Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (3): 450-455. doi: 10.19723/j.issn.1671-167X.2023.03.010
Previous Articles Next Articles
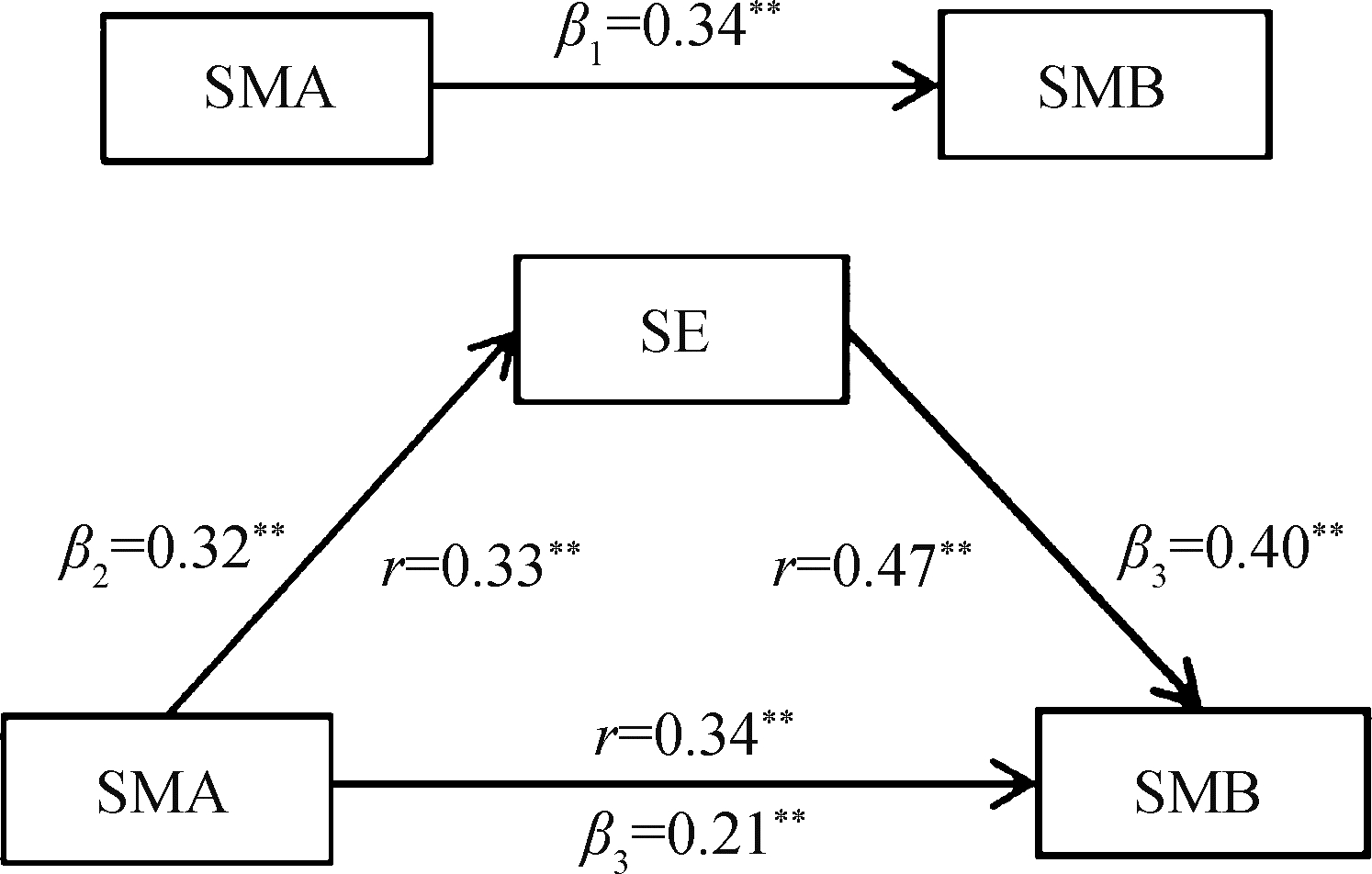
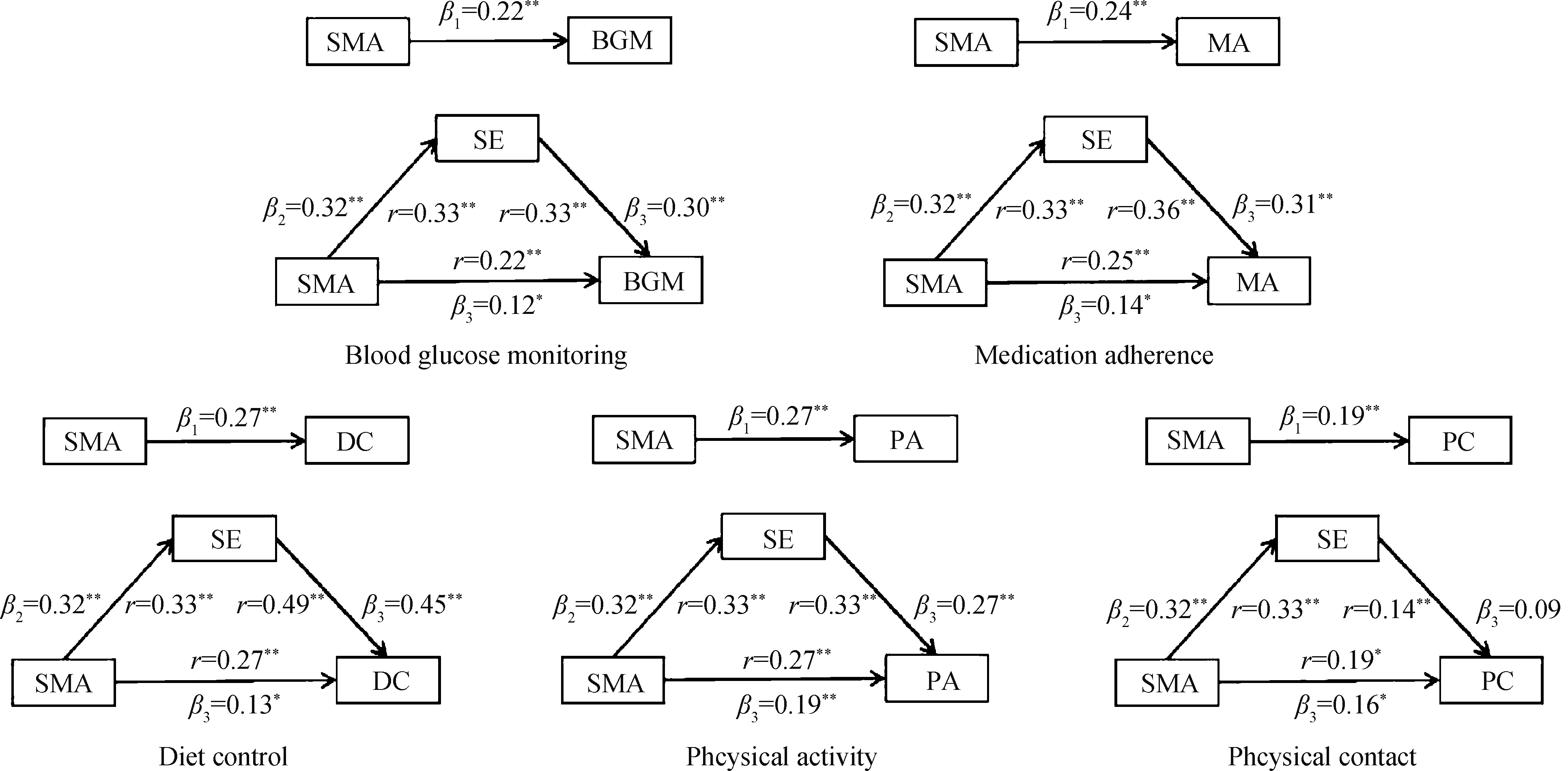
Mediating effect of self-efficacy on self-management ability and self-management behavior in patients with type 2 diabetes mellitus
Xiao-yue ZHANG1,Yu-xin LIN1,Ying JIANG2,Lan-chao ZHANG1,Mang-yan DONG3,Hai-yi CHI4,Hao-yu DONG5,Li-jun MA6,Zhi-jing LI1,Chun CHANG1,*( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. Bee Technology Limited Company, Beijing 100020, China
3. Department of Endocrinology, Houma People' s Hospital, Houma 043011, Shanxi, China
4. Department of Endocrinology, Hohhot First Hospital, Hohhot 010030, China
5. Department of Endocrinology, Heping Hospital Affiliated to Changzhi Medical College, Changzhi 046000, Shanxi, China
6. Department of Endocrinology, People' s Hospital of Xinrong District, Datong 037002, Shanxi, China
CLC Number:
- R193.3
| 1 | American Diabetes Association .Prevention or delay of type 2 diabetes: Standards of medical care in diabetes—2020[J].Diabetes Care,2020,43(Suppl 1):S32-S36. |
| 2 | American Diabetes Association .Lifestyle management: Standards of medical care in diabetes—2019[J].Diabetes Care,2019,42(Suppl 1):S46-S60. |
| 3 | Burford SJ , Park S , Dawda P .Small data and its visualization for diabetes self-management: Qualitative study[J].JMIR Diabetes,2019,21(8):e10324. |
| 4 | 李至韬, 李玟, 费宇, 等.职业人群的糖尿病及糖尿病前期患病现状及影响因素分析[J].现代预防医学,2021,48(12):2161-2165. |
| 5 | 曹俊, 林琴, 付梦雪, 等.近10年我国糖尿病病人自我管理现状、热点与趋势的可视化分析[J].护理研究,2019,33(6):937-940. |
| 6 |
Funnell MM , Anderson RM , Arnold MS , et al.Empowerment: An idea whose time has come in diabetes education[J].Diabetes Educ,1991,17(1):37-41.
doi: 10.1177/014572179101700108 |
| 7 | 叶会玲.授权理论在糖尿病教育中的应用现状[J].护理研究,2010,24(2):97-100. |
| 8 |
King DK , Glasgow RE , Toobert DJ , et al.Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors[J].Diabetes Care,2010,33(4):751-753.
doi: 10.2337/dc09-1746 |
| 9 |
Lee AA , Piette JD , Heisler M , et al.Diabetes self-management and glycemic control: The role of autonomy support from informal health supporters[J].Health Psychol,2019,38(2):122-132.
doi: 10.1037/hea0000710 |
| 10 | 李超群, 井坤娟, 刘昱莹, 等.糖尿病自我管理量表的汉化及信效度评价[J].现代预防医学,2018,45(24):4477-4481. |
| 11 |
Ritter PL , Lorig K , Laurent DD .Characteristics of the Spanish- and English-language self-efficacy to manage diabetes scales[J].Diabetes Educ,2016,42(2):167-177.
doi: 10.1177/0145721716628648 |
| 12 | 刘红云, 温忠麟, 张雷, 等.中介效应检验程序及其应用[J].心理学报,2004,36(5):614-620. |
| 13 | Chiou S , Liao K , Lin K , et al.Using patient health profile evaluation for predicting the likelihood of retinopathy in patients with type 2 diabetes: A cross-sectional study using latent profile analysis[J].Int J Environ Res Public Health,2022,19(10):6084. |
| 14 | Boussageon R , Pouchain D , Renard V .Prevention of complications in type 2 diabetes: Is drug glucose control evidence based?[J].Br J Gen Pract,2017,67(655):85-87. |
| 15 | 麻倩, 郭玉芳, 井坤娟.糖尿病患者自我管理现状及影响因素研究[J].现代预防医学,2019,46(5):915-920. |
| 16 | Lee Y , Shin S , Wang R , et al.Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus[J].Patient Educ Couns,2016,99(2):287-294. |
| 17 | van Smoorenburg AN , Hertroijs DFL , Dekkers T , et al.Patients' perspective on self-management: Type 2 diabetes in daily life[J].BMC Health Serv Res,2019,19(1):605. |
| 18 | 刘彩云, 尤莉莉.社会认知理论在促进糖尿病和糖尿病前期患者体力活动中的应用[J].中国健康教育,2021,37(11):1037-1040. |
| 19 | 丁贤彬, 张春华, 沈卓之, 等.健康自我管理对糖尿病患者不同自我效能的影响[J].实用预防医学,2016,23(11):1322-1325. |
| 20 | 张洁, 苏丹婷, 陆凤, 等.社区自我管理小组对糖尿病患者自我效能的远期影响研究[J].中国健康教育,2022,38(2):140-144. |
| [1] | Lei BAO,Xia-xia CAI,Ming-yuan ZHANG,Lei-lei REN. Effect of vitamin D3 on mild cognitive impairment in type 2 diabetic mice and its possible mechanism [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 587-592. |
| [2] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [3] | CHEN Ping,LI Ze-ming,GUO Yi,SUN Xin-ying,Edwin B. FISHER. To explore medication adherence of patients with type 2 diabetes mellitus using the latent profile analysis based on the Big Five personality theory [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 530-535. |
| [4] | Ze-ming LI,Min GAO,Xue-ying CHEN,Xin-ying SUN. Relationship between the five-factor model of personality traits and self-management attitude of patients with type 2 diabetes [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 506-513. |
| [5] | Jiang XIE,Fei LI. Association of sleep overlap syndrome with type 2 diabetes in a cross-sectional study [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 252-255. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 311
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 513
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||