Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 793-797. doi: 10.19723/j.issn.1671-167X.2021.04.029
Previous Articles Next Articles
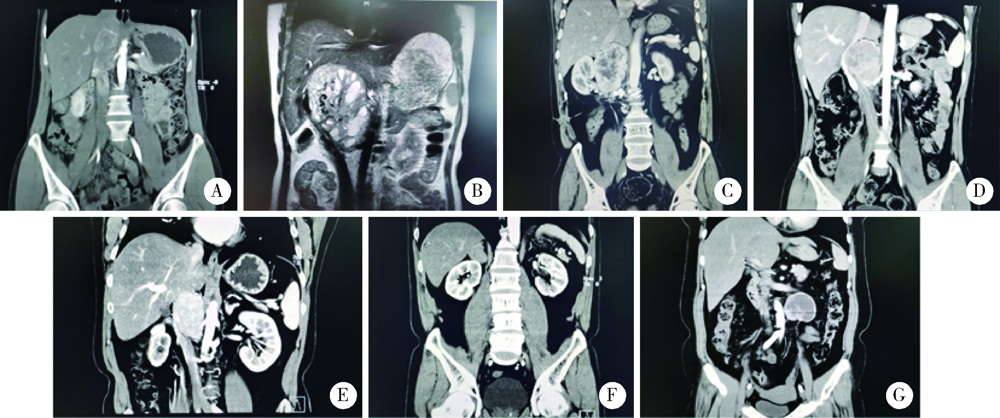
Strategy of reoperation for pheochromocytoma and paraganglioma
LIU Lei,QIN Yan-chun,WANG Guo-liang,ZHANG Shu-dong,HOU Xiao-fei,MA Lu-lin( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.1
| [1] |
Hamidi O, Young WF Jr., Iñiguez-Ariza NM, et al. Malignant pheochromocytoma and paraganglioma: 272 patients over 55 years [J]. J Clin Endocrinol Metab, 2017, 102(9):3296-3305.
doi: 10.1210/jc.2017-00992 |
| [2] |
Davison AS, Jones DM, Ruthven S, et al. Clinical evaluation and treatment of phaeochromocytoma [J]. Ann Clin Biochem, 2018, 55(1):34-48.
doi: 10.1177/0004563217739931 pmid: 29027806 |
| [3] |
Hamidi O, Young WF Jr., Gruber L, et al. Outcomes of patients with metastatic phaeochromocytoma and paraganglioma: A syste-matic review and meta-analysis [J]. Clin Endocrinol (Oxf), 2017, 87(5):440-450.
doi: 10.1111/cen.2017.87.issue-5 |
| [4] |
Lam AK. Update on adrenal tumours in 2017 World Health Orga-nization (WHO) of endocrine tumours [J]. Endocr Pathol, 2017, 28(3):213-227.
doi: 10.1007/s12022-017-9484-5 |
| [5] |
Wilhelm SM, Prinz RA, Barbu AM, et al. Analysis of large versus small pheochromocytomas: Operative approaches and patient outcomes [J]. Surgery, 2006, 140(4):553-560.
doi: 10.1016/j.surg.2006.07.008 |
| [6] |
Amar L, Servais A, Gimenez-Roqueplo AP, et al. Year of diagnosis, features at presentation, and risk of recurrence in patients with pheochromocytoma or secreting paraganglioma [J]. J Clin Endocrinol Metab, 2005, 90(4):2110-2116.
doi: 10.1210/jc.2004-1398 |
| [7] |
Edstrom Elder E, Hjelm Skog AL, Hoog A, et al. The management of benign and malignant pheochromocytoma and abdominal paraganglioma [J]. Eur J Surg Oncol, 2003, 29(3):278-283.
doi: 10.1053/ejso.2002.1413 |
| [8] |
Sbardella E, Grossman AB. Pheochromocytoma: An approach to diagnosis [J]. Best Pract Res Clin Endocrinol Metab, 2020, 34(2):101346.
doi: S1521-690X(19)30097-1 pmid: 31708376 |
| [9] |
Sonbare DJ, Abraham DT, Rajaratnam S, et al. Re-operative surgery for pheochromocytoma-paraganglioma: Analysis of 13 cases from a single institution [J]. Indian J Surg, 2018, 80(2):123-127.
doi: 10.1007/s12262-017-1658-3 pmid: 29915477 |
| [10] | Aggeli C, Nixon AM, Parianos C, et al. Surgery for pheochromocytoma: A 20-year experience of a single institution [J]. Hormones (Athens), 2017, 16(4):388-395. |
| [11] |
Hassan T, de la Taille A, Ingels A. Right robot-assisted partial adrenalectomy for pheochromocytoma with video [J]. J Visc Surg, 2020, 157(3):259-260.
doi: S1878-7886(20)30057-6 pmid: 32198067 |
| [12] |
Soejima Y, Yoshizumi T, Ikegami T, et al. Surgical resection of giant pheochromocytomas arising behind the retrohepatic inferior vena cava [J]. Anticancer Res, 2017, 37(1):277-280.
pmid: 28011503 |
| [1] | Yuqing LI,Biao WANG,Peng QIAO,Wei WANG,Xing GUAN. Medium to long-term efficacy of tension-free vaginal tape procedure in the treatment of female recurrent stress urinary incontinence [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 600-604. |
| [2] | Chieko MORIMOTO,Yi-qin WANG,Rong ZHOU,Jian-liu WANG. Clinical analysis of fertility-sparing therapy of patients with complex atypical hyperplasia and endometrial cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 936-942. |
| [3] | Yue WANG,Shuang ZHANG,Hong ZHANG,Li LIANG,Ling XU,Yuan-jia CHENG,Xue-ning DUAN,Yin-hua LIU,Ting LI. Clinicopathological features and prognosis of hormone receptor-positive/human epidermal growth factor receptor 2-negative breast cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 853-862. |
| [4] | Su-hua CHEN,Jun YANG,Xin CHEN,Chen-long YANG,Jian-jun SUN,Guo-zhong LIN,Tao YU,Xin YANG,Yun-feng HAN,Chao WU,Yu SI,Kai-ming MA. Surgical treatment of large and giant recurrent meningiomas near the middle and posterior third part of the superior sagittal sinus with extracranial invading [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1006-1012. |
| [5] | Yan-fang JIANG,Jian WANG,Yong-jian WANG,Jia LIU,Yin PEI,Xiao-peng LIU,Ying-fang AO,Yong MA. Mid-to-long term clinical outcomes and predictors after anterior cruciate ligament revision [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 857-863. |
| [6] | Huan-bin YU,Wen-jie WU,Xiao-ming LV,Yan SHI,Lei ZHENG,Jian-guo ZHANG. 125I seed brachytherapy for recurrent salivary gland carcinoma after external radiotherapy [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 919-923. |
| [7] | Lu LIU,Jie TIAN,Kai WU,Ying GAO,Zheng ZHANG,Jun-qing ZHANG,Xiao-hui GUO. Clinical profile of pheochromocytoma and paraganglioma with normal plasma free metanephrines [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 614-620. |
| [8] | Xu-chu ZHANG,Jian-hua ZHANG,Rong-fu WANG,Yan FAN,Zhan-li FU,Ping YAN,Guang-yu ZHAO,Yan-xia BAI. Diagnostic value of 18F-FDG PET/CT and tumor markers (CEA, CA19-9, CA24-2) in recurrence and metastasis of postoperative colorectal moderately differentiated adenocarcinoma [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1071-1077. |
| [9] | Qi TANG,Rong-cheng LIN,Lin YAO,Zheng ZHANG,Han HAO,Cui-jian ZHANG,Lin CAI,Xue-song LI,Zhi-song HE,Li-qun ZHOU. Clinicopathologic features and prognostic analyses of locally recurrent renal cell carcinoma patients after initial surgery [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 628-631. |
| [10] | WU Kai1 ZHANG Yang, ZHANG Hong, TAN Zeng-huan2 GUO Xiao-hui, YANG Jian-mei. Germline gene testing of the RET, VHL, SDHD and SDHB genes in patients with pheochromocytoma/paraganglioma [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 634-639. |
| [11] | XING Yun-chao, XIONG Geng-yan, FANG Dong, ZHANG Zheng, CAI Lin, ZHANG Lei, HE Zhi-song, LI Xue-song, ZHOU Li-qun. Preoperative prognostic factors and preoperative risk stratification of upper tract urothelial carcinoma [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1032-1037. |
| [12] | YANG Ying-chao, LIU Guo-li, ZHOU Jing-wei, HU Hao, SHEN Dan-hua. Diagnosis and treatment of pheochromocytoma in pregnancy: a case report [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 370-372. |
| [13] | WANG Zi-yun, WU Xin-bao. Anterior dislocation of the fibula resulting from surgical malreduction: a case report [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 361-365. |
| [14] | ZHOU Hua, SUN Yu, WANG Shao-bo, ZHANG Feng-shan, ZHANG Li, PAN Sheng-fa, ZHOU Fei-fei. Reoperation for cervical myelopathy duo to progressing ossification of the posterior longitudinal ligaments in patients with expansive laminoplasty [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 210-214. |
| [15] | LIU Yu-Qing, LU Jian, ZHAO Lei, HOU Xiao-Fei, MA Lu-Lin. Prognostic factors for intravesical recurrence after surgery for upper tract urothelial carcinoma in renal transplant recipients [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 605-610. |
|
||