Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (6): 1056-1061. doi: 10.19723/j.issn.1671-167X.2019.06.014
Previous Articles Next Articles
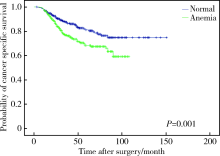
Evaluating the impact of preoperative anemia on the prognosis of upper tract urothelial carcinoma following radical nephroureterectomy: A single-center retrospective study of 686 patients
Bao GUAN1,Mai WENG2,Hang FAN2,Ding PENG1,Dong FANG1,Geng-yan XIONG1,Xue-song LI1,△( ),Li-qun ZHOU1
),Li-qun ZHOU1
- 1. Department of Urology, Peking University First Hospital, Beijing 100034, China
2. Department of Urology, Beijing Armed Police Corps Hospital, Beijing 100039, China
CLC Number:
- R730.261
| [1] | Feng C, Wang L, Ding G , et al. Predictive value of clinicopathological markers for the metachronous bladder cancer and prognosis of upper tract urothelial carcinoma[J]. Sci Rep, 2014,4(6):4015. |
| [2] | Mehta R, Gillan AS, Ming ZY , et al. Socio-economic deprivation and outcomes following radical nephroureterectomy for clinically localized upper tract transitional cell carcinoma[J]. World J Urol, 2015,33(1):41-49. |
| [3] | Ishioka J, Saito K, Kijima T , et al. Risk stratification for bladder recurrence of upper urinary tract urothelial carcinoma after radical nephroureterectomy[J]. BJU Int, 2015,115(5):705-712. |
| [4] | Hamada S, Horiguchi A, Asano T , et al. Prognostic impact of fatty acid synthase expression in upper urinary tract urothelial carcinoma[J]. Jpn J Clin Oncol, 2014,44(5):486-492. |
| [5] | Rink M, Sharifi N, Fritsche HM , et al. Impact of preoperative anemia on oncologic outcomes of upper tract urothelial carcinoma treated with radical nephroureterectomy[J]. J Urol, 2014,191(2):316-322. |
| [6] | Krabbe LM, Westerman ME, Bagrodia A , et al. Surgical management of the distal ureter during radical nephroureterectomy is an independent predictor of oncological outcomes: results of a current series and a review of the literature[J]. Urol Oncol, 2014,32(1):54e19-54e26. |
| [7] | Chromecki TF, Cha EK, Fajkovic H , et al. The impact of tumor multifocality on outcomes in patients treated with radical nephroureterectomy[J]. Eur Urol, 2012,61(2):245-253. |
| [8] | Nutritional anaemias . Report of a WHO scientific group[J]. World Health Organ Tech Rep Ser, 1968,405:5-37. |
| [9] | Epstein JI, Amin MB, Reuter VR , et al. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee[J]. Am J Surg Pathol, 1998,22(12):1435-1448. |
| [10] | Greene FL, Sobin LH . A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC[J]. J Surg Oncol, 2009,99(5):269-272. |
| [11] | Yeh HC, Chien TM, Wu WJ , et al. Is preoperative anemia a risk factor for upper tract urothelial carcinoma following radical nephroureterectomy?[J]. Urol oncol, 2016,34(8):337e331-337e339. |
| [12] | Lu YM, Li CC, Wu WJ , et al. Patients’ renal function is important when evaluating preoperative anemia in upper tract urothelial carcinoma[J]. Clin Genitourin Cancer, 2016,14(2):e241-e243. |
| [13] | Gilreath JA, Stenehjem DD, Rodgers GM . Diagnosis and treatment of cancer-related anemia[J]. Am J Hematol, 2014,89(2):203-212. |
| [14] | Gaspar BL, Sharma P, Das R . Anemia in malignancies: pathogenetic and diagnostic considerations[J]. Hematology, 2015,20(1):18-25. |
| [1] | Chang SHU,Ye HAN,Yuzhe SUN,Zaimu YANG,Jianxia HOU. Changes of parameters associated with anemia of inflammation in patients with stage Ⅲ periodontitis before and after periodontal initial therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 45-50. |
| [2] | Wei WANG,Jia-ning WANG,Wei YU,Sai-nan ZHU,Ying GAO,Jun-qing ZHANG. Comparison of coagulation function between adrenocorticotropic hormone independent Cushing syndrome and nonfunctional adrenal adenoma and its influence factors [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1062-1067. |
| [3] | Yong-wei LIN,Ya-lin ZHOU,Run-long ZHAO,Ya-jun XU,Yan-ping LIU. Analysis on the iron status and associated factors during the first trimester of pregnancy [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 600-605. |
| [4] | Zhi-hua LI,Chun-ru XU,Yin LIU,Hua GUAN,Meng ZHANG,Xin-yan CHE,Qi TANG,Yan-bo HUANG,Xue-song LI,Li-qun HOU. Correlation between daily fluid intake behavioral habits and pathological characteristics of upper tract urothelial carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 621-627. |
| [5] | Xiang DAI,Fei WANG,Yi-qing DU,Yu-xuan SONG,Tao XU. Correlation between adipokine and clinicopathological features and prognosis in upper tract urothelial carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 605-614. |
| [6] | FAN Li-shi,GAO Min,Edwin B. FISHER,SUN Xin-ying. Factors associated with quality of life in 747 patients with type 2 diabetes in Tongzhou District and Shunyi District of Beijing [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 523-529. |
| [7] | Run-zhuo MA,Hai-zhui XIA,Min LU,Zhi-ying ZHANG,Qi-ming ZHANG,Jian LU,Guo-liang WANG,Lu-lin MA. Impact of diagnostic ureteroscopy and biopsy on radical nephroureterectomy of upper tract urothelial carcinoma [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 665-672. |
| [8] | YANG Chao, WANG Jin-wei, YANG Yao-zheng, BAI Kun-hao, GAO Bi-xia, ZHAO Ming-hui, ZHANG Lu-xia, WU Shou-ling, WANG Fang. Impact of anemia and chronic kidney disease on the risk of cardiovascular disease and all-cause mortality among diabetic patients [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 495-500. |
| [9] | LIU Xiao-yu, YANG Xiao-qing, XIAO Hui-jie, DING Jie. Comparison between continuous noninvasive hemoglobin monitoring and venous blood hemoglobin monitoring in children with kidney disease [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 778-782. |
| [10] | GUAN Bao, CAO Zhen-peng, PENG Ding, LI Yi-fan, ZHAN Yong-hao, LIU Li-bo, HE Shi-ming, XIONG Geng-yan, LI Xue-song, ZHOU Li-qun. Prognostic factors of patients with T2N0M0 upper tract urothelial carcinoma: a single-center retrospective study of 235 patients [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 603-607. |
| [11] | CAO Ya-ying, TANG Xun, SUN Ke-xin, LIU Zhi-ke, XIANG Xiao, JUAN Juan, SONG Jing, YIN Qiong-zhou, ZHAXI De-ji, HU Ya-nan, YANG Yan-fen, SHI Mo-ye, TIAN Yao-hua, HUANG Shao-ping, . Relationship between glycemic control and visceral adiposity index among the patients with type 2 diabetes mellitus [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 446-450. |
| [12] | SONG Yi, ZHANG Bing, HU Pei-jin, MA Jun. Prevalence of anemia and its association with nutritional status among Chinese students of ethnic minorities in 2010 [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 429-435. |
| [13] | LIU Dan, Li-Ru, LIU Jia-Yu, YAO Hai-Hong, CHEN Qing-Ping, JIA Yuan, SU Yin- . Clinical characteristics and treatment outcomes of microscopic polyangiitis combined with autoimmune hemolytic anemia [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 657-660. |
| [14] | SUN Ke-Xin, LIU Zhi, CAO Ya-Ying, JUAN Juan, XIANG Xiao, YANG Cheng, HUANG Shao-Ping, LIU Xiao-Fen, LI Na, TANG Xun, LI Jin, WU Tao, CHEN Da-Fang, HU Yong-Hua- . Relationship between brachial-ankle pulse wave velocity and glycemic control of type 2 diabetes mellitus patients in Beijing community population [J]. Journal of Peking University(Health Sciences), 2015, 47(3): 431-436. |
|
||