Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (5): 1021-1027. doi: 10.19723/j.issn.1671-167X.2022.05.032
Previous Articles Next Articles
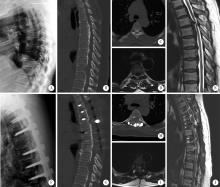
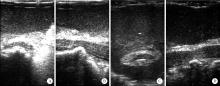
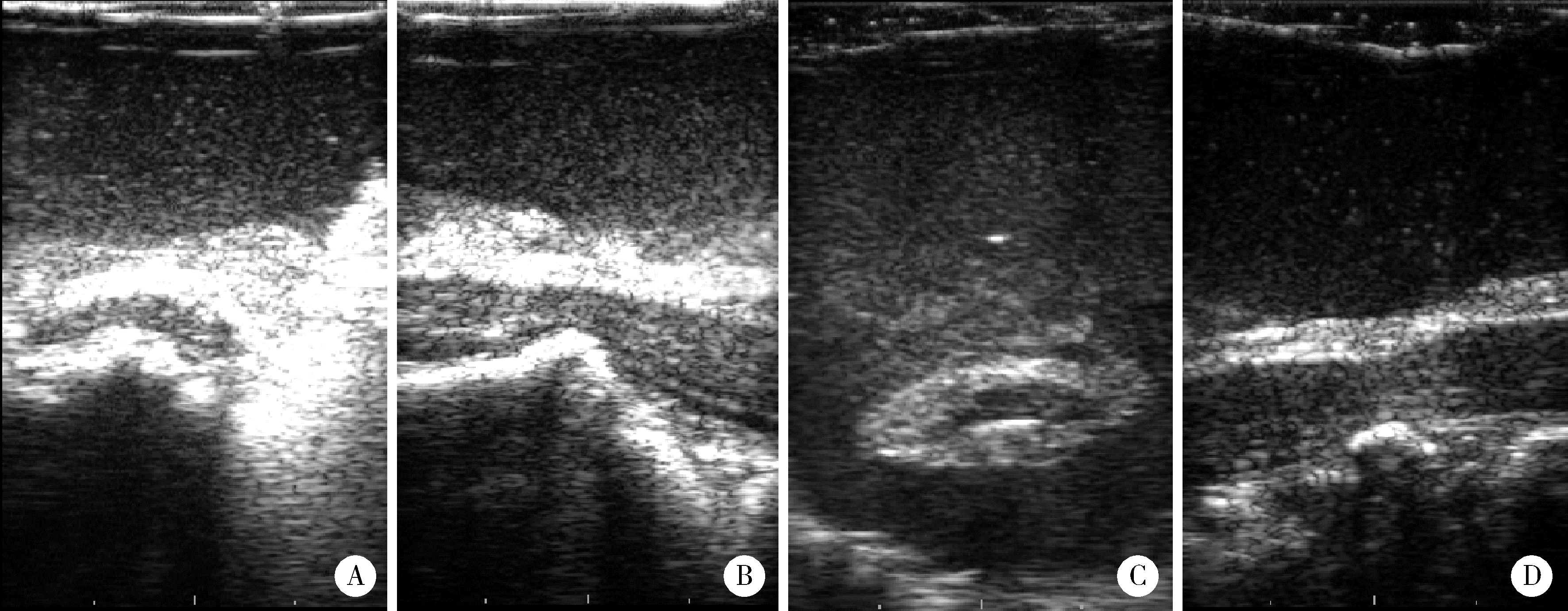
Intraoperative ultrasound assisted circumferential decompression for multilevel ossification of the posterior longitudinal ligament in thoracic vertebrae
Shu-heng ZHAI,Pan-pan HU,Xiao-guang LIU*( )
)
- Department of Orthopaedics, Peking University Third Hospital; Engineering Research Center of Bone and Joint Precision Medicine; Beijing Key Laboratory of Spinal Disease Research, Beijing 100191, China
CLC Number:
- R61
| 1 |
Chen G , Fan T , Yang X , et al. The prevalence and clinical characteristics of thoracic spinal stenosis: A systematic review[J]. Eur Spine J, 2020, 29 (9): 2164- 2172.
doi: 10.1007/s00586-020-06520-6 |
| 2 |
Hou X , Sun C , Liu X , et al. Clinical features of thoracic spinal stenosis-associated myelopathy: A retrospective analysis of 427 cases[J]. Clin Spine Surg, 2016, 29 (2): 86- 89.
doi: 10.1097/BSD.0000000000000081 |
| 3 | Ando K, Nakashima H, Machino M, et al. Postoperative progression of ligamentum flavum ossification after posterior instrumented surgery for thoracic posterior longitudinal ligament ossification: Long-term outcomes during a minimum 10-year follow-up [J/OL]. J Neurosurg Spine, 2021(2021-12-24)[2022-06-01]. https://pubmed.ncbi.nlh.gov/34952516/. |
| 4 |
Kato S , Murakami H , Demura S , et al. Indication for anterior spinal cord decompression via a posterolateral approach for the treatment of ossification of the posterior longitudinal ligament in the thoracic spine: A prospective cohort study[J]. Eur Spine J, 2020, 29 (1): 113- 121.
doi: 10.1007/s00586-019-06047-5 |
| 5 |
刘晓光. 胸椎管狭窄症的手术技术要点[J]. 中国脊柱脊髓杂志, 2017, 27 (7): 670- 672.
doi: 10.3969/j.issn.1004-406X.2017.07.17 |
| 6 |
刘晓光, 刘忠军, 陈仲强, 等. "涵洞塌陷法"360°脊髓环形减压术治疗胸椎管狭窄症[J]. 中华骨科杂志, 2010, 30 (11): 1059- 1062.
doi: 10.3760/cma.j.issn.0253-2352.2010.11.010 |
| 7 |
Zheng C , Zhu Y , Lyu F , et al. Motor-evoked potentials in the intraoperative decision-making of circumferential decompression via posterior approach for treating thoracic posterior longitudinal ligament ossification[J]. Spine J, 2021, 21 (7): 1168- 1175.
doi: 10.1016/j.spinee.2021.01.023 |
| 8 |
Hu P , Yu M , Liu X , et al. A circumferential decompression-based surgical strategy for multilevel ossification of thoracic posterior longitudinal ligament[J]. Spine J, 2015, 15 (12): 2484- 2492.
doi: 10.1016/j.spinee.2015.08.060 |
| 9 |
Yang P , Ge R , Chen ZQ , et al. Treatment of thoracic ossification of posterior longitudinal ligament with one-stage 360 degree circumferential decompression assisted by piezosurgery[J]. J Invest Surg, 2022, 35 (2): 249- 256.
doi: 10.1080/08941939.2020.1839149 |
| 10 |
Gao A , Yu M , Wei F , et al. One-stage posterior surgery with intraoperative ultrasound assistance for thoracic myelopathy with simultaneous ossification of the posterior longitudinal ligament and ligamentum flavum at the same segment: A minimum 5-year follow-up study[J]. Spine J, 2020, 20 (9): 1430- 1437.
doi: 10.1016/j.spinee.2020.05.097 |
| 11 | Yang X, Liu X, Liu X, et al. Clinical outcomes of intraoperative contrast-enhanced ultrasound compared with intraoperative neurophysiological monitoring during circumferential decompression for myelopathy associated with thoracic-ossification of the posterior longitudinal ligament [J/OL]. Med Sci Monit, 2020, 26: e921129(2020-04-29)[2022-06-22]. http://pubmid.ncbi.nlh.gov/32345957/. |
| 12 |
Hu P , Yu M , Liu X , et al. Cerebrospinal fluid leakage after surgeries on the thoracic spine: A review of 362 cases[J]. Asian Spine J, 2016, 10 (3): 472- 479.
doi: 10.4184/asj.2016.10.3.472 |
| 13 |
Hu PP , Liu XG , Yu M . Cerebrospinal fluid leakage after thoracic decompression[J]. Chin Med J (Engl), 2016, 129 (16): 1994- 2000.
doi: 10.4103/0366-6999.187854 |
| [1] | CHENG Cheng, TONG Huai-Yu, ZHANG Yuan-Zheng. Thoracic extramedullary subdural and epidural of inflammatory myofibroblastoma: a case report [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 333-335. |
|
||