Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (5): 923-927. doi: 10.19723/j.issn.1671-167X.2024.05.027
Previous Articles Next Articles
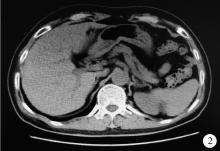
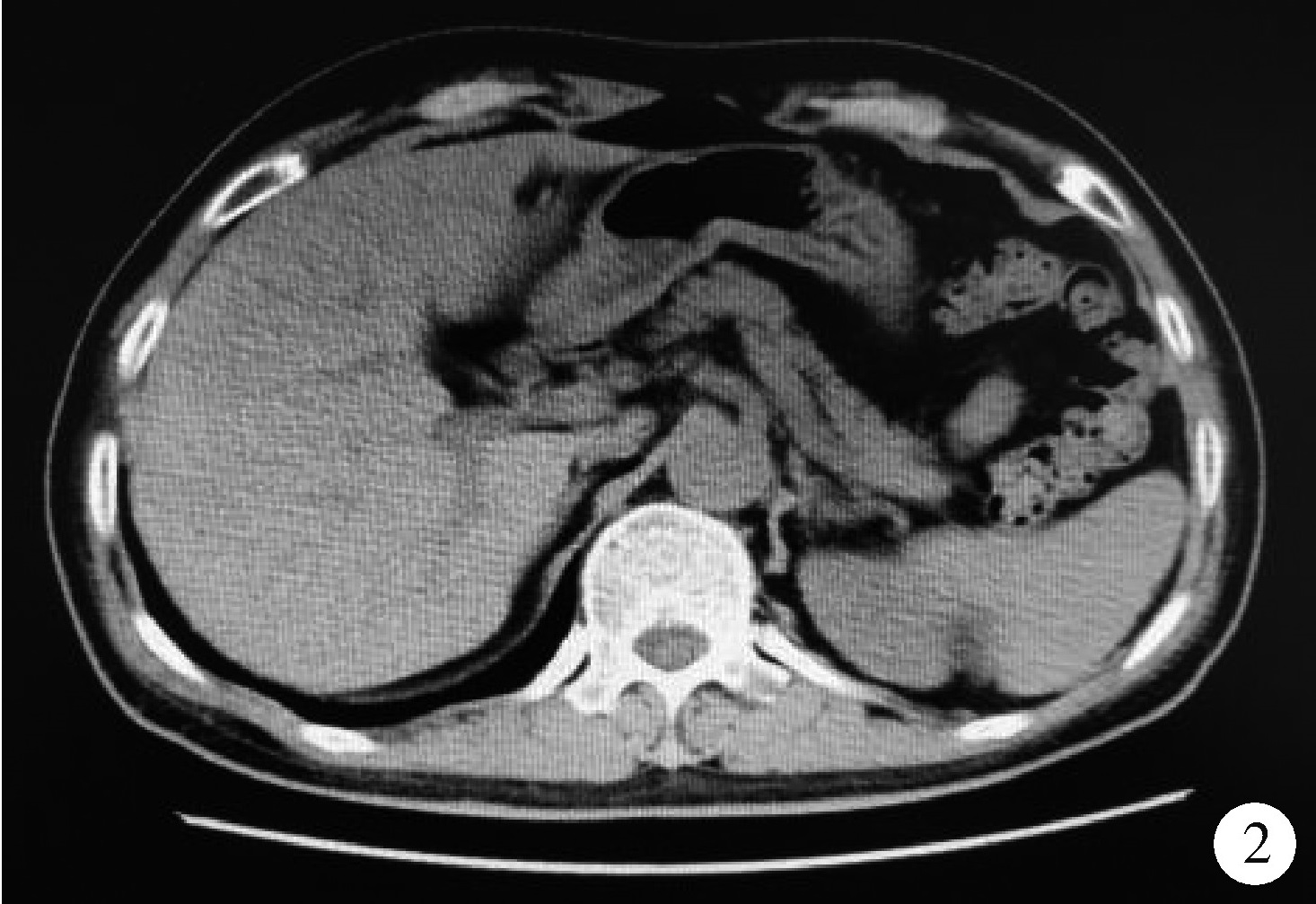
Fulminant type 1 diabetes mellitus with acute pancreatitis: A case report and literature review
Peiheng ZHANG, Ying GAO, Honghua WU, Jian ZHANG*( ), Junqing ZHANG
), Junqing ZHANG
- Department of Endocrinology, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R587.1
| 1 |
Imagawa A , Hanafusa T , Miyagawa JI , et al. A novel subtype of type 1 diabetes mellitus characterized by a rapid onset and an absence of diabetes-related antibodies. Osaka IDDM Study Group[J]. N Engl J Med, 2000, 342 (5): 301- 307.
doi: 10.1056/NEJM200002033420501 |
| 2 | 柳岚, 曾玲, 桑丹, 等. 暴发性1型糖尿病研究新进展[J]. 中国糖尿病杂志, 2018, 26 (5): 431- 436. |
| 3 |
Luo S , Zhang Z , Li X , et al. Fulminant type 1 diabetes: A collaborative clinical cases investigation in China[J]. Acta Diabetol, 2013, 50 (1): 53- 59.
doi: 10.1007/s00592-011-0362-1 |
| 4 | 李照青, 张金苹. 暴发性1型糖尿病患者的患病情况及临床特征[J]. 中华内科杂志, 2016, 55 (11): 849- 853. |
| 5 | 郑超, 林健, 杨琳, 等. 暴发性1型糖尿病的患病状况及其特征[J]. 中华内分泌代谢杂志, 2010, 26 (3): 188- 191. |
| 6 |
Imagawa A , Hanafusa T , Awata T , et al. Report of the Committee of the Japan Diabetes Society on the research of fulminant and acute-onset type 1 diabetes mellitus: New diagnostic criteria of fulminant type 1 diabetes mellitus (2012)[J]. J Diabetes Investig, 2012, 3 (6): 536- 539.
doi: 10.1111/jdi.12024 |
| 7 |
Sakurai K , Niitsuma S , Sato R , et al. Painless thyroiditis and fulminant type 1 diabetes mellitus in a patient treated with an immune checkpoint inhibitor, nivolumab[J]. Tohoku J Exp Med, 2018, 244 (1): 33- 40.
doi: 10.1620/tjem.244.33 |
| 8 |
Imagawa A . Two types of fulminant type 1 diabetes mellitus: Immune checkpoint inhibitor-related and conventional[J]. J Diabetes Investig, 2021, 12 (6): 917- 919.
doi: 10.1111/jdi.13450 |
| 9 | Kyriacou A , Melson E , Chen W , et al. Is immune checkpoint inhibitor-associated diabetes the same as fulminant type 1 diabetes mellitus?[J]. Clin Med (Lond), 2020, 20 (4): 417- 423. |
| 10 | 中华医学会急诊分会, 京津冀急诊急救联盟, 北京医学会急诊分会, 等. 急性胰腺炎急诊诊断及治疗专家共识[J]. 中华急诊医学杂志, 2021, 30 (2): 161- 172. |
| 11 | Rawla P , Bandaru SS , Vellipuram AR . Review of infectious etiology of acute pancreatitis[J]. Gastroenterology Res, 2017, 10 (3): 153- 158. |
| 12 | Chatila T , Bilal M , Guturu P . Evaluation and management of acute pancreatitis[J]. World J Clin Cases, 2019, 7 (9): 1006- 1020. |
| 13 | Yoneda S , Imagawa A , Fukui K , et al. A histological study of fulminant type 1 diabetes mellitus related to human cytomegalovirus reactivation[J]. J Clin Endocrinol Metab, 2017, 102 (7): 2394- 2400. |
| 14 | Luo S , Ma X , Li X , et al. Fulminant type 1 diabetes: A comprehensive review of an autoimmune condition[J]. Diabetes Metab Res Rev, 2020, 36 (6): e3317. |
| 15 | Imagawa A , Hanafusa T , Miyagawa J , et al. A proposal of three distinct subtypes of type 1 diabetes mellitus based on clinical and pathological evidence[J]. Ann Med, 2000, 32 (8): 539- 543. |
| 16 | Obata A , Kaneto H , Kamei S , et al. Pancreatic inflammation captured by imaging technology at the onset of fulminant type 1 diabetes[J]. Diabetes Care, 2015, 38 (9): e135- e136. |
| 17 | Nakajima M , Shirokawa M , Nakano T , et al. Fulminant type 1 diabetes mellitus with remarkable elevation of serum pancreatic enzymes[J]. Am J Emerg Med, 2018, 36 (7): e1323- e1326. |
| 18 | Yabe D , Kuroe A , Ohya M , et al. A case of fulminant type 1 diabetes mellitus with exocrine pancreatic insufficiency and enhanced glucagon response to meal ingestion[J]. Diabetes Res Clin Pract, 2008, 82 (2): e1- e4. |
| 19 | Chen Y , Zhao M , Cui J , et al. Acute pancreatitis may be a pathogenic factor of fulminant type 1 diabetes mellitus[J]. Chin Med J (Engl), 2020, 134 (9): 1127- 1128. |
| 20 | Imagawa A , Hanafusa T . Fulminant type 1 diabetes-an important subtype in East Asia[J]. Diabetes Metab Res Rev, 2011, 27 (8): 959- 964. |
| 21 | Tanaka S , Aida K , Nishida Y , et al. Pathophysiological mechanisms involving aggressive islet cell destruction in fulminant type 1 diabetes[J]. Endocr J, 2013, 60 (7): 837- 845. |
| 22 | 陈文俊, 叶文慧, 麦华超. 以急腹症起病的暴发性1型糖尿病一例[J]. 临床内科杂志, 2021, 38 (4): 277- 278. |
| [1] | ZHUANG Jin-man,LI Tian-run,LI Xuan,LUAN Jing-yuan,WANG Chang-ming,FENG Qi-chen,HAN Jin-tao. Application of Rotarex mechanical thrombectomy system in acute lower limb ische-mia [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1159-1162. |
| [2] | LI Hong-liang, JIANG Yuan-hui, WEI Yuan, ZHAO Yang-yu, ZHU Xi, YAO Gai-qi. Clinical analysis of acute hyperlipidemic pancreatitis during pregnancy and postpartum period [J]. Journal of Peking University(Health Sciences), 2014, 46(1): 125-129. |
|
||