皮内腺癌, 多发于中老年人, 临床表现多类似湿疹样改变, 部分可呈疣状, 不具备特异性。色素性乳房外Paget病(pigmented extramammary Paget’ s disease, PEMPD)是EMPD的一种罕见的特殊类型, 临床上表现为色素斑, 组织病理除符合Paget病特点外, Paget细胞内外常有树突状黑素细胞及黑素颗粒。尖锐湿疣(condyloma acuminatum, CA)又称生殖器疣, 是常见的由人乳头瘤病毒感染所致的性传播疾病。国内外已有数例有关EMPD合并CA的报道, 但尚未见PEMPD合并CA的报道, 二者并发的临床意义亦不清楚。本文报道1例PEMPD合并CA患者并回顾国内外相关文献, 以探究CA与PEMPD之间的联系, 提高对此病的认识。
患者, 男, 65岁, 主因“ 阴囊赘生物3年半, 阴阜红斑伴瘙痒3年, 加重4个月” 就诊。患者3.5年前无明显诱因阴囊出现多发大小不等的疣状赘生物, 无自觉症状, 就诊于北京大学人民医院皮肤科, 考虑为“ 尖锐湿疣” , 多次予外用药(鬼臼毒素酊、复方鸦胆子油中药制剂)及冷冻治疗, 皮损好转后易反复。3年前患者再次因阴囊赘生物就诊, 行皮损处组织病理检查, 术中发现阴阜处皮肤红斑, 大小约1 cm× 2 cm, 表面潮湿, 边界清楚, 追问病史, 自诉红斑处偶有瘙痒, 考虑为“ 湿疹” , 予红斑处外用激素乳膏、他克莫司及抗生素乳膏治疗。疣状皮损处组织病理确诊为CA, 外用中草药热敷疣状皮损之后, 皮损逐渐减小、消退。4个月前, 患者自觉阴阜处红斑范围增大, 累及阴囊及阴茎部分皮肤, 偶有瘙痒, 为求进一步诊治而就诊。
患者自发病以来, 无发热、全身不适等症状, 精神、饮食可, 大小便正常, 体重无明显变化。患者既往高血压20余年, 平素规律服用降压药, 血压控制可, 8年前行胆囊切除术, 否认冶游史及家族中类似疾病史。
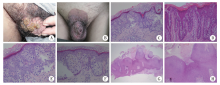
体格检查:一般情况良好, 各系统检查无异常。皮肤科检查:阴阜部、阴茎及阴囊上部可见一直径约8 cm的片状圆形暗红斑, 部分区域呈灰褐色, 边界清楚, 部分红斑触之有浸润感, 表面少许痂皮、无脱屑, 红斑上可见少量斑丘疹、结节, 未见水疱, 阴囊部亦可见表面粗糙的疣状丘疹、斑块, 部分融合(图1A、B)。双侧腹股沟及全身浅表淋巴结未触及肿大。
实验室及辅助检查:血、尿、便常规及血生化检查未见异常, 胸部X线片示双肺纹理增重, 心电图正常。腹部B超示脂肪肝, 肝内钙化灶, 大小约0.3 cm, 胆囊切除术后, 右肾囊肿, 大小约0.9 cm× 0.7 cm, 边界清, 内无彩色血流信号。阴囊、双侧睾丸和附睾B超示双侧睾丸、附睾未见明显异常, 阴囊壁表面不平滑, 回声欠均匀, 血流信号稍丰富。腹股沟淋巴结B超示双侧腹股沟多发淋巴结, 皮髓质结构清晰, 未见异常彩色血流信号。盆腔CT示前列腺增生伴点状钙化, 阴囊皮肤增厚。
分别取阴囊疣状斑块及阴阜部暗红斑皮损进行组织病理检查(图1C~H), 结果示(阴囊部)符合尖锐湿疣伴轻度非典型增生, (阴阜部)表皮内可见小巢状分布的胞浆透明的肿瘤细胞, 细胞核异型性明显, 部分细胞胞浆内可见色素颗粒。
阴阜部红斑免疫组织化学染色(图2)示:CK(+), CK7(+), CerbB-2(+), EMA(+), CEA(+), PAS(+), GCDFP-15(-), CK20(+), CK5/6(-), ER(-), PR(-), P16(-), Ki-67(40%+), P53(-), MelanA(-), HMB45(-), S-100(-)。阴囊疣状皮损人乳头瘤病毒(human papillomavirus, HPV)PCR检测为HPV-11阳性。
诊断:PEMPD合并CA。治疗:局部皮损切除术, 备皮片游离移植术。手术后组织病理示周切缘及基底切缘未见肿瘤成分。患者术后一般情况良好, 目前在随访中。
Paget病最早于1874年由Paget报道[1], 表现为女性乳房皮肤上湿疹样外观的皮损, 是一种表皮内腺癌。1889年Crocker[2]首次报道了发生于男性外生殖器上的Paget病, 即EMPD。EMPD是一种罕见的皮肤恶性肿瘤, 好发生于50岁以上的男性, 病程缓慢, 病期半年至十多年, 其损害好发于富含顶泌汗腺的区域, 如阴囊、阴茎、大小阴唇等部位。临床上皮肤损害类似于乳房Paget病, 表现为境界清楚的红斑、糜烂等湿疹样病变, 偶有疣状或结节状皮损。与Paget病不同的是, EMPD与潜在恶性肿瘤的关系似乎不大[3]。PEMPD是EMPD的罕见亚型, 色素性Paget细胞最早由Culberson等[4]于1956年报道, 此后陆续有少量类似报道。本病具有两个特点:(1)临床上表现为色素斑(比其周围皮肤颜色深); (2)组织病理上, 肿瘤细胞胞质内黑素颗粒明显增多或伴有表皮内树突状黑素细胞增多。CA是HPV所致的生殖器及肛周增生性损害, 常见的HPV亚型包括6、11、16、18型, 主要由性接触传染, 皮损表现为早期小而淡红色的丘疹, 逐渐增大、增多为疣状皮损。
本例患者阴囊处疣状皮损周围伴发境界清楚的暗红斑, 在组织病理学上, 疣状皮损呈现与CA相一致的特征, 暗红斑处表皮轻度乳头瘤样增生, 其内有多个Paget细胞, 部分肿瘤细胞内有黑素颗粒, 免疫组织化学示CK7、CEA、CK20阳性, GCDFP-15阴性, 结合临床、组织病理学及免疫组织化学检查, PEMPD合并CA诊断明确。
有研究报道在EMPD皮损基础上可发生乳头瘤样增生, 这些皮损在临床上类似CA, 需要结合组织病理学检查确诊。为研究两者的关系, Murao等[5]曾用免疫组织化学和PCR技术测定两种皮损的HPV, CA的免疫组织化学和PCR结果显示HPV阳性, 而EMPD则为阴性。Egawa等[6]报道了1例阴囊处并发CA、Bowen病及EMPD的病例, 经测定, CA皮损处HPV-6阳性, Bowen病HPV-31阳性, 而EMPD中HPV-6/11/16/18/31/33探针标记均为阴性。虽然有学者认为一些不明的EMPD相关因素有可能促进上皮细胞增生, 包括HPV相关的赘生物, 但本例患者首发表现为疣状赘生物, 且经过有效治疗后疣体逐渐消退, 而红斑面积逐渐增大。据此可推测, CA和Paget病之间可能缺乏一定的关联性, 并且由于二者的并发并不常见, 故二者并发可能仅为一种巧合。
鉴于EMPD可能与内脏器官的潜在腺癌有关, 有必要鉴别其为原发性还是继发性EMPD, 而免疫组织化学检查有助于鉴别诊断[7]。目前最常使用的原发性及继发性EMPD鉴别检查包括:CK7、CK20、CEA和巨囊性病的液状蛋白(GCDFP-15、BRST-2)[8]。研究表明, 外阴病变中CK20阳性/GCDFP-15阴性时EMPD继发于消化道腺癌的可能性大, 相反, CK20阴性/GCDFP-15阳性时继发于消化道腺癌的可能性较小[9]。本例患者红斑皮损经组织病理及免疫组织化学染色检查, 可确诊为EMPD, 为推测肿瘤细胞的来源, 继续加染GCDFP-15及CK20, 结果显示CK20阳性/GCDFP-15阴性, 倾向于肿瘤来源于内胚层, 即为继发性EMPD可能性大, 需进一步检查以排除内脏相关肿瘤。虽然该患者术前常规检查中未发现其他器官、组织明显异常, 但仍需密切随访。
PEMPD临床上色素斑的产生可能与下列因素有关[10]:(1)Paget细胞之间的树突状黑素细胞增生, 可能由肿瘤细胞释放黑素细胞趋化因子或碱性成纤维细胞生长因子(basic fibroblast growth factor, bFGF)所致; (2)Paget细胞吞噬黑素增加; (3)真皮浅层噬黑素细胞增多。本病在临床或组织病理上均易被误诊为黑素细胞相关肿瘤, 如恶性黑素瘤, 尤其是浅表播散性黑素瘤, 因此详细的体格检查以及必要的组织病理学、免疫组织化学检查有助于疾病的鉴别诊断。组织学方面, 黑素瘤细胞从表皮-真皮连接处直接浸润至真皮乳头层, 而EMPD肿瘤细胞弥散分布于表皮全层; 免疫组织化学方面, 通常PEMPD的CK7、CEA、HER2、EMA为阳性, S-100、MelanA、HMB45均为阴性, 而浅表播散性黑素瘤则相反。此外, 还需与腺样脂溢性角化病、浅表性基底细胞癌、Paget样Bowen病等鉴别, 组织病理学检查有助于鉴别诊断, 必要时可加做免疫组织化学检查。
EMPD的预后取决于多方面因素, 其中最重要的是肿瘤的浸润深度[11], 即浸润愈深, 疾病预后愈差, 此外还包括淋巴结是否肿大、淋巴结是否转移、血清中癌胚抗原(carcino-embryonic antigen, CEA)的水平及有无潜在的内脏肿瘤, 其中, 继发于内脏肿瘤的EMPD预后较差。
EMPD一经确诊, 必须尽快手术切除, 早期多采用局部广泛手术切除, 但术后局部复发率较高, 据文献报道, 外生殖器部位和肛周的术后复发率分别高达32%~50%和50%~70%[12]。目前多提倡采用Mohs外科切除技术, 不但可以彻底去除肿瘤, 同时又最大限度地保留了正常组织, 显著降低了疾病的复发率。局部放化疗或光动力治疗也可用于本病的治疗, 后者尤其适于对外观和功能要求较高、不适于手术的患者, 但其仅能缓解临床症状[11]。此外, 5%(体积分数)咪喹莫特霜、5%(体积分数)5-氟尿嘧啶(5-FU)及CO2激光也可单独或联合治疗EMPD。
综上所述, 本文报道了1例PEMPD合并CA的病例, 对于EMPD, 首先, 该病临床上可表现为疣状损害, 故外阴疣状损害, 除常见的CA外, 还需鉴别EMPD, 必要时进行组织病理学检查; 其次, EMPD合并CA, 两者似乎不具有一定的相关性, 但鉴于两者并发报道的病例不多, 故二者之间的关系尚缺乏有效的证据, 有待进一步研究证实; 第三, EMPD临床上常表现为湿疹样皮损, 易造成长期误诊, 且由于本病发病部位特殊, 部分患者因羞于就医而延误诊治, 故对于50岁以上的中、老年人发生在外生殖器部位或肛周的, 经长期治疗、经久不愈的湿疹样皮损, 应提高警惕, 考虑EMPD的可能, 活组织检查可以明确诊断, 此外, PEMPD是EMPD的罕见亚型, 无论是临床还是组织病理学均易误诊为恶性黑素瘤, 需借助免疫组织化学及特殊染色以资鉴别; 最后, EMPD可能与潜在的内脏肿瘤相关, 故需对患者进行全面系统的检查及长期密切的随访, 以期早期发现、早期诊断和早期治疗。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|