Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 704-709. doi: 10.19723/j.issn.1671-167X.2021.04.014
Previous Articles Next Articles
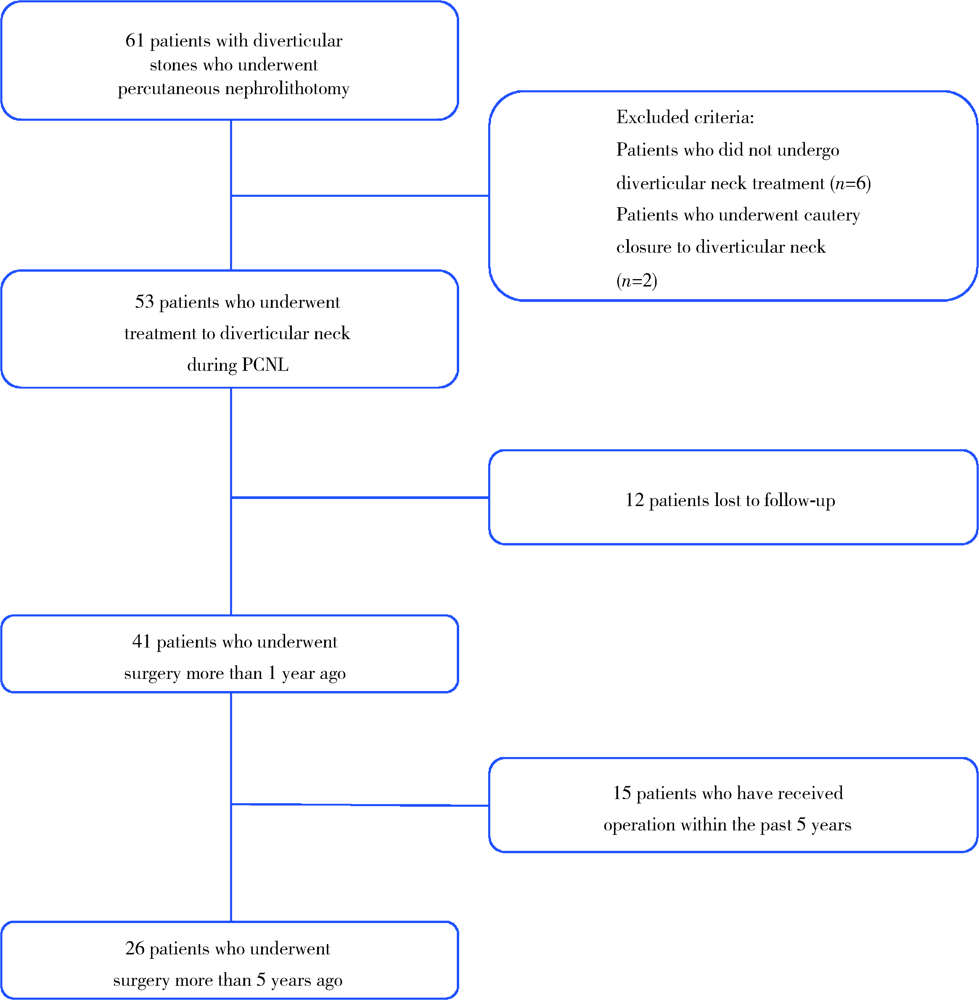
Comparison of long-term outcomes in different managements of diverticular neck in percutaneous nephrolithotomy for diverticular calculi
DAI Xiang,ZUO Mei-ni,ZHANG Xiao-peng,HU Hao( ),XU Tao
),XU Tao
- Department of Urology, Peking University People’s Hospital, Beijing 100044, China
CLC Number:
- R692.4
| [1] |
Waingankar N, Hayek S, Smith AD, et al. Calyceal diverticula: a comprehensive review [J]. Rev Urol, 2014, 16(1):29-43.
pmid: 24791153 |
| [2] |
Parkhomenko E, Tran T, Thai J, et al. Percutaneous management of stone containing calyceal diverticula: associated factors and outcomes [J]. J Urol, 2017, 198(4):864-868.
doi: S0022-5347(17)60624-4 pmid: 28483573 |
| [3] | Dretler S. A new useful endourologic classification of calyceal diverticula [J]. J Endourol, 1992, 6:6. |
| [4] |
McGarry L, Sahadev R, Hogan G, et al. Calyceal diverticula in children: laparoscopic marsupialization is the optimal intervention [J]. J Pediatr Urol, 2020, 16(2): 221.e1-221.e6.
doi: 10.1016/j.jpurol.2020.01.014 |
| [5] |
Bas O, Ozyuvali E, Aydogmus Y, et al. Management of calyceal diverticular calculi: a comparison of percutaneous nephrolithotomy and flexible ureterorenoscopy [J]. Urolithiasis, 2015, 43(2):155-161.
doi: 10.1007/s00240-014-0725-5 |
| [6] |
Turna B, Raza A, Moussa S, et al. Management of calyceal diverticular stones with extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy: long-term outcome [J]. BJU Int, 2007, 100(1):151-156.
doi: 10.1111/bju.2007.100.issue-1 |
| [7] | Yang H, Yao X, Tang C, et al. Flexible Ureterorenoscopy management of calyceal diverticular calculi [J]. Urol J, 2019, 16(1):12-15. |
| [8] | Zhang JQ, Wang Y, Zhang JH, et al. Retrospective analysis of ultrasound-guided flexible ureteroscopy in the management of calyceal diverticular calculi [J]. Chin Med J (Engl), 2016, 129(17):2067-2073. |
| [9] | Elsamra S, Motato H, Friedlander J, et al. 1 675 percutaneous treatment of calyceal diverticulum: access, stone extraction, and fulguration [J]. J Urol, 2013, 189(4):e689. |
| [10] |
Boonyapalanant C, Saksirisampant P, Taweemonkongsap T, et al. Factors impacting stone-free rate after retrograde intrarenal surgery for calyceal diverticular calculi [J]. Res Rep Urol, 2020, 12:345-350.
doi: 10.2147/RRU.S265959 pmid: 32903933 |
| [11] | 王强, 孙家庆, 晁亮, 等. 经皮肾镜超声碎石清石联合自制钩状电极一期治疗肾盏憩室结石 [J]. 中华腔镜泌尿外科杂志:电子版, 2013, 7(1):33-36. |
| [12] |
Donnellan SM, Harewood LM, Webb DR. Percutaneous management of caliceal diverticular calculi: technique and outcome [J]. J Endourol, 1999, 13(2):83-88.
pmid: 10213100 |
| [1] | Ming-rui WANG,Qi WANG,Hao HU,Jin-hui LAI,Yong-xin HE,Jie XIONG,Xian-hui LIU,Shi-jun LIU,Ke-xin XU,Tao XU. Long-term analysis of safety and efficacy of standard percutaneous nephrolithotomy in patients with solitary kidneys [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 663-666. |
| [2] | SHEN Cheng, ZHANG Bo, HAN Wen-ke, LIN Jian, WANG Gang, ZHANG Xiao-chun, SONG Yi, ZHAO Zheng, ZHANG Zhong-yuan, JIN Jie, YU Wei. Percutaneous renal access for percutaneous nephrolithotomy guided by contrast enhanced ultrasound: a single-center preliminary experience in China [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1071-1075. |
| [3] | YU Lu-ping, XU Tao. Analysis of development, safety and efficacy of percutaneous nephrolithotomy for management of upper urinary tract calculi in pediatric patients [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 626-631. |
|
||