Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 582-585. doi: 10.19723/j.issn.1671-167X.2020.03.028
Previous Articles Next Articles
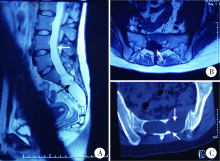
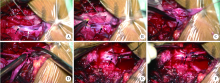
Clinical study of 21 cases of sacral cysts containing fila terminale
Guo-zhong LIN,Zhen-yu WANG( ),Jing-cheng XIE,Bin LIU,Chang-cheng MA,Xiao-dong CHEN
),Jing-cheng XIE,Bin LIU,Chang-cheng MA,Xiao-dong CHEN
- Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R651.2
| [1] | 陈晓东, 王振宇, 谢京城, 等. 症状性骶管内囊肿的诊断与治疗[J]. 中国脊柱脊髓杂志, 2006,16(2):138-141. |
| [2] | Sun J, Wang Z, Li Z, et al. Reconstruction of nerve root sheaths for sacralextradural spinal meningeal cysts with spinal nerve root fibers[J]. Sci China Life Sci, 2013,56(11):1007-1013. |
| [3] |
Nabors MW, Pait TG, Byrd EB, et al. Updated assessment and current classification of spinal meningeal cysts[J]. J Neurosurg, 1988,68(3):366-377.
pmid: 3343608 |
| [4] | 谢京城, 王振宇, 陈晓东. 骶管终丝脊膜囊肿合并脊髓拴系综合征的诊断和治疗[J]. 中国临床神经外科杂志, 2015,20(11):651-653. |
| [5] | Hukuda S, Mochizuki T, Ogata M, et al. Operations for cervical spondylotic myelopathy. A comparison of the results of anterior and posterior procedures[J]. J Bone Joint Surg Br, 1985,67(4):609-615. |
| [6] | Selcuki M, Mete M, Barutcuoglu M, et al. Tethered cord syndrome in adults: Experience of 56 patients[J]. Turk Neurosurg, 2015,25(6):922-929. |
| [7] | 汪寒松. MRI在诊断骶管囊肿中的应用[J]. 中国当代医药, 2014,21(2):127-128. |
| [8] | Lee GY, Paradiso G, Tator CH, et al. Surgical management of tethered cord syndrome in adults: indications, techniques, and long-term outcomes in 60 patients[J]. J Neurosurg Spine, 2006,4(2):123-131. |
| [9] | Sun JJ, Wang ZY, Liu B, et al. Neck transfixion for sacralextradural spinal meningeal cysts without spinal nerve root fibers[J]. Eur Spine J, 2016,25(6):1945-1952. |
| [10] | 林国中, 王振宇, 刘斌. 神经电生理监测技术在椎管内病变术中的应用[J]. 北京大学学报(医学版), 2012,44(5):776-779. |
| [1] | Mei-ge LIU,Pu FANG,Yan WANG,Lu CONG,Yang-yi FAN,Yuan YUAN,Yan XU,Jun ZHANG,Dao-jun HONG. Clinical, pathological and genetic characteristics of 8 patients with distal hereditary motor neuropathy [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 957-963. |
| [2] | LIN Guo-zhong, MA Chang-cheng, WANG Zhen-yu, XIE Jing-cheng, LIU Bin, CHEN Xiao-dong. Minimally invasive treatment of cervical1-2 epidural neurilemmoma [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 586-589. |
| [3] | Jing WANG,Jun-peng CHEN,Yang WANG,Xiang-liang XU,Chuan-bin GUO. Application of digital mandibular movement record and masticatory muscle electromyography in the evaluation of stomatognathic function in patients with mandibular tumor [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 571-578. |
| [4] | CHEN Li-hua, YANG Yi, WEI Qun, LI Yun-jun, LI Wen-de, GAO Jin-bao,YU Bin, ZHAO Hao, XU Ru-xiang. Microsurgical management of petroclival meningiomas combined trans-subtemporal and suboccipital retrosigmoid keyhole approach [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 738-742. |
| [5] | DUAN Hong-Zhou, LI Liang, ZHANG Yang, ZHANG Jia-Yong, BAO Sheng-De. Surgical treatment of paraclinoid aneurysms [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 679-684. |
| [6] | PENG Jing, LONG Hai, YUAN Yi-Ming, CUI Wan-Shou, ZHANG Zhi-Chao, PAN Wen-Bo. Comparison of the outcomes of microscopic varicocelectomy and laparoscopic varicocelectomy [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 541-543. |
|