Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (6): 1124-1129. doi: 10.19723/j.issn.1671-167X.2020.06.023
Previous Articles Next Articles
Application of mixed reality technique for the surgery of oral and maxillofacial tumors
Zu-nan TANG,Yuh SOH Hui,Lei-hao HU,Yao YU,Wen-bo ZHANG,Xin PENG( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.05
| [1] | 章文博, 于尧, 王洋, 等. 数字化外科技术在上颌骨缺损重建中的应[J]. 北京大学学报(医学版), 2017,49(1):1-5. |
| [2] |
Bouchard C, Magill JC, Nikonovskiy V, et al. Osteomark: a surgical navigation system for oral and maxillofacial surgery[J]. Int J Oral Maxillofac Surg, 2012,41(2):265-270.
doi: 10.1016/j.ijom.2011.10.017 pmid: 22103996 |
| [3] |
Haddock NT, Monaco C, Weimer KA, et al. Increasing bony contact and overlap with computer-designed offset cuts in free fibula mandible reconstruction[J]. J Craniofac Surg, 2012,23(6):1592-1595.
doi: 10.1097/SCS.0b013e318257576c pmid: 23147284 |
| [4] |
Pietruski P, Majak M, wiatek-Najwer E, et al. Navigation-guided fibula free flap for mandibular reconstruction: A proof of concept study[J]. J Plast Reconstr Aesthet Surg, 2019,72(4):572-580.
doi: 10.1016/j.bjps.2019.01.026 pmid: 30803870 |
| [5] |
Tepper OM, Rudy HL, Lefkowitz A, et al. Mixed reality with holoLens: where virtual reality meets augmented reality in the operating room[J]. Plast Reconstr Surg, 2017,140(5):1066-1070.
pmid: 29068946 |
| [6] |
Mitsuno D, Ueda K, Hirota Y, et al. Effective application of mixed reality device hololens: simple manual alignment of surgical field and holograms[J]. Plast Reconstr Surg, 2019,143(2):647-651.
doi: 10.1097/PRS.0000000000005215 pmid: 30688914 |
| [7] |
Incekara F, Smits M, Dirven C, et al. Clinical feasibility of a wearable mixed-reality device in neurosurgery[J]. World Neurosurg, 2018,118:e422-e427.
doi: 10.1016/j.wneu.2018.06.208 pmid: 30257298 |
| [8] |
Zhu H, Li Y, Wang C, et al. A first attempt of inferior vena cava filter successfully guided by a mixed-reality system: a case report[J]. J Geriatr Cardiol, 2019,16(7):575-577.
doi: 10.11909/j.issn.1671-5411.2019.07.008 pmid: 31447896 |
| [9] |
Saito Y, Sugimoto M, Imura S, et al. Intraoperative 3d hologram support with mixed reality techniques in liver surgery[J]. Ann Surg, 2020,271(1):e4-e7.
doi: 10.1097/SLA.0000000000003552 pmid: 31425293 |
| [10] | Rose AS, Kim H, Fuchs H, et al. Development of augmented-reality applications in otolaryngology-head and neck surgery[J]. Laryngoscope, 2019,129(S3):S1-S11. |
| [11] | 乔晨. 增强现实牙科虚拟手术的关键技术研究[D]. 北京理工大学, 2011. |
| [12] | 张益. 数字化外科技术及眼眶骨折精确重建[J]. 中华口腔医学杂志, 2012,47(8):463-465. |
| [13] | 于尧, 章文博, 王洋, 等. iPlan CMF软件辅助下增强CT三维重建在头颈部肿瘤治疗中的应用[J]. 北京大学学报(医学版), 2017,49(5):878-882. |
| [14] | 赵峰, 高勃, 刘震侠, 等. Dicom标准和Mimics软件辅助建立下颌骨三维有限元模型[J]. 西南国防医药, 2005,15(5):479-481. |
| [15] |
Sauer IM, Queisner M, Tang P, et al. Mixed reality in visceral surgery: development of a suitable workflow and evaluation of intraoperative use-cases[J]. Ann Surg, 2017,266(5):706-712.
doi: 10.1097/SLA.0000000000002448 pmid: 28767561 |
| [16] |
Léger É, Drouin S, Collins DL, et al. Quantifying attention shifts in augmented reality image-guided neurosurgery[J]. Healthc Technol Lett, 2017,4(5):188-192.
doi: 10.1049/htl.2017.0062 pmid: 29184663 |
| [17] |
Khor WS, Baker B, Amin K, et al. Augmented and virtual reality in surgery-the digital surgical environment: applications, limitations and legal pitfalls[J]. Ann Transl Med, 2016,4(23):454.
doi: 10.21037/atm.2016.12.23 pmid: 28090510 |
| [18] |
Gregory TM, Gregory J, Sledge J, et al. Surgery guided by mixed reality: presentation of a proof of concept[J]. Acta Orthop, 2018,89(5):480-483.
doi: 10.1080/17453674.2018.1506974 pmid: 30350756 |
| [19] |
McJunkin JL, Jiramongkolchai P, Chung W, et al. Development of a mixed reality platform for lateral skull base anatomy[J]. Otol Neurotol, 2018,39(10):e1137-e1142.
doi: 10.1097/MAO.0000000000001995 pmid: 30239435 |
| [20] | 叶哲伟, 吴星火. 混合现实技术在骨科的最新应用进展[J]. 临床外科杂志, 2018,26(1):13-14. |
| [21] |
Zhang WB, Mao C, Liu XJ, et al. Outcomes of orbital floor reconstruction after extensive maxillectomy using the computer-assisted fabricated individual titanium mesh technique[J]. J Oral Maxillofac Surg, 2015,73(10):2065.
pmid: 26188101 |
| [22] |
Sukegawa S, Kanno T, Furuki Y. Application of computer-assisted navigation systems in oral and maxillofacial surgery[J]. Jpn Dent Sci Rev, 2018,54(3):139-149.
pmid: 30128061 |
| [23] | 陈宝权, 秦学英. 混合现实中的虚实融合与人机智能交融[J]. 中国科学(信息科学), 2016,46(12):1737-1747. |
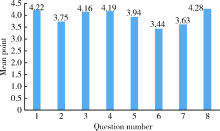
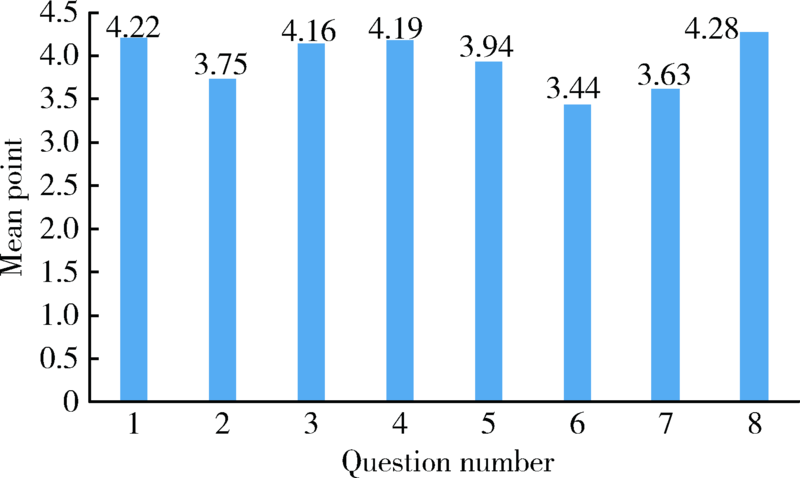
| [24] | Likert R. A technique for the measurement of attitudes[J]. Arch Psychol, 1932,22:5-55. |
| [1] | Fei WANG,Yang-yang ZHAO,Ming GUAN,Jing WANG,Xiang-liang XU,Yu LIU,Xin-li ZHAI. Application of intravenous sedation in 2 582 cases of oral and maxillofacial surgery [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 181-186. |
| [2] | Ming-zhe LI,Xiao-xia WANG,Zi-li LI,Biao YI,Cheng LIANG,Wei HE. Accuracy analysis of computer assisted navigation for condylectomy via intraoral approach [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 182-186. |
| [3] | Ling GAO,Yun LIU,Xu-dong YANG. Effects of intranasal dexmedetomidine for children undergoing dental rehabilitation under general anesthesia: a double-blinded randomized controlled trial [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1078-1082. |
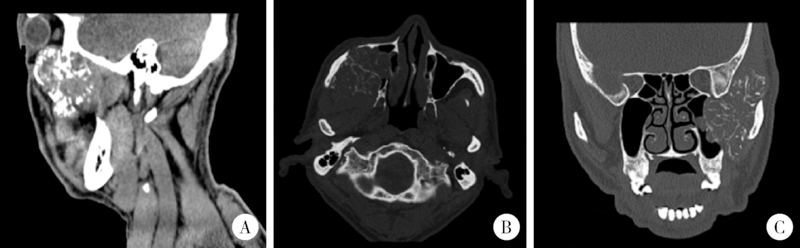
| [4] | YU Yao, ZHANG Wen-bo, WANG Yang, LIU Xiao-jing, GUO Chuan-bin, YU Guang-yan, PENG Xin. Application of three-dimensional reconstruction of the enhanced CT with iPlan CMF software in head and neck neoplasms [J]. Journal of Peking University(Health Sciences), 0, (): 878-882. |
| [5] | YU Yao, ZHANG Wen-bo, WANG Yang, LIU Xiao-jing, GUO Chuan-bin, YU Guang-yan, PENG Xin. Application of three-dimensional reconstruction of the enhanced CT with iPlan CMF software in head and neck neoplasms [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 878-882. |
| [6] | GE Na, GUAN Ming, LI Xi, LI Shuai, WANG En-bo. Application of flexible laryngeal mask airway in oral & maxillofacial day surgery [J]. Journal of Peking University(Health Sciences), 2015, 47(6): 1010-1014. |
|
||