Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 692-696. doi: 10.19723/j.issn.1671-167X.2021.04.012
Previous Articles Next Articles
Relationship between prostate apex depth and early recovery of urinary continence after laparoscopic radical prostatectomy
ZHANG Fan,HUANG Xiao-juan,YANG Bin,YAN Ye,LIU Cheng,ZHANG Shu-dong,HUANG Yi( ),MA Lu-lin
),MA Lu-lin
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.25
| [1] |
Siegel RL, Miller KD, Fuchis HE, et al. Cancer statistics, 2021 [J]. CA Cancer J Clin, 2021, 71(1):7-33.
doi: 10.3322/caac.v71.1 |
| [2] |
Wong MC, Goggins WB, Wang HH, et al. Global incidence and mortality for prostate cancer: Analysis of temporal patterns and trends in 36 countries [J]. Eur Urol, 2016, 70(5):862-874.
doi: 10.1016/j.eururo.2016.05.043 |
| [3] |
Mohler JL, Anarakis ES, Armstrong AJ, et al. Prostate cancer, version 2.2019, NCCN clinical practice guidelines in oncology [J]. J Natl Compr Canc Netw, 2019, 17(5):479-505.
doi: 10.6004/jnccn.2019.0023 |
| [4] |
Mungovan SF, Sandhu JS, Akin O, et al. Preoperative membranous urethral length measurement and continence recovery following radical prostatectomy: A systematic review and meta-analysis [J]. Euro Urol, 2017, 71(3):368-378.
doi: 10.1016/j.eururo.2016.06.023 |
| [5] |
Macura KJ, Genadry RR. Female urinary incontinence: Pathophysiology, methods of evaluation and role of MR imaging [J]. Abdom Imaging, 2008, 33(3):371-380.
doi: 10.1007/s00261-007-9257-6 |
| [6] |
Huang HC, Jiang YH, Lin VC, et al. Possible predictor of early recovery on urinary continence after laparoscopic radical prostatectomy: Bladder neck level and urodynamic parameters [J]. J Formos Med Assoc, 2019, 118(1 Pt 2):237-243.
doi: 10.1016/j.jfma.2018.04.009 |
| [7] |
Kageyama S, Yoshida T, Nagasawa M, et al. The location of the bladder neck in postoperative cystography predicts continence convalescence after radical prostatectomy [J]. BMC Urol, 2018, 18(1):52.
doi: 10.1186/s12894-018-0370-3 pmid: 29848326 |
| [8] |
Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy [J]. Eur Urol, 2012, 62(3):405-417.
doi: 10.1016/j.eururo.2012.05.045 |
| [9] |
Heesakkeers J, Farag F, Bauer RM, et al. Pathophysiology and contributing factors in postprostatectomy incontinence: A review [J]. Eur Urol, 2017, 71(6):936-944.
doi: 10.1016/j.eururo.2016.09.031 |
| [10] |
Pavlovich CP, Rocco B, Druskin SC, et al. Urinary continence recovery after radical prostatectomy: Anatomical/reconstructive and nerve-sparing techniques to improve outcomes [J]. BJU Int, 2017, 120(2):185-196.
doi: 10.1111/bju.2017.120.issue-2 |
| [11] |
Walz J, Epstin JI, Ganzer R, et al. A critical analysis of the current knowledge of surgical anatomy of the prostate related to optimisation of cancer control and preservation of continence and erection in candidates for radical prostatectomy: An update [J]. Eur Urol, 2016, 70(2):301-311.
doi: 10.1016/j.eururo.2016.01.026 |
| [12] |
Covas Moschovas M, Bhat S, Onol FF, et al. Modified apical dissection and lateral prostatic fascia preservation improves early postoperative functional recovery in robotic-assisted laparoscopic radical prostatectomy: Results from a propensity score-matched analysis [J]. Eur Urol, 2020, 78(6):875-884.
doi: 10.1016/j.eururo.2020.05.041 |
| [13] |
Lee YJ, Jung JW, Lee S, et al. Contemporary trends in radical prostatectomy and predictors of recovery of urinary continence in men aged over 70 years: Comparisons between cohorts aged over 70 and less than 70 years [J]. Asian J Androl, 2020, 22(3):280-286.
doi: 10.4103/aja.aja_62_19 |
| [14] | 张帆, 肖春雷, 张树栋, 等. 前列腺体积及前列腺突入膀胱长度与腹腔镜前列腺癌根治术后控尿功能恢复的相关性 [J]. 北京大学学报(医学版), 2018, 50(4):621-625. |
| [15] |
Grivas N, van Der RR, Schouten D, et al. Quantitative assessment of fascia preservation improves the prediction of membranous urethral length and inner levator distance on continence outcome after robot‐assisted radical prostatectomy [J]. Neurourol Urodyn, 2017, 37(1):417-425.
doi: 10.1002/nau.v37.1 |
| [16] |
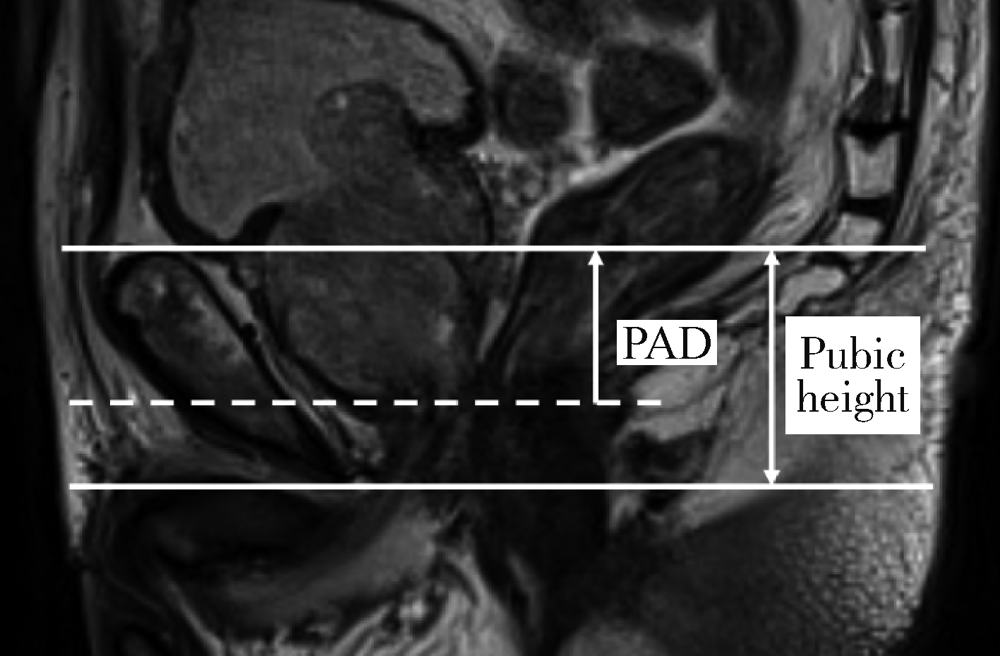
Yang B, Zhang F, Xiao C, et al. Impact of preoperative magnetic resonance imaging anatomic features on urinary continence recovery after laparoscopic radical prostatectomy [J]. Urol Int, 2020, 104(3/4):239-246.
doi: 10.1159/000506021 |
| [17] |
Matsushita K, Kent MT, Vickers AJ, et al. Preoperative predictive model of recovery of urinary continence after radical prostatectomy [J]. BJU Int, 2015, 116(4):577-583.
doi: 10.1111/bju.13087 pmid: 25682782 |
| [18] |
Kadono Y, Nohara T, Kawaguchi S, et al. Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: Effectiveness of a longer urethral stump to prevent urinary incontinence [J]. BJU Int, 2018, 122(3):456-462.
doi: 10.1111/bju.14181 |
| [19] | Fukui S, Kagebayashi Y, Iemura Y, et al. Preoperative MRI parameters predict urinary continence after robot-assisted laparoscopic prostatectomy in prostatic cancer patients [J]. Diagnostics (Basel), 2019, 9(3):102. |
| [1] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [2] | Shuhui YU,Jianing HAN,Lijun ZHONG,Congyu CHEN,Yunxiang XIAO,Yanbo HUANG,Yang YANG,Xinyan CHE. Predictive value of preoperative pelvic floor electrophysiological parameters on early urinary incontinence following radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 594-599. |
| [3] | Yuqing LI,Biao WANG,Peng QIAO,Wei WANG,Xing GUAN. Medium to long-term efficacy of tension-free vaginal tape procedure in the treatment of female recurrent stress urinary incontinence [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 600-604. |
| [4] | Hai MAO,Fan ZHANG,Zhan-yi ZHANG,Ye YAN,Yi-chang HAO,Yi HUANG,Lu-lin MA,Hong-ling CHU,Shu-dong ZHANG. Predictive model of early urinary continence recovery based on prostate gland MRI parameters after laparoscopic radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 818-824. |
| [5] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [6] | Zhan-yi ZHANG,Fan ZHANG,Ye YAN,Cai-guang CAO,Chang-jian LI,Shao-hui DENG,Yue-hao SUN,Tian-liang HUANG,Yun-he GUAN,Nan LI,Min LU,Zhen-hua HU,Shu-dong ZHANG. Near-infrared targeted probe designed for intraoperative imaging of prostatic neurovascular bundles [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 843-850. |
| [7] | Hui-li LIU,Yan-han LV,Xiao-xiao WANG,Min LI. Factors influencing the chronic post-surgical pain after laparoscopic surgery for elderly patients with urinary tract tumors [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 851-856. |
| [8] | Ling-fu ZHANG,Chun-sheng HOU,Zhi XU,Li-xin WANG,Xiao-feng LING,Gang WANG,Long CUI,Dian-rong XIU. Clinical effect of laparoscopic transcystic drainage combined with common bile duct exploration for the patients with difficult biliary stones [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1185-1189. |
| [9] | Li-zhe AN,Liu-lin XIONG,Liang CHEN,Huan-rui WANG,Wei-nan CHEN,Xiao-bo HUANG. Laparoscopic pyeloplasty combined with ultrasonic lithotripsy via nephroscope for treatment of ureteropelvic junction obstruction with renal calculi [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 746-750. |
| [10] | ZHANG Fan,CHEN Qu,HAO Yi-chang,YAN Ye,LIU Cheng,HUANG Yi,MA Lu-lin. Relationship between recovery of urinary continence after laparoscopic radical prostatectomy and preoperative/postoperative membranous urethral length [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 299-303. |
| [11] | HAO Han,LIU Yue,CHEN Yu-ke,SI Long-mei,ZHANG Meng,FAN Yu,ZHANG Zhong-yuan,TANG Qi,ZHANG Lei,WU Shi-liang,SONG Yi,LIN Jian,ZHAO Zheng,SHEN Cheng,YU Wei,HAN Wen-ke. Evaluating continence recovery time after robot-assisted radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 697-703. |
| [12] | Bing-wei HUANG,Jie WANG,Peng ZHANG,Zhe LI,Si-cheng BI,Qiang WANG,Cai-bo YUE,Kun-lin YANG,Xue-song LI,Li-qun ZHOU. Application of indocyanine green in complex upper urinary tract repair surgery [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 651-656. |
| [13] | Shu-dong ZHANG,Peng HONG,Bin-shuai WANG,Shao-hui DENG,Fan ZHANG,Li-yuan TAO,Cai-guang CAO,Zhen-hua HU,Lu-lin MA. Usefulness of the indocyanine green fluorescence imaging technique in laparoscopic partial nephrectomy [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 657-662. |
| [14] | Si-da CHENG,Xin-fei LI,Sheng-wei XIONG,Shu-bo FAN,Jie WANG,Wei-jie ZHU,Zi-ao LI,Guang-pu DING,Ting YU,Wan-qiang LI,Yong-ming SUN,Kun-lin YANG,Lei ZHANG,Han HAO,Xue-song LI,Li-qun ZHOU. Robot-assisted laparoscopic upper urinary tract reconstruction surgery: A review of 108 cases by a single surgeon [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 771-779. |
| [15] | Hai-yue ZHAO,Xiong-jun YE,Wei-nan CHEN,Li-zhe AN,Jun LIU,Liu-lin XIONG,Xiao-bo HUANG. Treatment of crossing vessels in laparoscopic pyeloplasty [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 660-664. |
|
||