SUMMARY Lipoid pneumonia (LP) is an uncommon form of pneumonia that is characterized by the presence of intra-alveolar lipid and lipid-laden macrophages on microscopy. It categorized as exogenous lipoid pneumonia (ExLP) and endogenous lipoid pneumonia (EnLP). Exogenous lipoid pneumonia caused by inhalation of liposuction substances (animal fat, vegetable oil, or mineral oil), mostly, in adult cases, they were medicines for constipation or rhinopharyngitis. Most of these patients showed mild clinical manifestations, and chronic medical condition. There were reports of lipoid pneumonia being successfully treated with corticosteroids, immunoglobulins and whole lung lavage. We report a case of exogenous lipoid pneumonia characterized by high fever and acute medical condition. A 77-year-old woman with hypertension and diabetes mellitus, accepted paraffin oil treatment for “incomplete intestinal obstruction”, then, an accident of aspiration happened, as she went through the history of coughing while eating, followed by persistent hyperthermia and increases of white blood cells (WBC). Chest CT showed progressive ground-glass opacities, accompanied with fusion of consolidation, her sputum etiological examination was negative, and the therapy of broad-spectrum antibiotic was invalid. The patient was subjected to bronchofibroscopy with bronchoalveolar lavage (BAL). The bronchoalveolar lavage fluid (BALF) appeared colorless and transparent, and did not show a milky appearence. Total cell count of the BALF was 2.0×105cell/mL, including 7.2% macrophages and 92.8% neutrophils. Cultures of the BALF were negative for bacterial, fungal, and mycobacterial pathogens. The BALF cytologic findings showed vacuolated lipid-laden macrophages (Oil Red O staining). These findings revealed exogenous lipoid pneumonia. There were reports of lipoid pneumonia being successfully treated with corticosteroids, immunoglobulins, and whole-lung lavage. So this patient was treated with methylprednisolone 120 mg/d for 3 days and 80 mg/d for 6 days, at the same time, immunoglobulins was given to infusion, but the daily peak temperature of the patients fluctuated between 38 and 39 degrees. Then, whole lung lavage was performed 28 days after admission. Unfortunately, acute pulmonary edema occurred during the operation, as the tracheal intubation problems, and 6 days later, the patient died at last. The clinical manifestations of exogenous lipid pneumonia vary greatly, from asymptomatic to life-threatening symptoms, and as febrile low fever is the main manifestation, but hyperthermia may also be the remarkable presentation.
脂质性肺炎(lipoid pneumonia, LP)是一种由于类脂物质在肺内集聚引起的非常见疾病[1, 2], 根据脂类物质来源不同, 可分为内源性脂质性肺炎(endogenous lipoid pneumonia)和外源性脂质性肺炎(exogenous lipoid pneumonia)。内源性脂质性肺炎又叫“ 胆固醇肺炎” 或“ 黄金肺炎” , 类脂物质由肺组织自身产生[3], 多见于未分化性结缔组织病、原发性硬化性胆管炎及肺泡蛋白沉积症[4, 5]。外源性脂质性肺炎由吸入或误吸脂类物质(动物脂肪、植物油或矿物油)引起[6], 成年患者中大多数案例见于使用油性通便药物治疗便秘或者油性滴鼻液治疗鼻咽炎[7, 8]。外源性脂质性肺炎的临床表现各异, 老年患者多为慢性、进行性、无症状的肺部炎症[9], 有临床表现的多数较轻, 以慢性咳嗽为主, 极少数患者会出现胸痛、咯血、体重减轻、间断发热等[1]。本文报道1例以高热为表现的外源性脂质性肺炎。
患者女性, 77岁, 因“ 不完全性肠梗阻” 入住中日友好医院中医消化科, 既往患高血压、糖尿病, 饮水呛咳数年, 1月前因外伤性蛛网膜下腔出血行手术治疗。入院后予禁食水、肠外营养、抗感染、石蜡油口服通便等治疗, 患者逐渐恢复排气、排便。
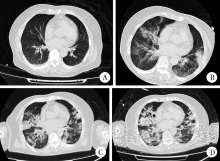
入院第8天夜间, 患者口服石蜡油时出现呛咳, 发生误吸。第9天患者开始出现高热伴嗜睡, 为稽留热表现, 全天体温均在38 ℃以上, 体温峰值进行性升高, 最高为40.8 ℃。胸部CT提示双肺磨玻璃样改变(图1)。血常规检查:白细胞10× 109~13× 109/L, 中性粒细胞百分比84%~90%, 降钙素原1.2~6.8 μ g/L。先后予头孢西丁、哌拉西林钠他唑巴坦钠(商品名:特治星)、万古霉素、亚胺培南西司他丁钠(商品名:泰能)、氟康唑等抗感染治疗(其中泰能+万古霉素联合足疗程治疗5天), 体温无明显降低。多次血培养、痰涂片、痰培养均阴性, 支气管镜检查提示各管腔通畅, 未见明显黄白痰液, 肺泡灌洗液为白色透明, 病毒、细菌、真菌、结核等病原学检查均阴性。
患者高热, 广谱抗生素治疗无效, 反复病原学检查阴性, 支气管镜检查未见感染征象, 可排除肺部感染。复查胸部CT提示双侧磨玻璃样改变进行性加重, 伴实变、融合, 实变区域可见脂肪衰减区(图1、2)。氧合指数维持在200~300 mmHg(1 mmHg=0.133 kPa)。肺泡灌洗液细胞总数20× 104/mL, 巨噬细胞7.2%, 中性粒细胞92.8%, 细胞学检查可见大量中性粒细胞及散在巨噬细胞, 细胞呈空泡状, 苏丹Ⅲ 染色阳性(图3), 考虑脂质性肺炎诊断。
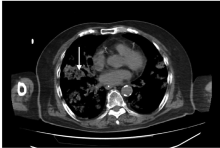 | 图2 患者胸部CT实变区域可见脂肪衰减区(箭头所示)Figure 2 CT image showed areas of fat attenuation within consolidative (arrow showed) |
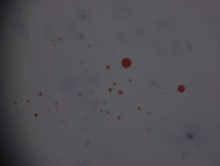 | 图3 患者肺泡灌洗液中可见空泡状巨噬细胞, 脂肪染色阳性(油红染色 × 40)Figure 3 Bronchoalveolar lavage fluid cytology showed multiple lipid-laden macrophages (Oil Red O staining × 40) |
先后予甲泼尼龙琥珀酸钠(商品名:甲强龙)120 mg/d治疗3 d, 80 mg/d治疗6 d, 患者每日体温峰值仍波动在38~39 ℃。入院第28天行全肺灌洗术一次, 疗效不佳, 术中出现急性肺水肿, 于入院第34天死亡。
外源性脂质性肺炎的诊断主要是基于油性物质暴露史、影像学改变、痰或肺泡灌洗液中见脂质沉积的巨噬细胞[10, 11]。本例患者有明确的石蜡油误吸病史, 影像学检查提示双肺磨玻璃样改变且进行性加重, 肺泡灌洗液检查可见脂质沉积的巨噬细胞, 外源性脂质性肺炎的诊断明确。
外源性脂质性肺炎多发生于儿科患者或存在虚弱、贲门失驰缓、胃食管反流或其他能引起食管及咽部神经肌肉功能失调的老年患者[4, 8, 12]。值得注意的是, 成年患者中约25%并无高危因素[9]。脂质吸入后可以损害黏液纤毛运动, 减少从呼吸道清除, 进而被肺脂肪酶乳化, 并被肺泡巨噬细胞吞噬, 启动局部炎症反应, 引起肺组织损伤[13]。外源性脂质性肺炎的临床表现不特异, 且随着患者年龄、吸入脂类物质的次数及吸入量而不同[14]。根据发病特点可分为急性外源性脂质性肺炎和慢性外源性脂质性肺炎。急性病变继发于短时间内吸入大量脂类物质, 慢性病变由长期反复吸入油脂引起[15]。本例患者虽然曾出现血白细胞和降钙素原的轻度升高, 但经广谱抗生素足疗程治疗无效, 气管镜检查管腔内未见黄脓痰, 多次病原学检查均阴性, 可除外细菌感染可能。患者发病前大量误吸石蜡油, 随后出现高热、嗜睡等表现, 为急性外源性脂质性肺炎。
急性外源性脂质性肺炎患者可出现发热、咳嗽、咳痰、白细胞升高等临床表现。吸入史、抗生素治疗无效、无全身系统性症状是提示该疾病的重要指标[13, 16, 17]。Baron等[18]通过对比、总结发现, 急性外源性脂质性肺炎患者(9例)均存在数天至数周的发热, 而慢性外源性脂质性肺炎患者(6例)均无发热表现, 但该研究中并未详细描述患者的热型及体温峰值情况。Sias等[19]报道了10例3个月到7岁的外源性脂质性肺炎患儿, 8例出现发热, 但都是低热, 无高热表现者。急性外源性脂质性肺炎的病理生理改变是肺的局部炎症反应, 临床表现的严重程度可能与一次性吸入的油脂量相关, 但由于几乎所有案例报道中均未能准确表述吸入量的情况, 尚无法证实这一猜测。
外源性脂质性肺炎临床表现差异很大, 可从无症状至严重威胁生命, 发热以低热为主要表现。由本例患者可见, 外源性脂质性肺炎的患者也可能会出现以高热为主的临床表现。
(本文编辑:任英慧)
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|