Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (2): 366-370. doi: 10.19723/j.issn.1671-167X.2024.02.027
Previous Articles Next Articles
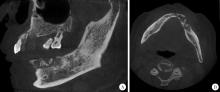
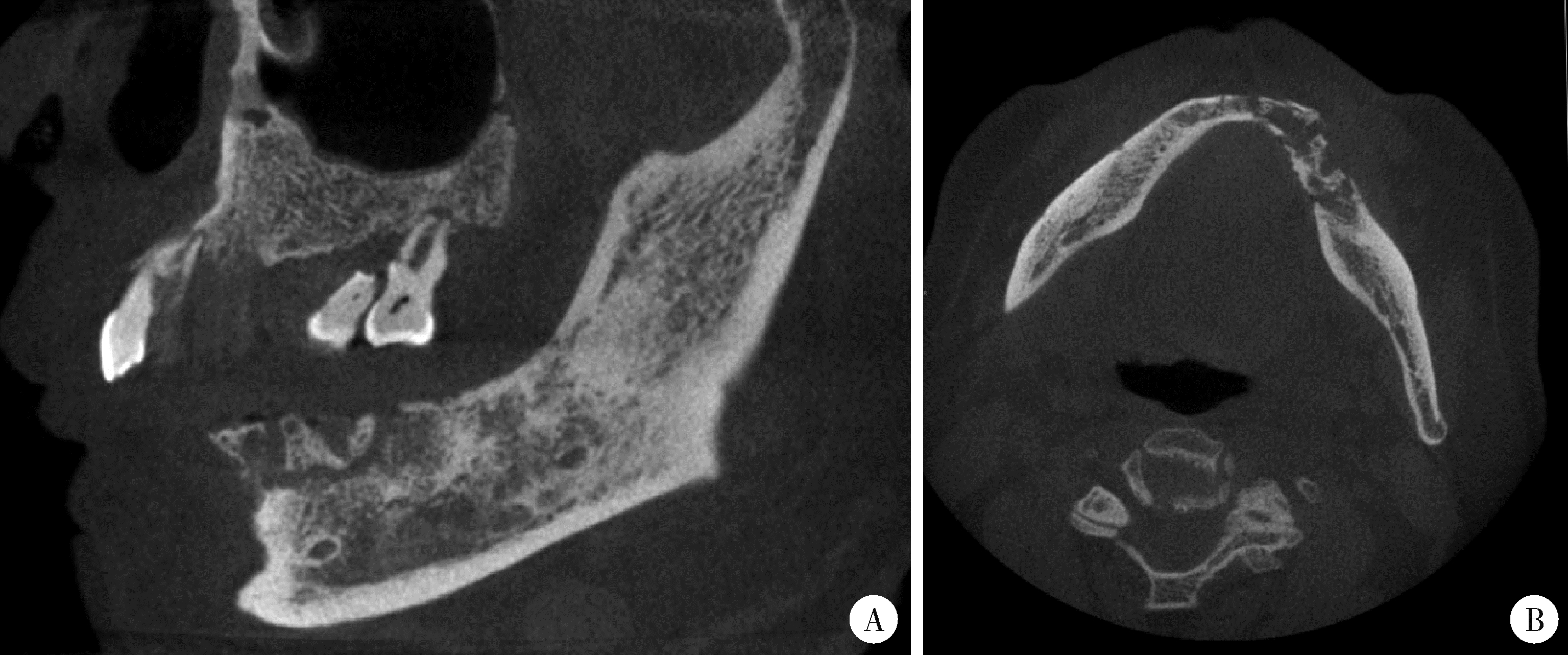
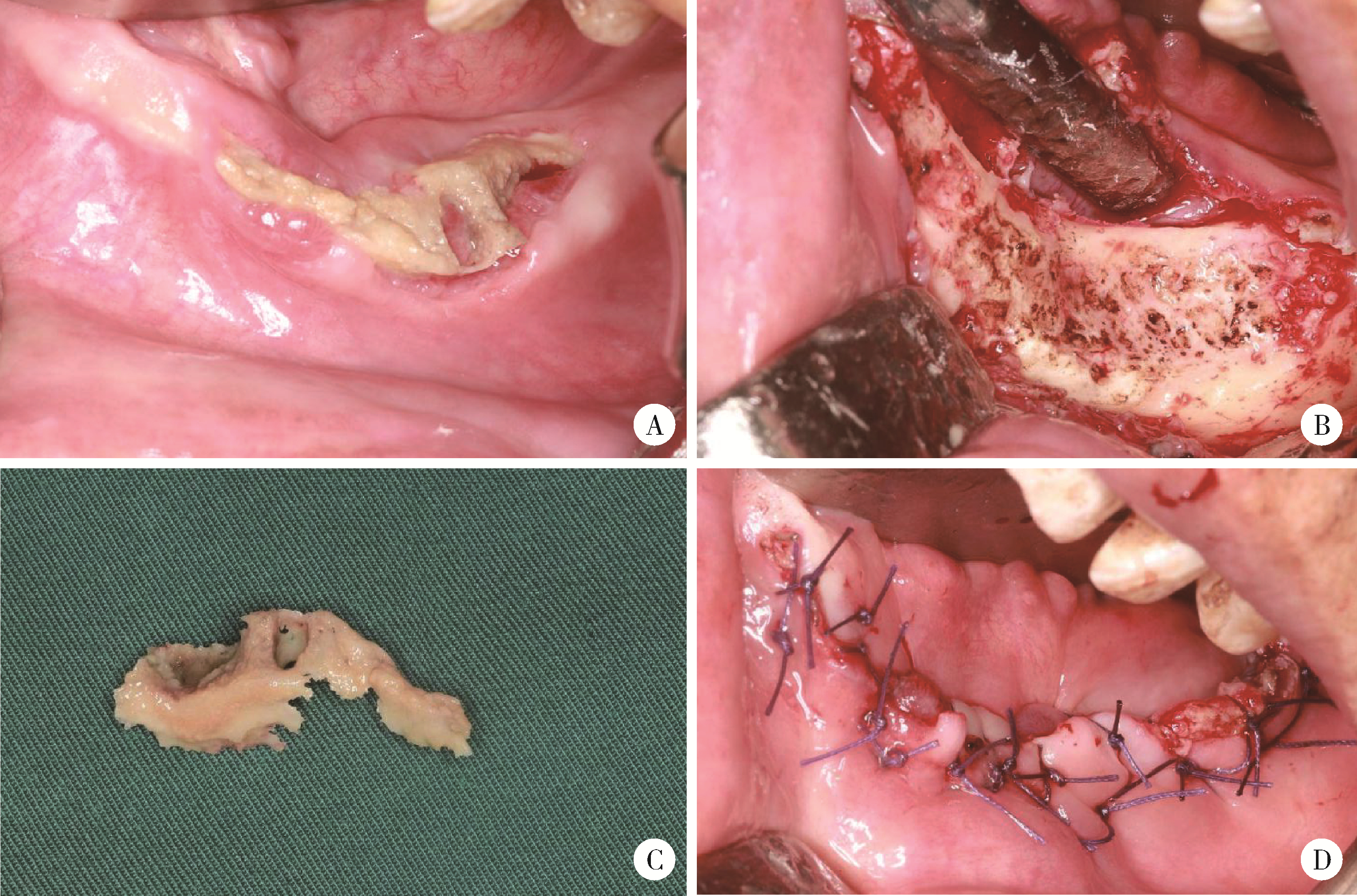
Left mandibular osteonecrosis following herpes zoster of the third branch of left trigeminal nerve: A case report
Ying ZHOU,Ning ZHAO,Hongyuan HUANG,Qingxiang LI,Chuanbin GUO,Yuxing GUO*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing 100081, China
CLC Number:
- R782.3
| 1 |
Esposito S , Principi N . Herpes zoster prevention: A difficult pro-blem to solve[J]. Vaccine, 2018, 36 (36): 5442- 5448.
doi: 10.1016/j.vaccine.2017.07.099 |
| 2 | 中国医师协会皮肤科医师分会带状疱疹专家共识工作组. 带状疱疹中国专家共识[J]. 中华皮肤科杂志, 2018, 51 (6): 403- 408. |
| 3 | 中华医学会全科医学分会, 中华医学会杂志社, 中华医学会《中华全科医师杂志》编辑委员会, 等. 社区老年人常见感染性疾病疫苗应用专家共识[J]. 中华全科医师杂志, 2022, 21 (1): 6- 23. |
| 4 |
Ferreira ACAF , Romão TT , Macedo YS , et al. COVID-19 and herpes zoster co-infection presenting with trigeminal neuropathy[J]. Eur J Neurol, 2020, 27 (9): 1748- 1750.
doi: 10.1111/ene.14361 |
| 5 |
Pelloni LS , Pelloni R , Borradori L . Herpes zoster of the trigeminal nerve with multi-dermatomal involvement: A case report of an unusual presentation[J]. BMC Dermatol, 2020, 20 (1): 12.
doi: 10.1186/s12895-020-00110-1 |
| 6 |
Faure E , Engels-Deutsch M , Paraschiv EA , et al. Mandibular osteonecrosis following herpes zoster infection: Report of a rare case with a literature review[J]. Clin Case Rep, 2021, 9 (5): e04196.
doi: 10.1002/ccr3.4196 |
| 7 | 班建东, 王健, 侯燕, 等. 三叉神经带状疱疹合并不典型Ramsay Hunt综合征1例[J]. 实用口腔医学杂志, 2023, 39 (3): 396- 398. |
| 8 | Dechaume M , Descrozailles C , Garlopeau F , et al. Localized mandibular necrosis during trigeminal herpes[J]. Revue Stomatol, 1955, 56 (7): 516- 521. |
| 9 |
Gupta S , Sreenivasan V , Patil P . Dental complications of herpes zoster: Two case reports and review of literature[J]. Indian J Dent Res, 2015, 26 (2): 214.
doi: 10.4103/0970-9290.159175 |
| 10 | 王继华. 以三叉神经带状疱疹为始发症状的艾滋病24例报告[J]. 中国耳鼻咽喉颅底外科杂志, 1999, 5 (2): 41- 43. |
| 11 | Francis M , Subramanian K , Sankari SL . Herpes zoster with post herpetic neuralgia involving the right maxillary branch of trigeminal nerve: A case report and review of literature[J]. J Clin Diagn Res, 2017, 11 (1): 40- 42. |
| 12 | 施越琦, 李萌宇, 华洪飞, 等. 三叉神经带状疱疹罕见并发症颌骨坏死回顾分析[J]. 口腔医学, 2019, 39 (3): 240- 245. |
| 13 |
Wright WE , Davis ML , Geffen DB , et al. Alveolar bone necrosis and tooth loss: A rare complication associated with herpes zoster infection of the fifth cranial nerve[J]. Oral Surg Oral Med Oral Pathol, 1983, 56 (1): 39- 46.
doi: 10.1016/0030-4220(83)90053-1 |
| 14 |
Linnemann CC Jr. , Alvira MM . Pathogenesis of varicella-zoster angiitis in the CNS[J]. Arch Neurol, 1980, 37 (4): 239- 240.
doi: 10.1001/archneur.1980.00500530077013 |
| 15 |
Gilden D , Cohrs RJ , Mahalingam R , et al. Varicella zoster virus vasculopathies: Diverse clinical manifestations, laboratory features, pathogenesis, and treatment[J]. Lancet Neurol, 2009, 8 (8): 731- 740.
doi: 10.1016/S1474-4422(09)70134-6 |
| 16 |
Mintz SM , Anavi Y . Maxillary osteomyelitis and spontaneous tooth exfoliation after herpes zoster[J]. Oral Surg Oral Med Oral Pathol, 1992, 73 (6): 664- 666.
doi: 10.1016/0030-4220(92)90005-B |
| 17 |
Yin M , Huang P , Yang S , et al. Ramsay Hunt syndrome and mandibular alveolar bone necrosis following herpes zoster: A case report and literature review[J]. Front Neurol, 2022, 13, 1073607.
doi: 10.3389/fneur.2022.1073607 |
| 18 |
Weller TH . Varicella and herpes zoster. Changing concepts of the natural history, control, and importance of a not-so-benign virus[J]. N Engl J Med, 1983, 309 (22): 1362- 1368.
doi: 10.1056/NEJM198312013092205 |
| 19 | Shigeishi H , Sugiyama M , Ohta K . Relationship between the prevalence of oral human papillomavirus DNA and periodontal disease (Review)[J]. Biomed Rep, 2021, 14 (5): 40. |
| 20 | 汤江林, 徐新颜, 彭济勇, 等. 晚期癌症患者化疗后带状疱疹病毒感染状况分析[J]. 中华医院感染学杂志, 2018, 28 (3): 380- 383. |
|
||