Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (3): 530-535. doi: 10.19723/j.issn.1671-167X.2019.03.023
Previous Articles Next Articles
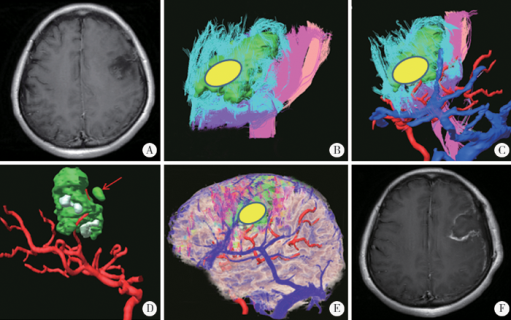
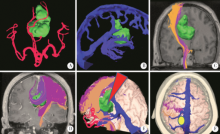
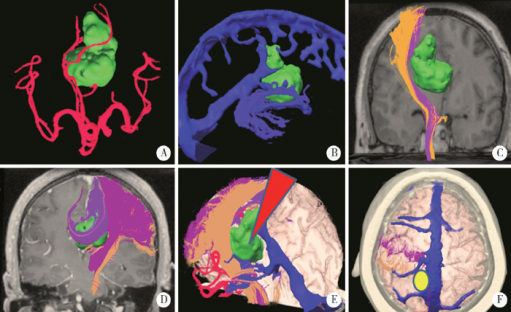
Application of diffusion tensor imaging combined with virtual reality three-dimensional reconstruction in the operation of gliomas involved eloquent regions
Su-hua CHEN1,Jun YANG1△( ),Hong-bin HAN2,3,De-hua CUI2,Jian-jun SUN1,Chang-cheng MA1,Qing-yuan HE2,3,Guo-zhong LIN1,Yun-feng HAN1,Chao WU1,Kai-ming MA1,Yi-bo ZHANG1
),Hong-bin HAN2,3,De-hua CUI2,Jian-jun SUN1,Chang-cheng MA1,Qing-yuan HE2,3,Guo-zhong LIN1,Yun-feng HAN1,Chao WU1,Kai-ming MA1,Yi-bo ZHANG1
- 1. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
2. Beijing Key Lab of Magnetic Resonance Imaging Device and Technique, Beijing 100191, China
3. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R651.1
| [1] |
Lacroix M, Abisaid D, Fourney DR , et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival[J]. J Neurosurg, 2001,95(2):190-198.
doi: 10.3171/jns.2001.95.2.0190 |
| [2] |
Sawaya R, Hammoud M, Schoppa D , et al. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors[J]. Neurosurgery, 1998,42(5):1044-1055.
doi: 10.1097/00006123-199805000-00054 |
| [3] |
Schucht P, Beck J, Abu-Isa J , et al. Gross total resection rates in contemporary glioblastoma surgery: results of an institutional protocol combining 5-aminolevulinic acid intraoperative fluorescence imaging and brain mapping[J]. Neurosurgery, 2012,71(5):927-935.
doi: 10.1227/NEU.0b013e31826d1e6b |
| [4] |
Della Puppa A, de Pelleqrin S, d’Avella E , et al. 5-aminolevulinic acid (5-ALA) fluorescence guided surgery of high-grade gliomas in eloquent areas assisted by functional mapping. Our experience and review of the literature[J]. Acta Neurochir(Wien), 2013,155(6):965-972.
doi: 10.1007/s00701-013-1660-x |
| [5] | Wölfer J, Stummer W . Brain tumor imaging[M]. Berlin: Sprin-ger, 2014: 143-154. |
| [6] |
de Witt Hamer PC, Robles SG, Zwinderman AH , et al. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta analysis[J]. J Clin Oncol, 2012,30(20):2559-2565.
doi: 10.1200/JCO.2011.38.4818 |
| [7] |
McGirt MJ, Mukherjee D, Chaichana KL , et al. Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme[J]. Neurosurgery, 2009,65(3):463-470.
doi: 10.1227/01.NEU.0000349763.42238.E9 |
| [8] | 陈晓雷, 许百男, 王飞 , 等. 功能神经导航及术中磁共振成像在语言区胶质瘤手术中的应用[J]. 中华外科杂志, 2011(8):688-692. |
| [9] |
Senft C, Bink A, Franz K , et al. Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial.[J]. Lancet Oncol, 2011,12(11):997-1003.
doi: 10.1016/S1470-2045(11)70196-6 |
| [10] |
Guyotat J, Pallud J, Armoiry X , et al. 5-aminolevulinic acid-protoporphyrin Ⅸ fluorescence-guided surgery of high-grade gliomas: a systematic review[J]. Adv Tech Stand Neurosurg, 2016,43(43):61-83.
doi: 10.1007/978-3-319-21359-0 |
| [11] |
Signorelli F . The value of cortical stimulation applied to the sur-gery of malignant gliomas in language areas[J]. Neurol Sci, 2001,22(3):217-218.
doi: 10.1007/s100720100016 |
| [12] |
Pereira LC, Oliveira KM , L’Abbate GL, et al. Outcome of fully awake craniotomy for lesions near the eloquent cortex: analysis of a prospective surgical series of 79 supratentorial primary brain tumors with long follow-up[J]. Acta Neurochir (Wien), 2009,151(10):1215-1230.
doi: 10.1007/s00701-009-0363-9 |
| [13] | 漆松涛, 李志勇, 方陆雄 , 等. 功能区胶质瘤手术的基本策略与方法[J]. 中华神经外科杂志, 2013,29(11):1083-1086. |
| [14] |
Kockro RA, Serra L, Tseng-Tsai Y , et al. Planning and simulation of neurosurgery in a virtual reality environment[J]. Neurosurgery, 2000,46(1):118-137.
doi: 10.1093/neurosurgery/46.1.118 |
| [15] |
Stadie AT, Kockro RA, Reisch R , et al. Virtual reality system for planning minimally invasive neurosurgery[J]. J Neurosurg, 2008,108(2):382-394.
doi: 10.3171/JNS/2008/108/2/0382 |
| [16] | 陈素华, 杨军, 马顺昌 , 等. 虚拟现实技术在颅颈交界区病变手术中的应用[J]. 中华神经外科杂志, 2018,34(6):591-595. |
| [17] |
Shi J, Xia J, Wei Y , et al. Three-dimensional virtual reality simulation of periarticular tumors using Dextroscope reconstruction and simulated surgery: a preliminary 10-case study[J]. Med Sci Monit, 2014,20:1043-1050.
doi: 10.12659/MSM.889770 |
| [18] |
Ng I, Hwang PY, Kumar D , et al. Surgical planning for micro-surgical excision of cerebral arterio-venous malformations using virtual reality technology[J]. Acta Neurochir (Wien), 2009,151(5):453-463.
doi: 10.1007/s00701-009-0278-5 |
| [19] |
Hattingen E, Rathert J, Jurcoane A , et al. A standardised evaluation of pre-surgical imaging of the corticospinal tract: where to place the seed ROI[J]. Neurosurg Rev, 2009,32(4):445-456.
doi: 10.1007/s10143-009-0197-1 |
| [20] |
Kim Y, Kim H, Kim YO . Virtual reality and augmented reality in plastic surgery: a review[J]. Arch Plast Surg, 2017,44(3):179-187.
doi: 10.5999/aps.2017.44.3.179 |
| [21] |
Guan XP, Wang W, Wang AB , et al. Brain interstitial fluid drainage alterations in glioma-bearing rats[J]. Aging Dis, 2018,9(2):228-234.
doi: 10.14336/AD.2017.0415 |
| [1] | ZHAO Si-ming,ZHAO Xiao-han,ZHANG Jie,WANG Dang-xiao,WANG Xiao-yan. Preliminary evaluation of a virtual reality dental simulation system on training of caries identification ability [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 139-142. |
| [2] | Hong HONG,Yu-ting QIAN,Lei FU,Wu WANG,Cheng-hui LI,Yi-qing YIN. Study on the use of CT three-dimensional reconstruction technique for guiding tracheal intubation with rigid fiber bronchoscope in difficult airway [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 870-874. |
| [3] | YU Yao, ZHANG Wen-bo, WANG Yang, LIU Xiao-jing, GUO Chuan-bin, YU Guang-yan, PENG Xin. Application of three-dimensional reconstruction of the enhanced CT with iPlan CMF software in head and neck neoplasms [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 878-882. |
| [4] | ZHAO Yi-jiao, WANG Si-wei, LIU Yi, WANG Yong. A method for rapid extracting three-dimensional root model of vivo tooth from cone beam computed tomography data based on the anatomical characteristics of periodontal ligament [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 54-059. |
|
||