Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (6): 1140-1145. doi: 10.19723/j.issn.1671-167X.2020.06.026
Previous Articles Next Articles
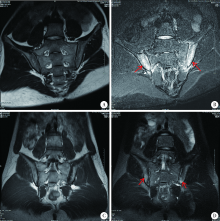
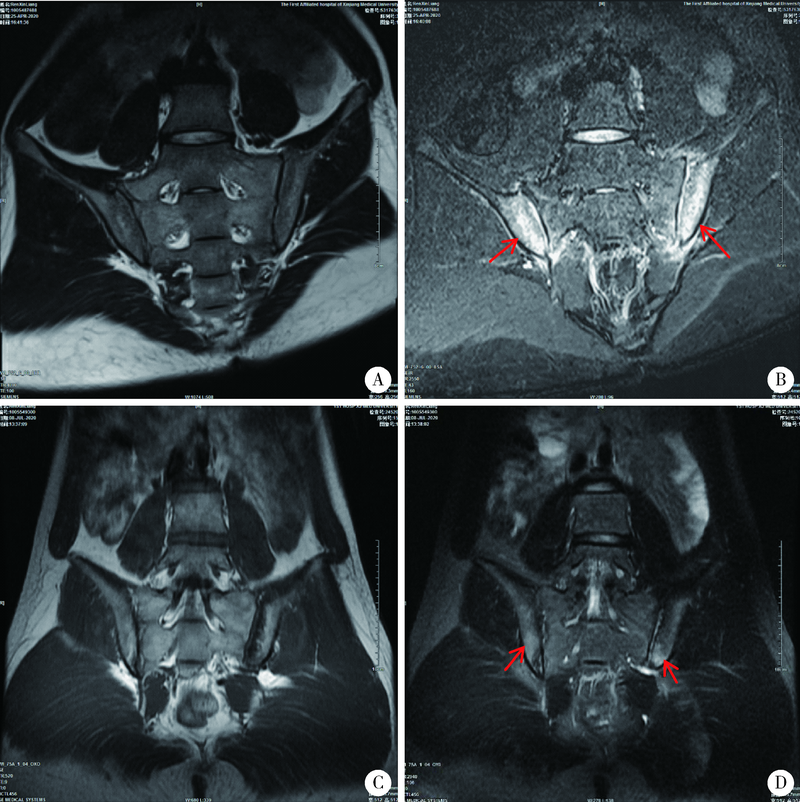
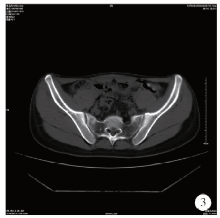
Chronic multifocal osteomyelitis: A case report and literature review
Yong-wei HU1,Rui LIU2,△( ),Li LUO1,△(
),Li LUO1,△( )
)
- 1. Department of Rheumatology, the First Affiliated Hospital of Xinjiang Medical University, Urumchi 8300542, China
2. Department of Rheumatology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R681.2
| [1] |
Master SL, Simon A, Aksentijevich I, et al. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease[J]. Annu Rev Immunol, 2009,27:621-668.
doi: 10.1146/annurev.immunol.25.022106.141627 pmid: 19302049 |
| [2] | 余可谊, 沈敏. 自身炎症性骨病[J]. 中华医学杂志, 2016,96(15):1230-1232. |
| [3] |
Jansson A, Renner ED, Ramer J, et al. Classification of nonbacterial osteitis: rttrospective study of clinical, immunological and genetic in 89 patients[J]. Rheumatology, 2007,46(1):154-160.
doi: 10.1093/rheumatology/kel190 pmid: 16782988 |
| [4] |
Sciannro R, Insalaco A, Bracci LL, et al. Deregulation of the IL-1β axis in chronic recurrent multifocal osteomyelitis[J]. Pediatr Rheumatol Online J, 2014,7(17):12-30.
doi: 10.1186/1546-0096-7-12 |
| [5] | 吴凤岐. 再认识全身型幼年特发性关节炎[J]. 中华实用儿科临床杂志, 2014,11(29):1607-1610. |
| [6] |
Greenwood S, Leone A, Cassar-Pullicino VN. SAPHO and recurrent multifocal osteomyelitis[J]. Radiol Clin North Am, 2017,55(5):1035-1053.
pmid: 28774447 |
| [7] |
Sato H, Wada Y, Hasegawa E, et al. Adult-onset chronic recurrent multifocal osteomyelitis with high intensity of muscles detected by magnetic resonance imaging, successfully controlled with tocilizumab[J]. Intern Med, 2017,56(17):2353-2360.
doi: 10.2169/internalmedicine.8473-16 pmid: 28794369 |
| [8] |
Earwaker JW, Cotten A. SAPHO: Syndrome or concept? Imaging findings[J]. Skeletal Radiol, 2003,32(6):311-327.
doi: 10.1007/s00256-003-0629-x pmid: 12719925 |
| [9] | Inoue K, Yamaguchi T, Ozawa H, et al. Diagnosing active inflammation in the SAPHO syndrome using 18FDG-PET/CT in suspected metastatic vertebral bone tumors[J]. Ann Nucl Med, 2007,2l(8):477-480. |
| [10] |
Takeuchi K, Matsusita M, Takagishi K. A case of SAPHO (synovitis-acne-pustulosis-hyperostosis-osteomyelitis) syndrome in which [18F]fluorodeoxyglucose positron emission tomography was useful for differentiating from multiple metastatic bone tumors[J]. Mod Rheumatol, 2007,17(1):67-7l.
doi: 10.1007/s10165-006-0536-9 |
| [11] |
Morbach H, Hedrich CM, Beer M, et al. Autoinflammatory bone disorders[J]. Clin Immunol, 2013,147(3):185-196.
doi: 10.1016/j.clim.2012.12.012 |
| [12] |
Sharma M, ferguson PJ. Autoinflammatory bone disorders: update on immunologic abnormalities and clues about possible triggers[J]. Curr Opin Rheumatol, 2013,25(5):658-664.
doi: 10.1097/BOR.0b013e328363eb08 |
| [13] |
Maria FG, Mario D, Carmela G, et al. Chronic recurrent multifocal osteomyelitis: a case report[J]. Ital J Pediatr, 2018,44(1):26.
pmid: 29454377 |
| [14] |
Wipff J, Adamsbaum C, Kahan A, et al. Chronic recurrent multifocal osteomyelitis. Joint Bone Spine[J]. Joint Bone Spine Revue Du Rhumatisme, 2011,78(6):555-560.
doi: 10.1016/j.jbspin.2011.02.010 |
| [15] | Petty RE. Textbook of pediatric rheumatology[M]. 7th ed. Philadelphia: Elsevier, 2016: 406-417. |
| [16] |
von Kalle T, Heim N, Hospach T, et al. Typical pattern of bone involvement in whole-body MRI of patients with chronic recurrent multifocal osteomyelitis (CRMO)[J]. Rofo, 2013,185(7):655-661.
doi: 10.1055/s-0033-1335283 pmid: 23696017 |
| [17] | Ramraj R, Chun C, Marcovici P. Chronic Recurrent Multifocal Osteomyelitis in Crohn Disease: Complete Resolution With Anti-TNFα Therapy[J]. J Pediatr Gastrointestinal Nutr, 2018,67(3):e57. |
| [18] |
Roderick MR, Shah R, Rogers V, et al. Chronic recurrent multifocal osteomyelitis (CRMO): advancing the diagnosis[J]. Pediatr Rheumatol Online J, 2016,14(1):47.
doi: 10.1186/s12969-016-0109-1 pmid: 27576444 |
| [19] |
Jansson AF, Müller TH, Gliera L, et al. Clinical score for nonbacterial osteitis in children and adults[J]. Arthritis Rheum, 2009,60(4):1152-1159.
doi: 10.1002/art.24402 pmid: 19333943 |
| [20] |
Bousvaros A, Marcon M, Treem W, et al. Chronic recurrent multifocal osteomyelitis associated with chronic inflammatory bowel disease in children[J]. Dig Dis Sci, 1999,44(12):2500-2507.
pmid: 10630504 |
| [21] |
Wipff J, Costantino F, Lemelle I, et al. A large national cohort of French patients with chronic recurrent multifocal osteitis[J]. Arthritis Rheumatol, 2015,67(4):1128-1137.
doi: 10.1002/art.39013 pmid: 25545761 |
| [22] | 赵梦珠, 余可宜, 沈敏, 等. 慢性无菌性骨髓炎8例及文献复习[J]. 中华临床免疫和变态反应杂志, 2019,4(13):118-124. |
| [23] |
Zhao Y, Wu EY, Oliver MS, et al. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions[J]. Arthritis Care Res (Hoboken), 2018,70(8):1228-1237.
doi: 10.1002/acr.2018.70.issue-8 |
| No related articles found! |
|
||