Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (5): 875-880. doi: 10.19723/j.issn.1671-167X.2019.05.014
Previous Articles Next Articles
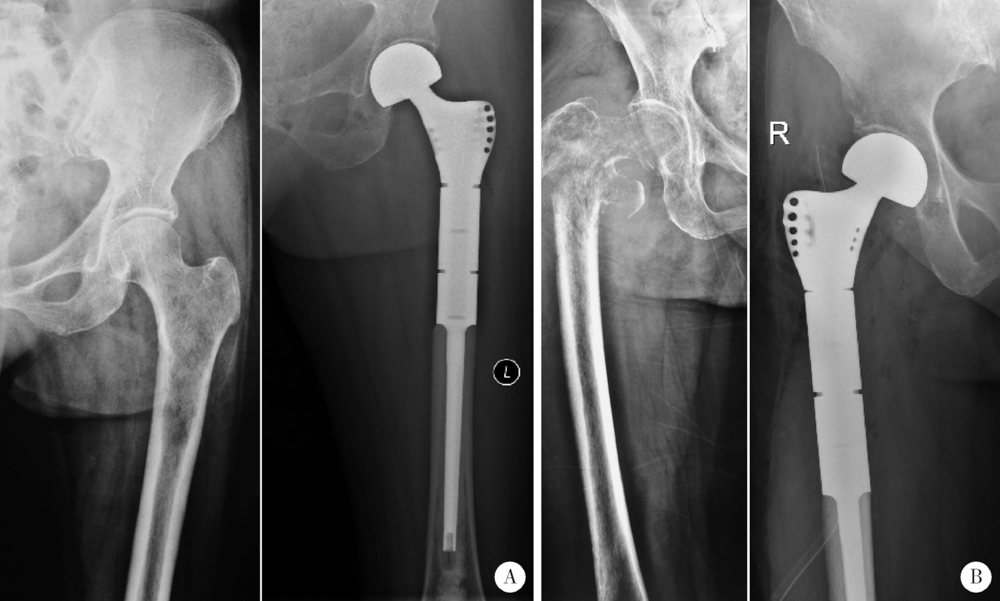
Perioperative clinical characteristics of patients with pathological fracture of proximal femur
Yun-peng CUI,Chuan MI,Bing WANG,Yuan-xing PAN,Yun-fei LIN,Xue-dong SHI( )
)
- Department of Orthopaedics, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R683.42
| [1] | Sumathi VP, Jeys L, Legdeur N . Metastatic tumours of bone[J]. Surgery (Oxford), 2012,30(2):80-85. |
| [2] | Costa L, Badia X, Chow E , et al. Impact of skeletal complications on patients’ quality of life, mobility, and functional independence[J]. Support Care Cancer, 2008,16(10):879-889. |
| [3] | Harvey N, Ahlmann ER, Allison DC , et al. Endoprostheses last longer than intramedullary devices in proximal femur metastases[J]. Clin Orthop Relat Res, 2012,470(3):684-691. |
| [4] | 杨毅, 郭卫, 尉然 . 两种方式重建股骨近端转移癌患者的围手术期安全性比较[J]. 中国骨与关节外科, 2013,6(3):214-218. |
| [5] | Steensma M, Boland PJ, Morris CD , et al. Endoprosthetic treatment is more durable for pathologic proximal femur fractures[J]. Clin Orthop Relat Res, 2012,470(3):920-926. |
| [6] | Wedin R, Bauer HC . Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosjournal or reconstruction nail?[J]. J Bone Joint Surg, 2005,87(12):1653-1657. |
| [7] | Ratasvuori M, Wedin R, Hansen BH , et al. Prognostic role of en-bloc resection and late onset of bone metastasis in patients with bone-seeking carcinomas of the kidney, breast, lung, and prostate: SSG study on 672 operated skeletal metastases[J]. J Surg Oncol, 2014,110(4):360-365. |
| [8] | Hobusch GM, Bollmann J, Puchner SE , et al. What sport activity levels are achieved in patients after resection and endoprosthetic reconstruction for a proximal femur bone sarcoma?[J]. Clin Orthop Relat Res, 2016,475(3):1-10. |
| [9] | Guzik G . Treatment outcomes and quality of life after the implantation of modular prostheses of the proximal femur in patients with cancer metastases[J]. Ortop Traumatol Rehabil, 2016,18(3):231-238. |
| [10] | Peterson JR, O’Connor IT, Topfer J, et al. Functional results and complications with long stem hemiarthroplasty in patients with metastases to the proximal femur[J]. J Am Coll Surgeons, 2016,223(4):e150. |
| [11] | Calabró T, Rooyen RV, Piraino I , et al. Reconstruction of the proximal femur with a modular resection prosjournal[J]. Eur J Orthop Surg Traumatol, 2016,26(4):415-421. |
| [12] | Peterson JR, Decilveo AP, O’Connor IT, et al. What are the functional results and complications with long stem hemiarthroplasty in patients with metastases to the proximal femur?[J]. Clin Ortho Relat Res, 2017,475(3):745-756. |
| [13] | Houdek MT, Watts CD, Wyles CC , et al. Functional and oncologic outcome of cemented endoprosjournal for malignant proximal femoral tumors[J]. J Surg Oncol, 2016,114(4):501-506. |
| [14] | Thambapillary S, Dimitriou R, Makridis KG , et al. Implant longevity, complications and functional outcome following proximal femoral arthroplasty for musculoskeletal tumors: a systematic review[J]. J Arthroplasty, 2013,28(8):1381-1385. |
| [15] | Janssen SJ, Teunis T, Hornicek FJ , et al. Outcome after fixation of metastatic proximal femoral fractures: A systematic review of 40 studies[J]. J Surg Oncol, 2016,114(4):507-519. |
| [16] | Houdek MT, Wyles CC, Labott JR , et al. Durability of hemiarthroplasty for pathologic proximal femur fractures[J]. J Arthroplasty, 2017,32(12):3607-3610. |
| [17] | Zoccali C, Attala D, Uccio ASD , et al. The dual mobility cup in muscular skeletal oncology: rationale and indications[J]. Int Orthop, 2017,41(3):447-453. |
| [18] | Gross JB . Estimating allowable blood loss: corrected for dilution[J]. Anesthesiology, 1983,58(3):277-280. |
| [19] | Liu X, Zhang X, Chen Y , et al. Hidden blood loss after total hip arthroplasty[J]. J Arthroplasty, 2011,26(7):1100-1105. |
| [20] | Kumar A, Torres ML, Cliby WA , et al. Inflammatory and nutritional serum markers as predictors of peri-operative morbidity and survival in ovarian cancer[J]. Anticancer Res, 2017,37(7):3673-3677. |
| [21] | Goh SL, De Silva RP, Dhital K , et al. Is low serum albumin associated with postoperative complications in patients undergoing oesophagectomy for oesophageal malignancies?[J]. Interact Cardiovasc Thorac Surg, 2015,20(1):107-113. |
| [22] | Musallam KM, Tamim HM, Richards T , et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study[J]. Lancet, 2011,378(9800):1396-1407. |
| [23] | Fowler AJ, Ahmad T, Phull MK , et al. Meta-analysis of the association between preoperative anaemia and mortality after surgery[J]. Br J Surg, 2015,102(11):1314-1324. |
| [24] | Rasouli MR, Restrepo C, Maltenfort MG , et al. Risk factors for surgical site infection following total joint arthroplasty[J]. J Bone Joint Surg Am, 2014,96(18):e158. |
| [25] | 周宗科, 翁习生, 向兵 , 等. 中国髋、膝关节置换术加速康复——围术期贫血诊治专家共识[J]. 中华骨与关节外科杂志, 2016,9(1):10-15. |
| [26] | Mirels H . Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures[J]. Clin Orthop Relat Res, 1989,249:256-264. |
| [27] | Damron TA, Morgan H, Prakash D , et al. Critical evaluation of Mirels’ rating system for impending pathologic fractures[J]. Clin Orthop Relat Res, 2003(415 Suppl):S201-S207. |
| [28] | Damron TA, Nazarian A, Entezari V , et al. CT-based structural rigidity analysis is more accurate than Mirels scoring for fracture prediction in metastatic femoral lesions[J]. Clin Orthop Relat Res, 2016,474(3):643-651. |
| [29] | Ulaner GA, Zindman AM, Zheng J , et al. FDG PET/CT assesses the risk of femoral pathological fractures in patients with metastatic breast cancer[J]. Clin Nucl Med, 2017,42(4):264-270. |
| [1] | Xinzhu BAI,Jinhui HE,Songsong LU,Chun LI,Yilin WANG,Jian XIONG. Vertebral fractures combined with prolonged activated partial prothrombin time: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 371-374. |
| [2] | Jin-hua ZHANG,Jie PAN,Zhi-peng SUN,Xiao WANG. Effect of various intracanal materials on the diagnostic accuracy of cone-beam computed tomography in vertical root fractures [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 333-338. |
| [3] | Zhong-di LIU,Ting-min XU,Yu DANG,Dian-ying ZHANG,Zhong-guo FU. Clinical effectiveness of less invasive intramedullary nail fixation combined with titanium cable cerclage for subtrochanteric fractures [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1102-1106. |
| [4] | Fu-zheng GUO,Feng-xue ZHU,Jiu-xu DENG,Zhe DU,Xiu-juan ZHAO. Risk factors for mechanical ventilation in patients with severe multiple trauma [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 738-742. |
| [5] | Li-yuan QI,Chen CHEN,Lan JIANG,Jia-nan LI,Yu-hong LIANG. Construction of swept source optical coherence tomography imaging system for root canal endoscopy and application in diagnosis of root fractures [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 753-757. |
| [6] | Yi-ran ZHANG,Feng RAO,Wei PI,Pei-xun ZHANG,Bao-guo JIANG. Proximal femoral nails antirotation and dynamic hip screws for fixation of unstable intertrochanteric fractures of femur: A meta-analysis [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 493-500. |
| [7] | Wei ZHANG,Pei-xun ZHANG. Analysis of prophylactic effect of extended-duration anticoagulant drugs in elderly patients undergoing hip fracture [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 501-504. |
| [8] | Bing-chuan LIU,Zhong-wei YANG,Fang ZHOU,Hong-quan JI,Zhi-shan ZHANG,Yan GUO,Yun TIAN. Application of the modified internal fixation method of minimally invasive percuta-neous plate osteosynthesis in treatment of proximal humeral fracture [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 277-282. |
| [9] | Jian CHEN,Cai-hong ZUO,Cai-yi ZHANG,Ming YANG,Pei-xun ZHANG. Comparison of the effects of two cephalomedullary nails (zimmer natural nail and proximal femoral nail antirotation) in treatment of elderly intertrochan teric fractures [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 283-287. |
| [10] | Xin yi LI,Jin xia ZHAO,Xiang yuan LIU. Diagnosis and treatment of antiphospholipid antibody:related recurrent spontaneous abortion and analysis of therapeutic drugs and pregnancy outcome in 75 patients with antiphospholipid syndrome [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 956-961. |
| [11] | HUANG Zi-xiong, ZHANG Xiao-peng, DONG Sen, LIU Shi-jun, YANG Rong-li, ZHOU Yu-shi, MA Wei-guo. Renal mucinous tubular and spindle cell carcinoma combined with multiple bone metastasis: a case report and literature review [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 732-735. |
| [12] | WEI Bin, ZHANG Hua, XU Mao, LI Min, WANG Jun, ZHANG Li-ping, GUO Xiang-yang, ZHAO Yi-ming, ZHOU Fang. Effect of different anesthetic methods on postoperative outcomes in elderly patients undergoing hip fracture surgery [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1008-1013. |
| [13] | LI Xu, LI Feng-long, LU Yi, ZHU Yi-ming, GUO Si-yi, LI Yi-jun, JIANG Chun-yan. Clinical study on locking plate for the treatment of non-osteoporotic complex proximal humeral fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 855-860. |
| [14] | ZHANG Shu, ZHANG Ji-yuan, YANG Du-ming, YANG Ming, ZHANG Pei-xun. Morphology character and reduction methods of sagittally unstable intertrochanteric fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 236-241. |
| [15] | ZHANG Quan, SUN Ning, HUANG Qiang, ZHU Shi-wen. Minimally invasive plate osteosynthesis for treatment of proximal humeral fractures through anterolateral acromial approach [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 242-245. |
|
||