SUMMARY Multilocular prostatic cystadenoma (MPC) is a rare benign tumor that originates from the prostate itself. MPC is usually characterized by large multilocular cysts located between the rectum and bladder. The clinical presentation includes obstructive voiding symptoms, such as poor stream, intermittency, sensation of incomplete emptying, acute urinary retention and sometimes constipation symptoms due to mechanical compression of the lower intestine. Most of the previously reported patients with MPC underwent open surgery. Although the natural history of MPC remains unknown, surgical excision may not always be necessary. Here we report the case of a 49-year-old male, treated by transurethral electroresection of prostate (TURP) for prostate cyst one and half years before.His biopsy of TURP showed benign prostatic tissue with no evidence of malignancy. However, the symptoms of urinary tract obstruction were obviously aggravated after the operation. Acute urinary retention occurred intermittently 3 times. In our hospital, his total prostate specific antigen (tPSA)was 5.440 μg/L,free prostate specific antigen (fPSA ) was 1.528 μg/L. After examination, it was considered as benign lesions clearly. In the operation of TURP, we found that the tumor was multilocular cystic. Histologically,the cell was mucus. Concerning the immunophenotype,CK5/6(+), p40(+), PSA(+), P504S(+), PAX-2(-), PAX-8(-), MUC1(+), MUC5ac(+), the results of special staining were as follows: AB(+), PAS(+).At the end of the follow up 3 months later, the routine semen analysis results showed that his semen volume was 3 mL and the sperm density and sperm mobility were normal. At the end of the follow up eight months later, the patient remained free of lower urinary tract symptoms and there were no signs of recurrence. His international prostate symptom score (I-PSS) had dropped from 32 to 4, and quality of life score (QOL) had dropped from 6 to 2. MPC is a rare benign tumor originating from the prostate. TURP may aggravate the symptoms of lower urinary tract obstruction in patients with MPC, and may be temporarily observed for some asymptomatic young and middle-aged patients.
多房性前列腺囊腺瘤(multilocular prostatic cystadenoma, MPC)是一种罕见的前列腺组织来源的良性肿瘤, 肿瘤体积通常较大, 位于直肠和膀胱之间[1]。患者主要表现为泌尿系梗阻症状, 如排尿中断、尿流较细、尿不尽等。影像学检查如前列腺超声、盆腔磁共振成像不仅可以提供肿瘤的位置信息, 以及与周围器官的关系, 还有助于与其他恶性肿瘤鉴别。由于MPC罕见且缺乏长期的随访报告, 该病的诊断和治疗尚无定论。2017年 8月北京大学人民医院泌尿外科收治MPC经尿道电切术后复发 1 例, 并成功行经尿道前列腺电切术(transurethral resection of prostate, TURP), 现报告如下。
患者, 男, 49 岁, 已婚。患者于2016-10-26因体检泌尿系统超声发现前列腺占位性病变, 前列腺特异性抗原(prostate specific antigen, PSA)未见升高。患者自身无特殊不适, 未经特殊诊治。患者为明确前列腺占位性病变性质于2017-04-26在当地医院行TURP, 术后病理诊断为前列腺囊肿。术后间断有肉眼血尿, 未行规律复查。患者于2017-07-10出现急性尿潴留, 就诊当地医院行导尿、抗炎等治疗, 至就诊北京大学人民医院时已发生3次急性尿潴留, 均就诊当地医院行导尿抗炎治疗后缓解, 期间患者有排尿不尽感, 会阴部坠胀不适。患者于 2017-07-26再次于当地医院就诊, 前列腺磁共振成像(magnetic resonance imaging, MRI)显示:前列腺中央叶增大, 其左侧可见一类圆形囊性肿物, 边界清楚, 大小约 45 mm× 60 mm× 45 mm 巨大多房囊性病灶, 呈长T1长T2信号, 内见分隔, 肿物向左后方累及和压迫周围叶左侧。当地医院膀胱镜检示膀胱黏膜充血水肿, 尿道前列腺部囊性肿块, 突向膀胱内, 压迫后尿道。患者排尿困难, 留置导尿管。
患者为进一步诊治于2017年8月来北京大学人民医院就诊, 已留置尿管1周。国际前列腺症状评分(international prostate symptom score, I-PSS)为32分, 生活质量评分(quality of life score, QOL)为6分。查体:直肠指诊于前列腺区可触及巨大肿物, 横径约 5 cm, 并向肠腔内突出, 肿物上界未能触及, 中央沟消失, 质中, 表面尚光滑, 未触及结节。入院后查总前列腺特异性抗原(total prostate specific antigen, tPSA)5.440 μ g/L(ng/mL), 游离前列腺特异性抗原(free prostate specific antigen, fPSA) 1.528 μ g/L。前列腺MRI(图1)示前列腺病变术后, 前列腺正常结构消失, 左侧见一囊性信号影, 大小约5.8 cm× 4.4 cm× 5.1 cm, 其内呈长T1长T2信号改变, 见多发线性分隔, 未见明显实性成分。尿道被挤压至右侧边缘, 其右侧边缘尚可见少量前列腺组织信号。膀胱充盈欠佳, 内可见置管影。前列腺病变术后, 前列腺多房囊性病变, 实性成分不明确, 诊断为前列腺上部多房囊性病灶, 考虑良性肿瘤, 囊腺瘤并出血可能性大。
入院后完善血、尿、便常规, 凝血功能, 生化及心电图、胸片等检查, 均未见异常。患者拒绝行前列腺根治性切除术, 于2017-08-18硬膜外麻醉下行TURP。2017-08-21复查前列腺MRI(图2)示TURP术后改变, 前列腺左侧见混杂信号影, 大小约 3.9 cm× 2.5 cm× 2.7 cm, 内呈多房囊性分隔样改变, 囊性呈长T1长T2信号改变, 分隔厚薄不均, 盆腔左侧散在索条影。尿道稍右移。前列腺囊肿较术前明显减小, 尿道通畅, 原尿道右偏较前好转。1周后拔除导尿管。患者排尿通畅, 有尿失禁症状。1个月后, 患者排尿通畅, 尿失禁症状明显改善, I-PSS为1分, QOL为2分。术后随访3个月复查精液常规提示精液量 3 mL, 精子数目及活动度正常。随访8个月, I-PSS为4分, QOL为2分。排尿通畅, 未见症状复发。
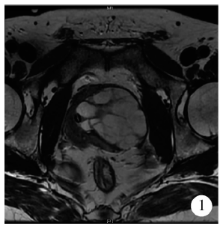 | 图1 术前(留置导尿管)MRI示尿道被压, 严重移位Figure 1 MRI of preoperation showed urethra was compressed seriously from normal position (urethral catheter was in the urethra) |
 | 图2 术后第3天MRI示尿道恢复中轴位Figure 2 MRI of postoperation showed urethra was almost in the normal position (urethral catheter was being in the urethra) |
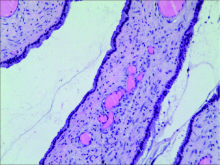
前列腺肿物切除标本术后病理(图3):送检囊壁样组织, 被覆前列腺上皮成分, 部分细胞内为黏液成分, 免疫组化染色结果示CK5/6(+)、p40(+)、PSA(+)、P504S(+)、PAX-2(-)、PAX-8(-)、MUC1(+)、MUC5ac(+), 特殊染色结果示AB(+)、PAS(+), 结合临床符合前列腺囊腺瘤, 总大小为2 cm× 1 cm× 0.8 cm。
前列腺囊腺瘤是前列腺组织来源的良性肿瘤, 迄今为止英文文献报道仅20余例, 这意味着MPC易被临床医师所忽视。目前治疗较为成功的方案主要是通过开放或者腹腔镜下切除前列腺, 但由于该病罕见且缺乏长期随访数据, 关于该病的诊断和治疗尚缺乏共识。为提高对MPC的认识, 结合北京大学人民医院进行的TURP治疗复发性MPC的尝试, 参考相关文献进行了综合分析。
该病患者28~80岁均有分布[2], 目前报道的该病临床表现多样, 主要临床表现类似于良性前列腺增生症[3], 表现为尿道梗阻和急性尿潴留, 其症状严重程度与MPC的大小和位置有关。偶有患者诉便秘症状, 这可能是由于MPC体积较大压迫直肠所致[4]。也有由于MPC压迫了射精管导致梗阻性无精子症的临床报道[5]。
术前患者血清 PSA高于正常值, 可能是由于MPC明显扩张导致部分腺管破裂而使囊液进入微血管[1, 6], 然而根据目前报道的病例, 由PSA水平尚不能推断肿瘤大小和性质[1, 6, 7, 8]。目前已经有多种检查手段可以提供该病肿物的位置和大小信息[9], 但是由于该病罕见, 如CT和MRI报告常常把该病误认为盆腔恶性肿瘤[3], 目前确诊MPC依赖组织病理学证据[10]。往往在术后病理检查时临床医师才考虑到该诊断[11], 然而在术前需要与良性前列腺增生、盆腔恶性肿瘤等鉴别[12], 这对选择合适的手术方案以及患者的预后尤为重要。
微观上, 虽然该肿瘤有较明显的细胞异型性, 但是目前尚未见该病有恶变倾向及远处转移报道[6]。完整切除通常不复发, 但若切除不完整则可能复发。根据目前报道的病例, 对于较大的、有症状的MPC的治疗应以开放或者通过腹腔镜完整手术切除为主[11], 但是由于该病患者的年龄分布范围较广, 开放或者通过腹腔镜手术切除前列腺可以避免复发, 但是却可能造成性功能丧失[13]。在前列腺癌患者中, 通过开放或者腹腔镜手术切除前列腺者术后两年的性功能保留情况低于50%[14], 对于良性肿瘤的年轻患者来说, 在明确诊断的情况下常常难以接受该术式, 然而, 对于未经外科治疗的MPC患者, 盲目采用TURP很难彻底切除肿瘤, 甚至会引起尿路梗阻症状加重。对于切除后复发无法手术切除的病例, 有文献报道用促性腺激素释放激素激动剂进行内分泌治疗后肿瘤缩小[15]。本病例第2次TURP明显改善下尿路梗阻症状, 然而, 由于患者在外院术前症状不明显, 误诊为良性前列腺增生症, 第1次行TURP术后1个月即症状复发且排尿困难症状较术前明显加重, 考虑是由于切除部分较少, 且术前尿道前列腺部尿道黏膜限制肿瘤生长并阻隔肿瘤压迫尿道, 使术后MPC“ 塌方” , 迅速生长压迫尿道。结合本病例, TURP对于未经治疗的MPC可能会引起术后下尿路梗阻症状加重, 对于部分无症状的中青年患者, 可暂行观察。
(本文编辑:王 蕾)
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|