目的 了解经皮椎间孔入路内镜下神经根减压治疗单侧神经根症状的腰椎管狭窄症的可行性。方法 选择北京大学第一医院骨科2011年7月至2016年4月经皮椎间孔入路行内镜下神经根减压治疗单侧神经根症状的腰椎管狭窄症患者96例进行回顾分析和随访,患者均有单侧下肢神经根刺激症状和体征,神经源性间歇跛行小于500 m。影像学检查(CT或MRI)证实单节段腰椎退行性改变所致椎管狭窄,或多节段狭窄经诊断性神经根封闭明确为单节段狭窄所致症状,患者男55例,女41例,平均年龄(71.6±5.4)岁(47~89岁),记录术中出血量、手术时间、术中并发症、术后并发症、术后下地时间及出院时间,术前和术后随访时,采用腿痛视觉疼痛模拟(visual analogue scale, VAS)评分和Oswestry残疾指数(Oswestry disability index, ODI)评分对患者疼痛及腰部功能进行评价,应用Nakai标准评价临床疗效。结果 所有患者以环锯去除部分上关节突腹侧扩大椎间孔,内镜下使用髓核钳、射频刀头等去除盘黄间隙的黄韧带显露神经根,摘除椎间盘,进行侧隐窝及神经根管的减压,减压范围为头侧至上位椎体椎弓根下缘,尾侧至下位椎体椎弓根上缘的整个椎间孔区域。探查发现神经根无受压,水压变动时神经根搏动良好, 患者术后当天下地,无明显不适症状时出院。68例患者获得随访,平均随访时间12.1个月(6~63个月),VAS评分各测量时间点比较差异均有统计学意义( F=491.60, P<0.001),ODI评分各测量时间点比较差异均有统计学意义( F=189.91, P<0.001)。应用Nakai评价的优良率为79.4%(优42例,良12例,可10例,差4例)。1例术后出现硬膜外血肿,1例术后足下垂,6例二期行开放手术。结论 有单侧神经根刺激症状的腰椎管狭窄症患者采取椎间孔镜技术进行神经根减压,手术创伤小、恢复快,近期治疗效果满意。
Objective: To evaluate the feasibility of transforaminal endoscopic nerve root decompression for degenerative lumbar spinal stenosis (DLSS).Methods: From July 2011 to April 2016, 96 cases of single segment DLSS were involved. All the patients had unilateral lower extremity neurological symptoms, signs, neurogenic intermittent claudication of less than 500 m. Imaging examinations (CT or MRI) or diagnostic nerve root block confirmed single segment degeneration. The mean age was (71.6±5.4) years, male: 55 cases, female: 41 cases. Their intraoperative blood loss, operation time, complications, ambulation time and discharge time were recorded. Leg pain VAS, ODI were used to evaluate the pain and lumbar function of the patients. The clinical efficacy was evaluated by Nakai evaluation.Results: All the patients were performed endoscopic decompression of the lateral recess and nerve root by removing the ventral part of the superior facet joint, the ligamentum flavum and the intervertebral disc. The decompression range was from the inferior edge of the upper pedicle to the superior edge of the lower pedicle. The nerve root was detected to have no compression and the pulse of nerve root returned to normal. The patient got ambulant on the operation day and discharged if he had no discomfort symptom. In the study, 68 cases got follow up. The mean follow-up time was 12.1 months (6-63 months). The VAS at dif-ferent follow-up time points was improved relative to the baseline, and the difference was statistically significant ( F=491.60, P<0.001). The ODI at different follow-up time points was improved relative to the baseline, and the difference was statistically significant ( F=189.91, P<0.001). The excellent and good rates of Nakai evaluation were 79.4% (excellent in 42 cases, good in 12 cases, fair in 10 cases and poor in 4 cases). The mean intraoperative blood loss was (49.29±11.86) mL. The mean operation time was (92.46±21.34) min. The mean ambulation time was 1.8 h. The mean discharge time was 2.3 days. Postoperative epidural hematoma was found in 1 case. Foot drop was found in 1 case. Second stage open surgery was performed in 6 cases.Conclusion: We can apply transforaminal endoscopic decompression for the patients of lumbar spinal stenosis who have unilateral nerve root irritation. Patients with transforaminal endoscopic decompression can get less surgical trauma, quick recovery and obtain good short-term outcome.
退变性腰椎管狭窄症(degenerative lumbar spinal stenosis, DLSS)是指腰椎间盘突出、关节突增生、黄韧带肥厚等退变因素导致腰椎中央椎管、侧隐窝、神经根管狭窄, 使神经根和/或马尾神经受到刺激或压迫, 引起一系列临床症状的疾病。对于保守治疗无效的腰椎管狭窄症, 目前的主要治疗方法是腰椎管减压术, 但老年患者常伴有糖尿病、高血压、冠心病、脑梗死等合并症, 开放手术后可能出现一系列并发症[1]。目前针对腰椎间盘突出症开展的椎间孔镜下腰椎间盘切除术仅需要局部麻醉或分离麻醉, 手术创伤小、出血少, 不扰乱脊柱稳定性, 术后恢复快, 住院时间短[2, 3], 随着手术技术的不断成熟, 本课题组尝试将该手术应用于仅有单侧神经根刺激症状的腰椎管狭窄症患者, 了解椎间孔镜下神经根减压的可行性。
1.1.1 纳入标准 (1)临床症状均表现为神经根管狭窄所致神经根受压, 出现单侧下肢疼痛, 神经源性间歇性跛行小于500 m; (2)影像学检查(CT或MRI)证实, 单节段腰椎退行性改变所致椎管狭窄, 或多节段狭窄经诊断性神经根封闭明确为单节段狭窄所致症状; (3)保守治疗3个月以上无缓解。
1.1.2 排除标准 (1)重要脏器功能不全、出血倾向、精神异常者; (2)合并脊柱感染、肿瘤、骨折者; (3)马尾综合征患者; (4)二次手术患者。
选择北京大学第一医院骨科2011年7月至2016年4月腰椎管狭窄症患者行椎间孔镜下单侧神经根减压术96例进行回顾分析和随访, 男55例, 女41例, 平均年龄(71.6± 5.4)岁(47~89岁)。
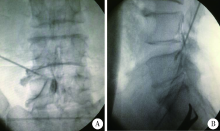
术前结合症状、查体、影像学检查明确责任节段, 如节段难以确定则行可疑节段神经根封闭协助诊断(图1)。
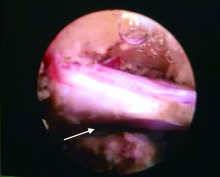
椎间孔镜手术技术要点:局部麻醉或分离腰麻[0.17%(质量分数)罗哌卡因6 mL)]后, 患者俯卧位, C臂监视下将穿刺针置入患侧手术节段椎间孔, 取出穿刺针内芯置入导丝, 逐级套筒扩开软组织通道, 逐级环锯去除部分上关节突腹侧部分(图2), 扩大椎间孔并行侧隐窝减压, 将工作通道置入椎管, 清除增厚的黄韧带, 于硬膜前间隙直视下取出椎间盘组织, 侧隐窝扩大成形, 探查头侧椎弓根下缘至尾侧椎弓根上缘间行走神经根无受压、水压变动时神经根搏动良好(图3), 取出椎间孔镜及工作通道, 缝合切口, 术后行MRI检查了解减压情况(图4)。
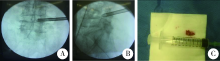 | 图2 置入工作通道(A、B), 放置通道过程中磨除的关节突(C)Figure 2 Insert the work channel (A and B), bone taken off from the superior facet joint (C) |
 | 图4 MRI椎管减压术后椎管面积大于术前椎管面积Figure 4 The area of postoperation was larger than that of preoperation on MRI.A, preoperation; B, postoperation. |
术后处理:患者术后当天下地, 无明显不适症状时出院, 如症状缓解不明显予以药物、理疗等保守治疗或开放手术。
记录术中出血量、手术时间、术中并发症、术后并发症、术后下地及出院时间。记录患者术前和术后随访时腿痛视觉疼痛模拟(visual analogue scale, VAS)评分和Oswestry残疾指数(Oswestry disability index, ODI)评分, 对患者疼痛及腰部功能进行评价, 疗效评价根据Nakai评分评价标准分为优、良、可、差4级。
采用SPSS18.0统计软件, 计量资料用均数± 标准差描述, 比较采用配对t检验, 双侧检验, P< 0.05认为差异有统计学意义。
共完成手术96例, 其中L3/4节段14例, L4/5节段44例, L5/S1节段38例。68例患者获得随访, L3/4节段8例, L4/5节段36例, L5/S1节段24例, 平均随访时间12.1个月(6~63个月)。
术后各时间点相对于术前VAS和ODI评分均有改善(表1), 对VAS评分各个测量时间点采用重复测量方差分析, 差异均有统计学意义(F=491.60, P< 0.001); 对ODI评分各个测量时间点采用重复测量方差分析, 差异均有统计学意义(F=189.91, P< 0.001)。应用Nakai评价的优良率为79.4%(优42例, 良12例, 可10例, 差4例), 6例二期行开放手术。
| 表1 VAS和ODI评分手术前后各随访时间点变化情况( |
1例患者长期服用阿司匹林, 术前停药3 d, 术后第3天出现症状反复伴健侧足背伸力弱, 复查MRI发现手术节段硬膜外血肿(图5), 二次手术行腰椎管减压, 术后症状缓解; 1例术后足下垂, 对症治疗8周后恢复。术中出血量、手术时间、术后下地时间和出院时间分别为(49.29± 11.86) mL、(92.46± 21.34) min、1.8(1, 12) h和2.3(1, 12) d。
腰椎管狭窄症的治疗过程中, 保守疗法对患者有一定的疗效, 但部分保守治疗无效的患者最终还是选择手术治疗。目前对于腰椎管狭窄症的手术治疗主要还是开放手术进行椎管减压, 解除神经压迫, 必要时进行内固定融合以保持脊柱稳定性, 但很多老年患者合并症较多, 不能耐受常规开放手术。
Yeung[4]首创了经Kambin 安全三角区进入椎间盘内行间接椎间盘减压的YESS(Yeung endosco-pic spine system)技术用于腰椎间盘突出症的治疗。Schubert等[5]在YESS技术基础上提出THESSYS(thomas hoogland endoscopic spine system)技术用于腰椎间盘突出症的治疗, 通过逐级切除下位椎体的部分上关节突腹侧骨质结构, 扩大椎间孔, 将手术工作导管直接置入椎管, 使共轴内镜能直达突出椎间盘, 在内镜直视下, 经硬脊膜前间隙可直接取出脱出或游离的腰椎间盘组织, 目前这些技术在国内外广泛开展, 取得了良好的疗效[2, 3]。
腰椎管狭窄症根据狭窄部位分为中央管狭窄、侧隐窝狭窄及神经根管狭窄。侧方黄韧带肥厚、关节突增生及椎间盘突出可造成侧隐窝狭窄及神经根管狭窄, 引起神经根刺激症状, 常表现为单侧下肢放射性疼痛、间歇性跛行。目前的椎间孔镜技术在置入工作通道及内镜前要用环锯逐级去除部分上关节突扩开椎间孔, 置入内镜后, 可在镜下使用髓核钳、射频刀头等去除盘黄间隙的黄韧带显露神经根, 并可摘除椎间盘, 从而进行侧隐窝及神经根管的减压, 已有学者尝试将该技术用于老年腰椎管狭窄症患者的治疗[6, 7]。本研究采用椎间孔镜技术进行神经根减压治疗单侧神经根症状的腰椎管狭窄症, 在严格把握手术适应证的前提下, 对有单侧神经根刺激症状的腰椎管狭窄症患者采取内镜下减压, 手术采用局麻或分离腰麻, 术中使用环锯向椎间孔背侧去除部分下位椎体上关节突, 将通道开口置于椎管内黄韧带表面, 显露增厚并覆盖于神经根表面的黄韧带, 以髓核钳取出神经根背侧的黄韧带及腹侧的椎间盘行神经根的“ 270° ” 减压, 减压范围为头侧至上位椎体椎弓根下缘, 尾侧至下位椎体椎弓根上缘的整个椎间孔区域, 手术创伤小, 不影响手术节段稳定性, 可获得近期良好治疗效果, 优良率达79.4%。
在使用椎间孔镜技术进行神经根减压过程中, 也要注意避免内镜手术的相关并发症[8, 9, 10], 术前应对患者一般状况进行评估, 疼痛不适等可增加老年患者心脑血管意外的发生率, 术中可通过局麻或分离麻醉缓解手术引起的患者不适; 术前需明确责任病灶, 必要时先进行可疑病灶节段神经根封闭进一步明确诊断以保证手术的精确减压; 熟悉椎间孔周围结构的解剖, 手术中要注意穿刺、环锯扩开椎间孔及镜下切除黄韧带、椎间盘等操作中避免损伤硬膜囊、出行神经根及走行神经根。本研究1例足下垂即考虑为工作通道卡压出行神经根所致, 经药物治疗后, 足下垂在术后2个月时恢复; 另1例长期抗凝治疗患者术后出现症状性硬膜外血肿行开放手术减压后缓解, 因此对于长期使用抗凝、抗血小板药物的患者要注意调整用药, 术中使用射频刀头严密止血, 以防出血渗入狭窄的椎管内造成硬膜外血肿。
椎间孔镜技术对于退变性腰椎管狭窄症的治疗有其局限性, 可用于有根性症状的侧隐窝或神经根管狭窄的患者, 不适于中央管狭窄所致临床症状的患者[11, 12], 本研究术后症状改善不明显的患者主要为中央管狭窄明显、压迫范围广泛、术中神经减压效果不佳所致, 另外本研究病例数较少、缺乏长期随访结果, 虽术后短期取得满意疗效, 远期是否会出现关节突进一步退变增生压迫神经根或硬膜囊导致症状重新出现尚待进一步观察, 因此, 今后应进一步改进技术, 增加手术病例, 继续随访观察该手术的疗效。
综上所述, 采用椎间孔镜技术进行神经根减压创伤小、术后恢复快, 短期内对于有根性症状的退变性腰椎管狭窄症患者的治疗可取得满意疗效, 是退变性腰椎管狭窄症患者, 尤其是不能耐受开放减压手术患者的一种治疗选择。
(本文编辑:王 蕾)
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|