Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (1): 177-181. doi: 10.19723/j.issn.1671-167X.2019.01.030
Previous Articles Next Articles
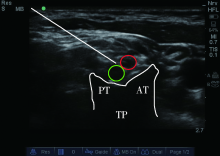
C5-6 nerve root block technique for postoperative analgesia of shoulder arthroscope: a randomized controlled trial
Ying DENG,Yan LI,Yao YAO,Dan-dan FENG,Mao XU( )
)
- Department of Anesthesiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R614.4
| [1] |
Hussain N, Goldar G, Raqina N . Suprascapular and interscalene nerve block for shoulder surgery: a systematic review and meta analysis[J]. Anesthesiology, 2017,127(6):998-1013.
doi: 10.1097/ALN.0000000000001894 |
| [2] |
Marhofer P, Harrop-Griffiths W, Willschke H , et al. Fifteen years of ultrasound guidance in regional anaesthesia: part 2. recent developments in block techniques[J]. Br J Anaesth, 2010,104(6):673-683.
doi: 10.1093/bja/aeq086 pmid: 20418267 |
| [3] |
Madison SJ, Humsi J, Loland VJ , et al. Ultrasound-guided root/trunk (interscalene) block for hand and forearm anesthesia[J]. Reg Anesth Pain Med, 2013,38(3):226-232.
doi: 10.1097/AAP.0b013e3182890d50 pmid: 23528646 |
| [4] |
Dhir S, Sondekoppam RV, Sharma R . A comparison of combined suprascapular and axillary nerve blocks to interscalene nerve block for analgesia in arthroscopic shoulder surgery: an equivalence stu-dy[J]. Reg Anesth Pain Med, 2016,41(5):564-571.
doi: 10.1097/AAP.0000000000000436 pmid: 27380105 |
| [5] |
Riazi S, Carmichael N, Awad L , et al. Effect of local anaesthetic volume (20 vs. 5 mL) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block[J]. Br J Anaesth, 2008,101(4):549-556.
doi: 10.1093/bja/aen229 pmid: 18682410 |
| [6] |
Lang RS, Kentor ML, Vallejo M , et al. The impact of local anesthetic distribution on block onset in ultrasound-guided interscalene block[J]. Acta Anaesthesiol Scand, 2012,56(9):1146-1151.
doi: 10.1111/j.1399-6576.2012.02745.x pmid: 22845687 |
| [7] |
Sinha SK, Abrams JH, Barnett JT , et al. Decreasing the local anesthetic volume from 20 to 10 mL for ultrasound-guided interscalene block at the cricoid level does not reduce the incidence of hemidiaphragmatic paresis[J]. Reg Anesth Pain Med, 2011,36(1):17-20.
doi: 10.1097/AAP.0b013e3182030648 pmid: 21751435 |
| [8] |
Vandepitte C, Gautier P, Xu D , et al. Effective volume of ropi-vicaine 0.75% through a catheter required for interscalene brachial plexus blockade[J]. Anesthesiology, 2013,118(4):863-867.
doi: 10.1097/ALN.0b013e3182850dc7 |
| [9] | Winnie AP . Interscalene brachial plexus block[J]. Anesth Analg, 1970,49:455-466. |
| [10] |
Mendelsohn AH, Deconde A, Lambert HW , et al. Cervical variations of the phrenic nerve[J]. Laryngoscope, 2011,121(9):1920-1923.
doi: 10.1002/lary.21894 pmid: 22024845 |
| [11] |
Lee J, Kim K, Kim S . Threatment of a symptomatic cervical perineural cyst with ultrasound-guided cervical selective nerve root block: a case report[J]. Medicine (Baltimore), 2018,97(37):e12412.
doi: 10.1097/MD.0000000000012412 |
| [12] |
van Geffen GJ, Moayeri N, Bruhn J , et al. Correlation between ultrasound imaging, cross-sectional anatomy, and histology of the brachial plexus: a review[J]. Reg Anesth Pain Med, 2009,34(5):490-497.
doi: 10.1097/AAP.0b013e3181add8a3 pmid: 19920425 |
| [13] |
Kapral S, Greher M, Huber G , et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade[J]. Reg Anesth Pain Med, 2008,33(3):253-258.
doi: 10.1016/j.rapm.2007.10.011 pmid: 18433677 |
| [14] |
Shin HJ, Na HS, Oh AY ,et a1. A prospective,randomized and controlled study of interscalene brachiaI plexus block for arthroscopic shoulder surgery: a comparison of C5 and con-ventional approach, a CONSORT-compliant article[J]. Medicine (Baltimore), 2016,95(37):e4921.
doi: 10.1097/MD.0000000000004921 |
| [15] |
Marhofer P, Greher M, Kapral S . Ultrasound guidance in regional anaesthesia[J]. Br J Anaesth, 2005,94(1):7-17.
doi: 10.1093/bja/aer111 pmid: 15277302 |
| [16] | 周玉弟, 姜慧丽, 汤洋 , 等. 超声引导下选择性颈神经根阻滞在肩关节镜术后镇痛中的应用[J]. 临床麻醉学杂志, 2017,12(33):1167-1170. |
| [17] |
Junq HS, Seo KH, Kanq JH . Optimal dose of perineural dexmedetomidine for inerscalene brachial plexus block to control post-operative pain in patients undergoing arthroscopic shoulder sur-gery: a prospective, double-blind,randomized controlled study[J]. Medicine (Baltimore), 2018,97(16):e0440.
doi: 10.1097/MD.0000000000010440 |
| [18] |
Marhofer D, Marhofer P, Triffterer L , et al. Dislocation rates of perineural catheters: a volunteer study[J]. Br J Anaesth, 2013,111(5):800-806.
doi: 10.1093/bja/aet198 pmid: 23748198 |
| [19] |
张大志, 刘永盛, 周海滨 . 舒芬太尼与地塞米松对罗哌卡因神经阻滞作用影响的比较研究[J]. 中国药物警戒, 2012,9(12):710-712.
doi: 10.3969/j.issn.1672-8629.2012.12.003 |
| [1] | Jiangjing WANG,Shunyi WEI,Yingfang AO,Yuping YANG. Comparison of the early analgesic efficacy of three different drugs after anterior cruciate ligament reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 293-298. |
| [2] | Fei WANG,Yang-yang ZHAO,Ming GUAN,Jing WANG,Xiang-liang XU,Yu LIU,Xin-li ZHAI. Application of intravenous sedation in 2 582 cases of oral and maxillofacial surgery [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 181-186. |
| [3] | LI Yan, WANG Hui, DENG Ying, YAO Yao, LI Min. Effect of dexmedetomidine on supraclavicular brachial plexus block: a randomized double blind prospective study [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 845-849. |
| [4] | MENG Tian, ZHANG Zhi-yong, ZHANG Xiao, CHEN Yu-huan, LI Jing-qi, CHENG Quan, LIU Wen-shu, GAO Wei. Preemptive analgesia with loxoprofen sodiumorally in extraction of impacted teeth [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 165-169. |
| [5] | ZHAO Min-wei, WANG Ning, ZENG Lin, LI Min, ZHAO Zhong-kai, ZHANG Han, TIAN Hua . Comparision for clinical efficiency of continuous adductor canal block and femoral nerve block in total knee arthroplasty [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 142-147. |
| [6] | LI Bing-yan, GENG Zhi-yu, WANG Dong-xin. Effect of dexmedetomidine infusion on postoperative recovery for patients undergoing major spinal surgery during propofol anesthesia [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 529-533. |
| [7] | YI Jun, XU Li, LIN Hui-hua . Postoperative analgesia effect of different background volumes of ropivacaine in continuous tibial nerve block in patients with calcaneal surgery [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 283-286. |
| [8] | CHI Li-Qun, LU Xin, WANG Lei, LIU Shu-Ping, DING Nan, ZHANG Hong-Ying, E Wen. Detection of cytochrome P450 3A4 gene polymorphism guides for labor analgesia with sufentanil medication [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 653-656. |
| [9] | LIU Hui-li, MA Cai-hong, ZHANG Xiao-qing, YANG Yan, SONG Xue-ling, GUO Xiang-yang. Combined efficacy of parecoxib and incisional ropivacaine infiltration on pain management after diagnostic hysteroscopy and laparoscopy [J]. Journal of Peking University(Health Sciences), 2013, 45(6): 901-905. |
|
||