Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (5): 899-909. doi: 10.19723/j.issn.1671-167X.2023.05.019
Previous Articles Next Articles
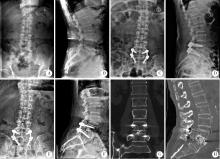
Efficacy analysis of autologous facet joint bone block in lumbar interbody fusion of osteoporosis patients
Da-wei WANG,Hua-dong WANG,Li LI,Xin YIN,Wei HUANG,Ji-dong GUO,Ya-feng YANG,Yi-hao LIU,Yang ZHENG*( )
)
- Department of Spine Surgery, the Fourth Medical Center, Chinese PLA General Hospital, Beijing 100048, China
CLC Number:
- R681.5
| 1 |
Wolfert AJ , Rompala A , Beyer GA , et al. The impact of osteoporosis on adverse outcomes after short fusion for degenerative lumbar disease[J]. Am Acad Orthop Surg, 2022, 30 (12): 573- 579.
doi: 10.5435/JAAOS-D-21-01258 |
| 2 |
Reid PC , Morr S , Kaiser MG . State of the union: A review of lumbar fusion indications and techniques for degenerative spine disease[J]. Neurosurg Spine, 2019, 31 (1): 1- 14.
doi: 10.3171/2019.4.SPINE18915 |
| 3 |
Zou D , Jiang S , Zhou S , et al. Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: A combination of DXA and Hounsfield units[J]. Spine (Phila Pa 1976), 2020, 45 (7): E406- E410.
doi: 10.1097/BRS.0000000000003284 |
| 4 | 孟海, 杨雍, 孙天胜, 等. 腰椎后路手术椎间融合器应用的专家共识[J]. 中国脊柱脊髓杂志, 2021, 31 (4): 379- 384. |
| 5 | 王东亮, 毛兆虎, 杨文玖, 等. 自体下关节突骨块在腰椎椎间融合中的应用解剖[J]. 中华实验外科杂志, 2013, 30 (12): 2726- 2727. |
| 6 |
Kai Y , Oyama M , Morooka M . Posterior lumbar interbody fusion using local facet joint autograft and pedicle screw fixation[J]. Spine (Phila Pa 1976), 2004, 29 (1): 41- 46.
doi: 10.1097/01.BRS.0000103940.57588.50 |
| 7 | 张绍东, 唐天驷, 杨惠林, 等. 保留部分关节突后路腰椎间融合治疗腰椎间盘退变性疾病[J]. 中国脊柱脊髓杂志, 2004, 14 (6): 360- 363. |
| 8 |
Siepe CJ , Stosch-Wiechert K , Heider F , et al. Anterior stand-alone fusion revisited: A prospective clinical, X-ray and CT investigation[J]. Eur Spine J, 2015, 24 (4): 838- 851.
doi: 10.1007/s00586-014-3642-y |
| 9 | 高志强, 李洋, 罗飞, 等. 对脊柱椎间融合的影像学评价策略[J]. 中国组织工程研究, 2015, 19 (48): 7825- 7830. |
| 10 |
Yao YC , Chou PH , Lin HH , et al. Risk factors of cage subsi-dence in patients received minimally invasive transforaminal lumbar interbody fusion[J]. Spine (Phila Pa 1976), 2020, 45 (19): E1279- E1285.
doi: 10.1097/BRS.0000000000003557 |
| 11 |
Park MK , Kim KT , Bang WS , et al. Risk factors for cage migration and cage retropulsion following transforaminal lumbar interbody fusion[J]. Spine J, 2019, 19 (3): 437- 447.
doi: 10.1016/j.spinee.2018.08.007 |
| 12 |
Strage KE , Parry JA , Mauffrey C . Standardizing statistics and data reporting in orthopaedic research[J]. Eur J Orthop Surg Traumatol, 2021, 31 (1): 1- 6.
doi: 10.1007/s00590-020-02843-8 |
| 13 | 杨喆, 谭志军, 张杨, 等. 医学研究中计量资料组间比较统计分析方法的正确应用[J]. 中国儿童保健杂志, 2019, 27 (10): 1157- 1160. |
| 14 |
Kuslich SD , Ulstrom CL , Griffith SL , et al. The Bagby and Kuslich method of lumbar interbody fusion: History, techniques, and 2-year follow-up results of a United States prospective, multicenter trial[J]. Spine (Phila Pa 1976), 1998, 23 (11): 1267- 1278.
doi: 10.1097/00007632-199806010-00019 |
| 15 | 唐强, 钟德君, 王清, 等. 椎间自体骨植骨面积比与椎间融合率的关系[J]. 中国组织工程研究, 2021, 25 (36): 5821- 5826. |
| 16 | Amorim-Barbosa T , Pereira C , Catelas D , et al. Risk factors for cage subsidence and clinical outcomes after transforaminal and posterior lumbar interbody fusion[J]. Eur J Orthop Surg Traumatol, 2022, 32 (7): 1291- 1299. |
| 17 |
Meng B , Bunch J , Burton D , et al. Lumbar interbody fusion: Recent advances in surgical techniques and bone healing strategies[J]. Eur Spine J, 2021, 30 (1): 22- 33.
doi: 10.1007/s00586-020-06596-0 |
| 18 | 白文媛, 顾洪生, 廖振华, 等. 正常成人腰椎间盘相关参数的测量和意义[J]. 中国临床解剖学杂志, 2013, 31 (5): 505- 510. |
| 19 | 中国健康促进基金会基层医疗机构骨质疏松症诊断与治疗专家共识委员会. 基层医疗机构骨质疏松症诊断和治疗专家共识(2021)[J]. 中国骨质疏松杂志, 2021, 27 (7): 937- 944. |
| 20 |
Wagner SC , Kang DG , Steelman T , et al. Diagnosing the undiagnosed: Osteoporosis in patients undergoing lumbar fusion[J]. Spine (Phila Pa 1976), 2016, 41 (21): E1279- E1283.
doi: 10.1097/BRS.0000000000001612 |
| 21 | Khalid SI , Nunna RS , Maasarani S , et al. Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion[J]. Neurosurg Focus, 2020, 49 (2): E6. |
| 22 | Yu Y , Robinson DL , Ackland DC , et al. Influence of the geometric and material properties of lumbar endplate on lumbar interbody fusion failure: A systematic review[J]. J Orthop Surg Res, 2022, 17 (1): 224. |
| 23 | 赵龙, 曾建成, 谢天航, 等. 腰椎椎间融合术后椎间融合器沉降的研究进展[J]. 中国修复重建外科杂志, 2021, 35 (8): 1063- 1067. |
| 24 | 郭新虎, 孟妍, 齐强, 等. 后路腰椎椎体间融合术后cage移位的危险因素分析及处理策略[J]. 中国脊柱脊髓杂志, 2022, 32 (1): 42- 49. |
| 25 | Govindarajan V , Diaz A , Perez-Roman RJ , et al. Osteoporosis treatment in patients undergoing spinal fusion: A systematic review and meta-analysis[J]. Neurosurg Focus, 2021, 50 (6): E9. |
| 26 | Tani S , Ishikawa K , Kudo Y , et al. The effect of denosumab on pedicle screw fixation: A prospective 2-year longitudinal study using finite element analysis[J]. J Orthop Surg Res, 2021, 16 (1): 219. |
| 27 | 金贺荣, 崔敬斌, 邵苍, 等. 椎间融合器材料: 临床应用的优势与关注热点[J]. 中国组织工程研究, 2022, 26 (22): 3592- 3597. |
| 28 | Formica M , Vallerga D , Zanirato A , et al. Fusion rate and influence of surgery-related factors in lumbar interbody arthrodesis for degenerative spine diseases: A meta-analysis and systematic review[J]. Musculoskelet Surg, 2020, 104 (1): 1- 15. |
| 29 | 万东东, 胡茂忠, 许东浩, 等. 髂骨取骨术后并发症的研究进展[J]. 中国矫形外科杂志, 2016, 24 (12): 1096- 1100. |
| 30 | 刘军, 万豫尧, 王慧敏, 等. 改良自体棘突腰椎椎体间植骨融合术的临床应用[J]. 广东医学, 2006, 27 (7): 994- 996. |
| 31 | Tavares WM , de Franca SA , Paiva WS , et al. A systematic review and meta-analysis of fusion rate enhancements and bone graft options for spine surgery[J]. Sci Rep, 2022, 12 (1): 7546. |
| 32 | Geurts J , Ramp D , Schären S , et al. Georg-Schmorl-Prize of the German Spine Society (DWG) 2016: Comparison of in vitro osteogenic potential of iliac crest and degenerative facet joint bone autografts for intervertebral fusion in lumbar spinal stenosis[J]. Eur Spine J, 2017, 26 (5): 1408- 1415. |
| 33 | 万标林, 梁伟国, 王斌, 等. 自体椎板关节突柱状植骨融合治疗腰椎退行性疾病的疗效分析[J]. 中国矫形外科杂志, 2012, 20 (11): 964- 967. |
| 34 | 王璐璐, 陈晓亮, 马进峰, 等. 自体下关节突骨块与Cage椎体间融合效果比较[J]. 青岛大学医学院学报, 2012, 48 (1): 30- 32. |
| [1] | Xinzhu BAI,Jinhui HE,Songsong LU,Chun LI,Yilin WANG,Jian XIONG. Vertebral fractures combined with prolonged activated partial prothrombin time: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 371-374. |
| [2] | Wei ZHU,Bin ZHU,Xiao-guang LIU. Influential factors related to functional status after full-endoscopic lumbar discectomy [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 537-542. |
| [3] | Jie ZHU,Jian-hong LI,Ting-ting YUAN,Lu He,Yu-hong LIANG. Relationship between periodontitis and osteoporosis in postmenopausal women [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1115-1118. |
| [4] | Peng WANG,Hua WU,Ying CHE,Dong-wei FAN,Jue LIU,Li-yuan TAO. Evaluation of screening accuracy on osteoporosis self-assessment tool for Asians and its cut-off value in healthy physical examination population [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1085-1090. |
| [5] | SHANG Lan-pu, TIAN Yun, LIU Xiao-guang. Clinical comparison of polymethylmethacrylate and bone cement in the treatment of osteoporotic vertebral compression fractures: a retrospective study [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 267-273. |
| [6] | ZHENG Yi-lin, SONG Wen-fang, WANG Dong-xin. Comparison between flexible laryngeal mask airway and reinforced tracheal tube used for lumbar vertebral surgery in prone position [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 262-266. |
| [7] | SUN Hao-lin, LI Chun-de△, LI Xu-wen, YI Xiao-dong, LIU Hong, LU Hai-lin, LI Hong, YU Zheng-rong, WANG Yu. Polymethylmethacrylate augmentation of bone cement injectable cannulated pedicle screws was used to treat degenerative lumbar scoliosis with osteoporosis [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 256-261. |
| [8] | SUN Hao-lin, LI Chun-de, YANG Ze-chuan, YI Xiao-dong, LIU Hong, LU Hai-lin, LI Hong, WANG Yu. Polymethylmethacrylate augmentation of bone cement-injectable cannulated pedicle screws for the treatment of degenerative lumbar diseases with osteoporosis [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1019-1025. |
| [9] | WANG He, HU Zhao-heng, CHEN Ling2, PAN Yu3. Influence of history of oral bisphosphonates on the incidence rate of fever after intravenous injection of zoledronic acid in patients with osteoporosis [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 680-682. |
| [10] | LI Bing-yan, GENG Zhi-yu, WANG Dong-xin. Effect of dexmedetomidine infusion on postoperative recovery for patients undergoing major spinal surgery during propofol anesthesia [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 529-533. |
| [11] | LI Ning, LIU Hao-nan, GONG Xiao-feng, ZHU Shi-wen, WU Xin-bao, HE Liang. Epidemiological analysis of hospitalized patients with femoral neck fracture in a first-class hospital of Beijing [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 292-296. |
| [12] | LI Hong, LI Chun-de, YI Xiao-dong, LIU Hong, LU Hai-lin, WANG Yu. Analysis of the clinical outcomes of the over 5-year follow-up study of degenerative lumbar scoliosis treated with posterior decompression and instrumented fusion [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 250-256. |
| [13] | SUN Hao-Lin, LI Chun-De, ZHU Jia-Lin, YI Xiao-Dong, LIU Hong, LU Hai-Lin, LI Hong, YU Zheng-Rong, WANG Yu. Clinical research of percutaneous vertebroplasty or percutaneous kyphoplasty for treating osteoporotic vertebral compression fractures induced by glucocorticosteroid [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 242-247. |
| [14] | HUANG Tian-Ji, KOU Yu-Hui, YIN Xiao-Feng, XIONG Jian, ZHANG Pei-Xun, ZHANG Dian-Ying, FU Zhong-Guo, XUE Feng, JIANG Bao-Guo. Clinical characteristics and risk factors of newly developed vertebral fractures after vertebral augmentation [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 237-241. |
| [15] | FANG Liming, ZHANG Yajun△, ZHANG Jun, HUANG Nan, ZUO Zhenhua, LI Bing, WANG Bo, LIN Huagang. Minimally invasive percutaneous pedicle screw fixation for the treatment of thoracolumbar fractures and posterior ligamentous complex injuries [J]. Journal of Peking University(Health Sciences), 2012, 44(6): 851-854. |
|
||