Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (1): 161-166. doi: 10.19723/j.issn.1671-167X.2024.01.025
Previous Articles Next Articles
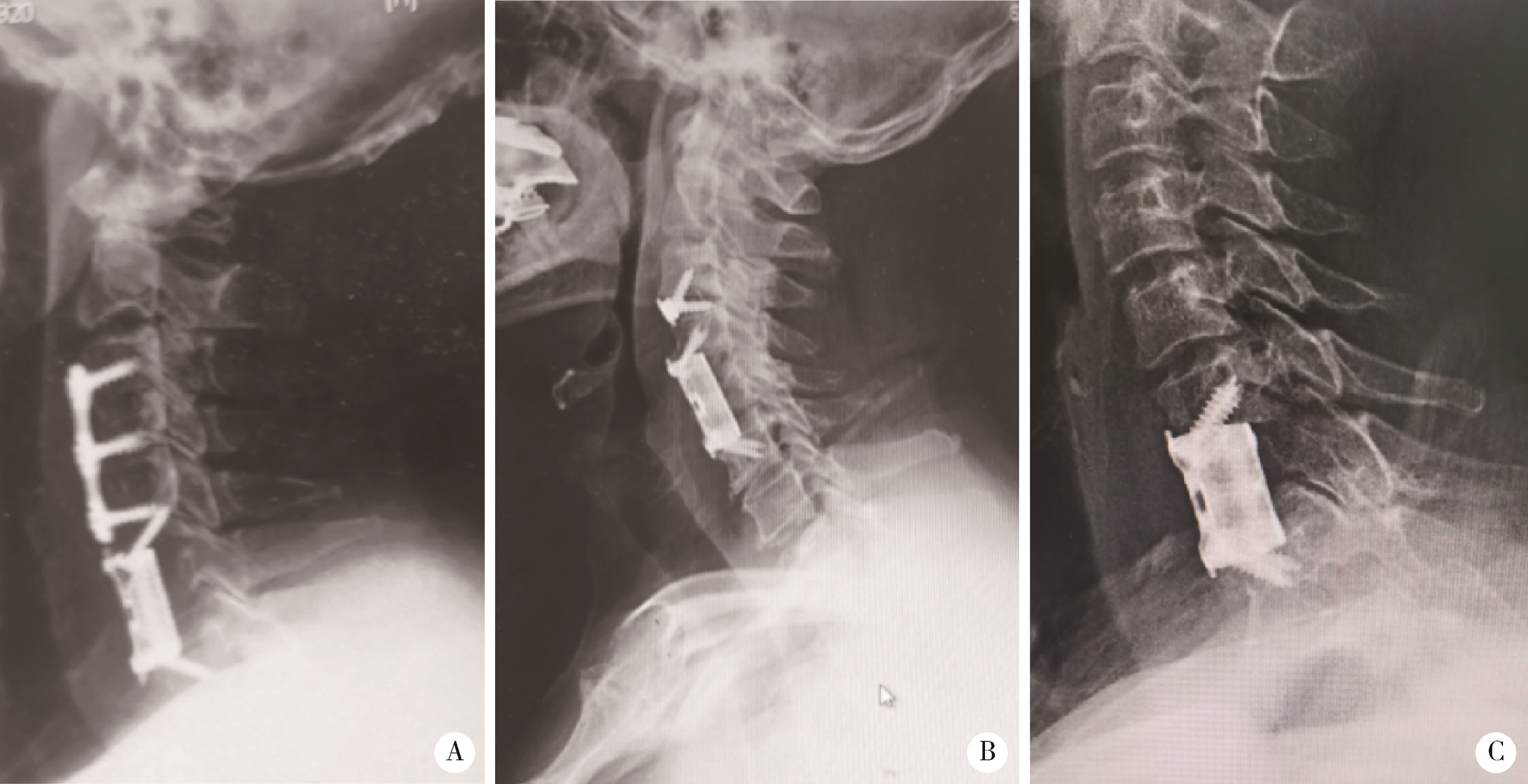
Clinical outcomes of 3D-printing stand-alone artificial vertebral body in anterior cervical surgeries
Panpan HU,Yan LI,Xiao LIU,Yanchao TANG,Zihe LI,Zhongjun LIU*( )
)
- Department of Orthopaedics, Peking University Third Hospital; Engineering Research Center of Bone and Joint Precision Medicine; Beijing Key Laboratory of Spinal Disease Research, Beijing 100191, China
CLC Number:
- R687.3
| 1 |
Lv Y , Tian W , Chen D , et al. The prevalence and associated factors of symptomatic cervical spondylosis in Chinese adults: A community-based cross-sectional study[J]. BMC Musculoskelet Disord, 2018, 19 (1): 325.
doi: 10.1186/s12891-018-2234-0 |
| 2 |
Bakhsheshian J , Mehta VA , Liu JC . Current diagnosis and management of cervical spondylotic myelopathy[J]. Global Spine J, 2017, 7 (6): 572- 586.
doi: 10.1177/2192568217699208 |
| 3 | 蔡钦林. 颈椎病的手术治疗(一)[J]. 中国脊柱脊髓杂志, 1996, (2): 42- 45. |
| 4 |
Böhler J , Gaudernak T . Anterior plate stabilization for fracture-dislocations of the lower cervical spine[J]. J Trauma, 1980, 20 (3): 203- 205.
doi: 10.1097/00005373-198003000-00002 |
| 5 | Orozco-Declos R , Llovet-Tapies J . Osteosintesis en las fracturas del raquis cervical: Nota técnica[J]. Rev Ortop Traumatol, 1970, 14, 285- 288. |
| 6 | 袁文, 贾连顺, 倪斌. 前路椎体次全切除减压及带锁钢板固定治疗脊髓型颈椎病[J]. 中华外科杂志, 2000, 38 (3): 182- 184. |
| 7 |
毛志国, 袁文, 贾连顺, 等. 钛质网笼内植物加前路带锁钢板对颈椎稳定性的生物力学评价[J]. 中国脊柱脊髓杂志, 2001, 11 (6): 355- 357.
doi: 10.3969/j.issn.1004-406X.2001.06.010 |
| 8 |
Qin R , Chen X , Zhou P , et al. Anterior cervical corpectomy and fusion versus posterior laminoplasty for the treatment of oppressive myelopathy owing to cervical ossification of posterior longitudinal ligament: A meta-analysis[J]. Eur Spine J, 2018, 27 (6): 1375- 1387.
doi: 10.1007/s00586-017-5451-6 |
| 9 |
Wang T , Tian XM , Liu SK , et al. Prevalence of complications after surgery in treatment for cervical compressive myelopathy: A meta-analysis for last decade[J]. Medicine (Baltimore), 2017, 96 (12): e6421.
doi: 10.1097/MD.0000000000006421 |
| 10 |
Lin Q , Zhou X , Wang X , et al. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy[J]. Eur Spine J, 2012, 21 (3): 474- 481.
doi: 10.1007/s00586-011-1961-9 |
| 11 |
Joaquim AF , Murar J , Savage JW , et al. Dysphagia after anterior cervical spine surgery: A systematic review of potential preventative measures[J]. Spine J, 2014, 14 (9): 2246- 2260.
doi: 10.1016/j.spinee.2014.03.030 |
| 12 | Barbagallo GM , Romano D , Certo F , et al. Zero-P: A new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices[J]. Eur Spine J, 2013, 22 (Suppl 6): S868- S878. |
| 13 |
Njoku I Jr , Alimi M , Leng LZ , et al. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: A clinical and radiological study[J]. J Neurosurg Spine, 2014, 21 (4): 529- 537.
doi: 10.3171/2014.6.SPINE12951 |
| 14 |
Tohamy MH , Osterhoff G , Abdelgawaad AS , et al. Anterior cervical corpectomy and fusion with stand-alone cages in patients with multilevel degenerative cervical spine disease is safe[J]. BMC Musculoskelet Disord, 2022, 23 (1): 20.
doi: 10.1186/s12891-021-04883-5 |
| 15 | Zhou H , Liu S , Li Z , et al. 3D-printed vertebral body for anterior spinal reconstruction in patients with thoracolumbar spinal tumors[J]. J Neurosurg Spine, 2022, 25, 1- 9. |
| 16 |
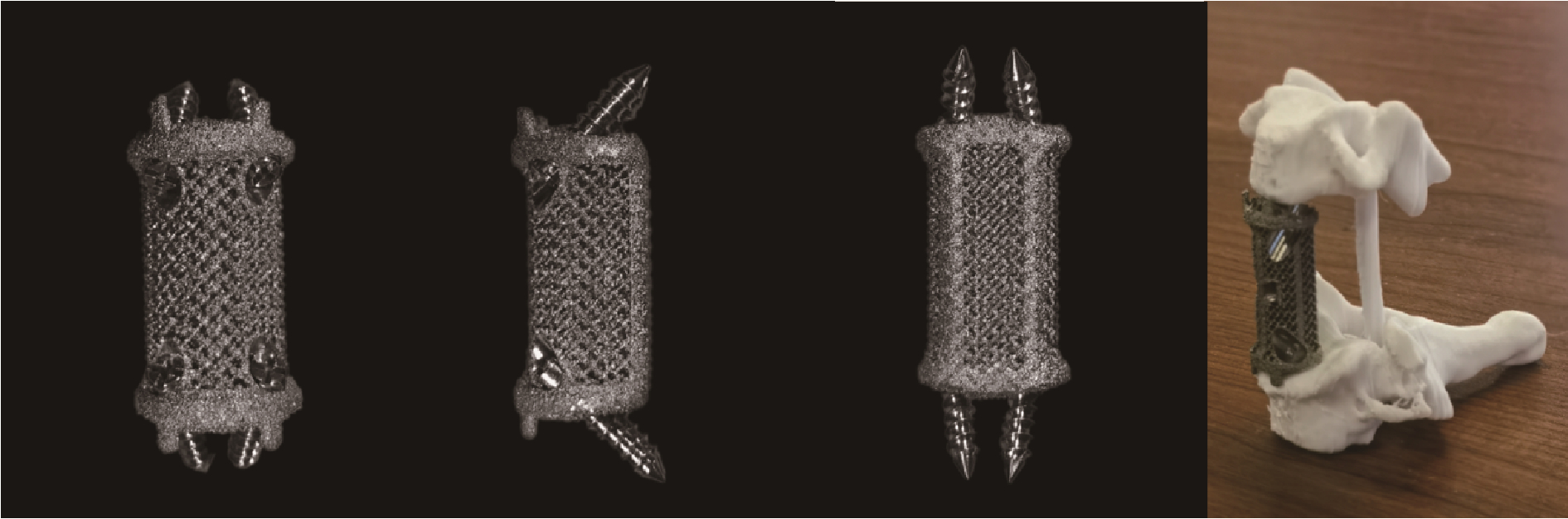
Hu P , Du S , Wei F , et al. Reconstruction after resection of C2 vertebral tumors: A comparative study of 3D-printed vertebral body versus titanium mesh[J]. Front Oncol, 2022, 12, 1065303.
doi: 10.3389/fonc.2022.1065303 |
| 17 |
Yang J , Cai H , Liu Z , et al. In vivo study of a self-stabilizing artificial vertebral body fabricated by electron beam melting[J]. Spine (Phila Pa 1976), 2014, 39 (8): E486- E492.
doi: 10.1097/BRS.0000000000000211 |
| 18 |
Bazaz R , Lee MJ , Yoo JU . Incidence of dysphagia after anterior cervical spine surgery: A prospective study[J]. Spine (Phila Pa 1976), 2002, 27 (22): 2453- 2458.
doi: 10.1097/00007632-200211150-00007 |
| 19 |
Kanayama M , Hashimoto T , Shigenobu K , et al. Pitfalls of anterior cervical fusion using titanium mesh and local autograft[J]. J Spinal Disord Tech, 2003, 16 (6): 513- 518.
doi: 10.1097/00024720-200312000-00005 |
| 20 |
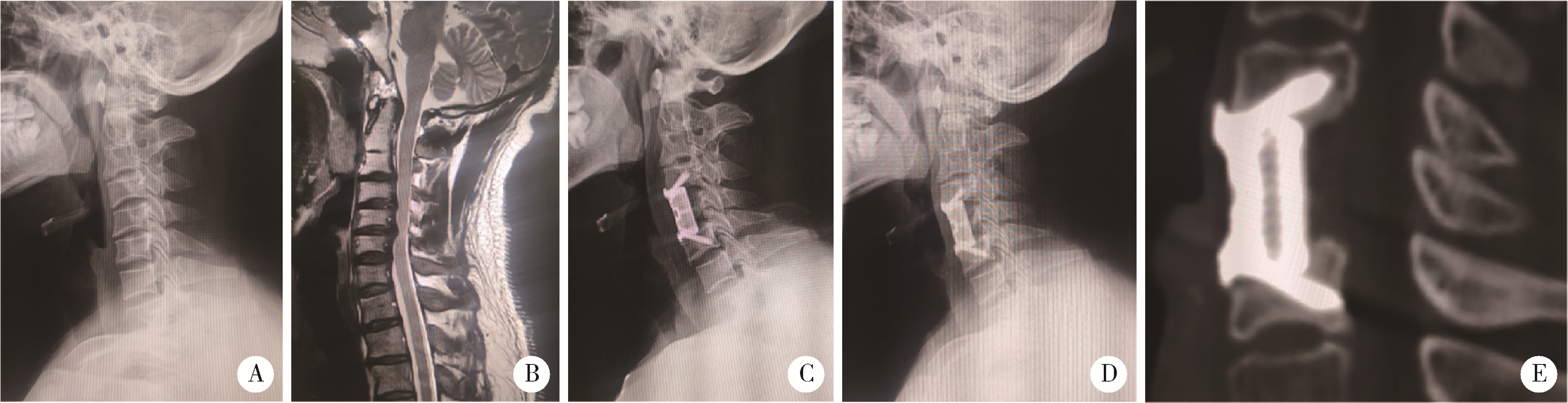
Wei F , Xu N , Li Z , et al. A prospective randomized cohort study on 3D-printed artificial vertebral body in single-level anterior cervical corpectomy for cervical spondylotic myelopathy[J]. Ann Transl Med, 2020, 8 (17): 1070.
doi: 10.21037/atm-19-4719 |
| 21 |
Liu Y , Qi M , Chen H , et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy[J]. Eur Spine J, 2012, 21 (12): 2428- 2435.
doi: 10.1007/s00586-012-2323-y |
| 22 |
Ji C , Yu S , Yan N , et al. Risk factors for subsidence of titanium mesh cage following single-level anterior cervical corpectomy and fusion[J]. BMC Musculoskelet Disord, 2020, 21 (1): 32.
doi: 10.1186/s12891-019-3036-8 |
| 23 |
Mohammad-Shahi MH , Nikolaou VS , Giannitsios D , et al. The effect of angular mismatch between vertebral endplate and vertebral body replacement endplate on implant subsidence[J]. J Spinal Disord Tech, 2013, 26 (5): 268- 273.
doi: 10.1097/BSD.0b013e3182425eab |
| 24 |
Chen Y , Chen D , Guo Y , et al. Subsidence of titanium mesh cage: A study based on 300 cases[J]. J Spinal Disord Tech, 2008, 21 (7): 489- 492.
doi: 10.1097/BSD.0b013e318158de22 |
| 25 |
Cheng H , Luo G , Xu D , et al. Comparison of radiological and clinical outcomes of 3D-printed artificial vertebral body with titanium mesh cage in single-level anterior cervical corpectomy and fusion: A meta-analysis[J]. Front Surg, 2023, 9, 1077551.
doi: 10.3389/fsurg.2022.1077551 |
| 26 |
Jiang SD , Jiang LS , Dai LY . Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for multilevel cervical spondylosis: A systematic review[J]. Arch Orthop Trauma Surg, 2012, 132 (2): 155- 161.
doi: 10.1007/s00402-011-1402-6 |
| 27 |
Riley LH 3rd , Skolasky RL , Albert TJ , et al. Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study[J]. Spine (Phila Pa 1976), 2005, 30 (22): 2564- 2569.
doi: 10.1097/01.brs.0000186317.86379.02 |
| [1] | Hua ZHOU,Ren-ji WANG,Zhong-jun LIU,Xiao-guang LIU,Feng-liang WU,Lei DANG,Feng WEI. 3D-printed vertebral body in anterior spinal reconstruction after total spondylectomy for patients with cervical chordoma [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 144-148. |
|
||