Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (1): 51-56. doi: 10.19723/j.issn.1671-167X.2024.01.009
Previous Articles Next Articles
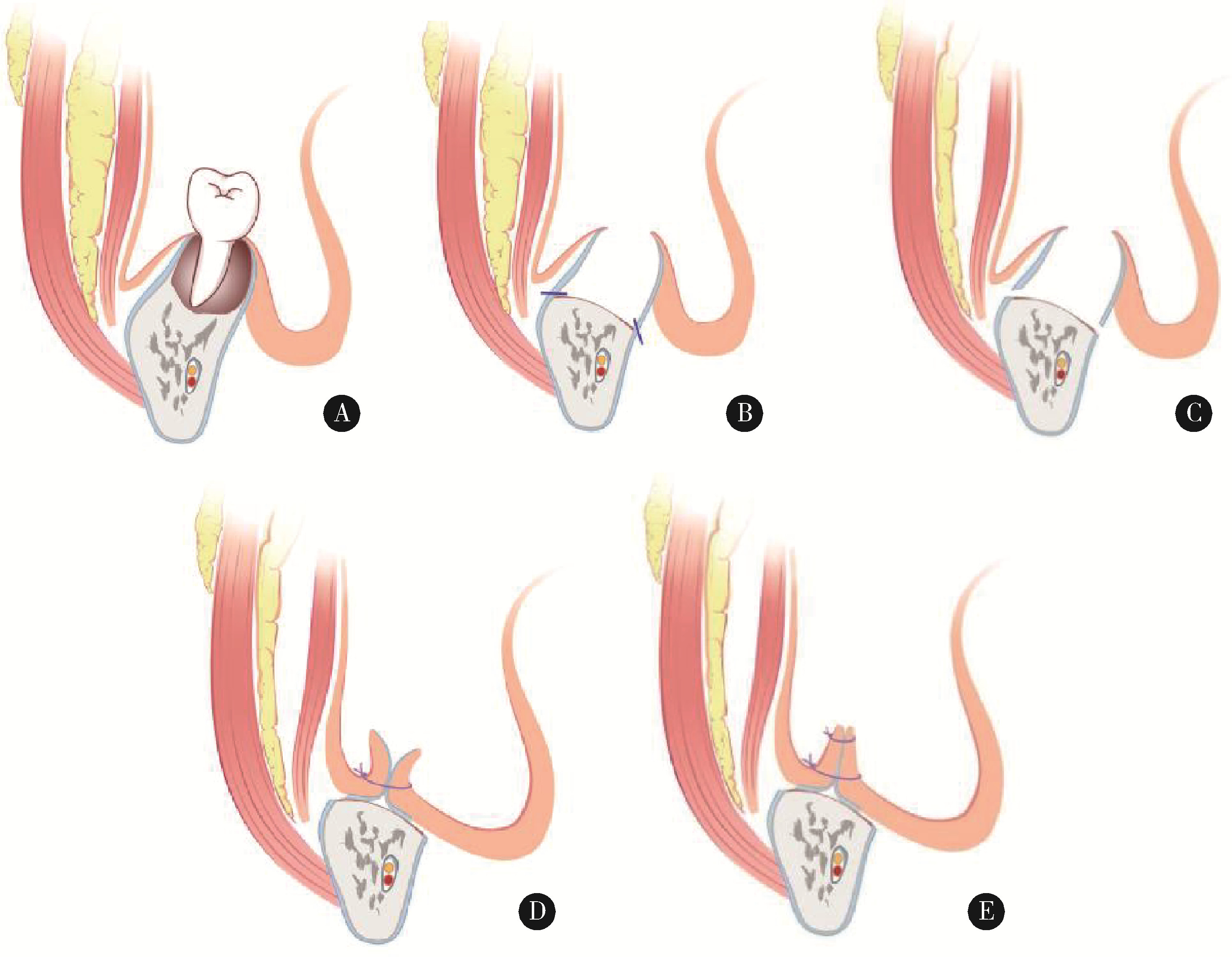
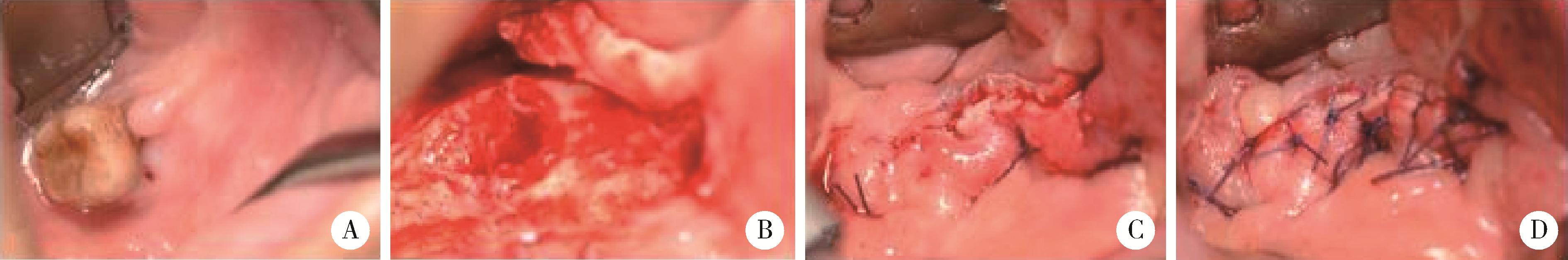
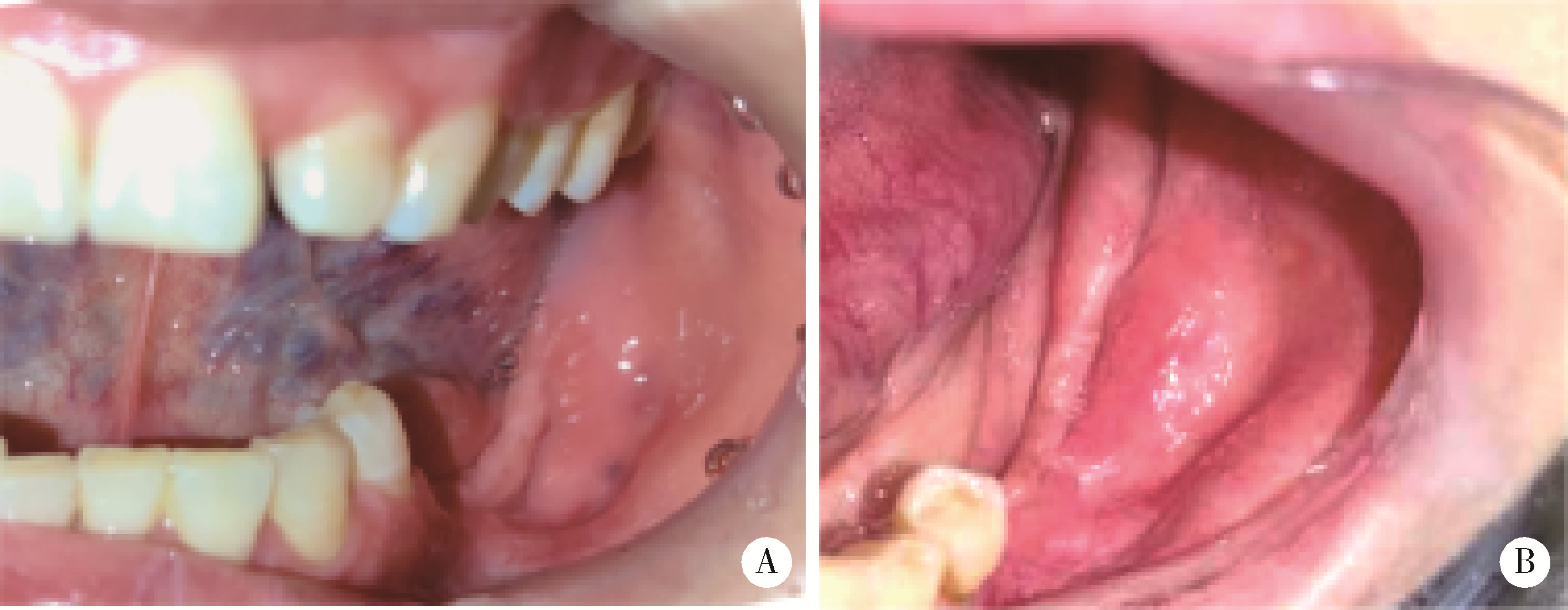
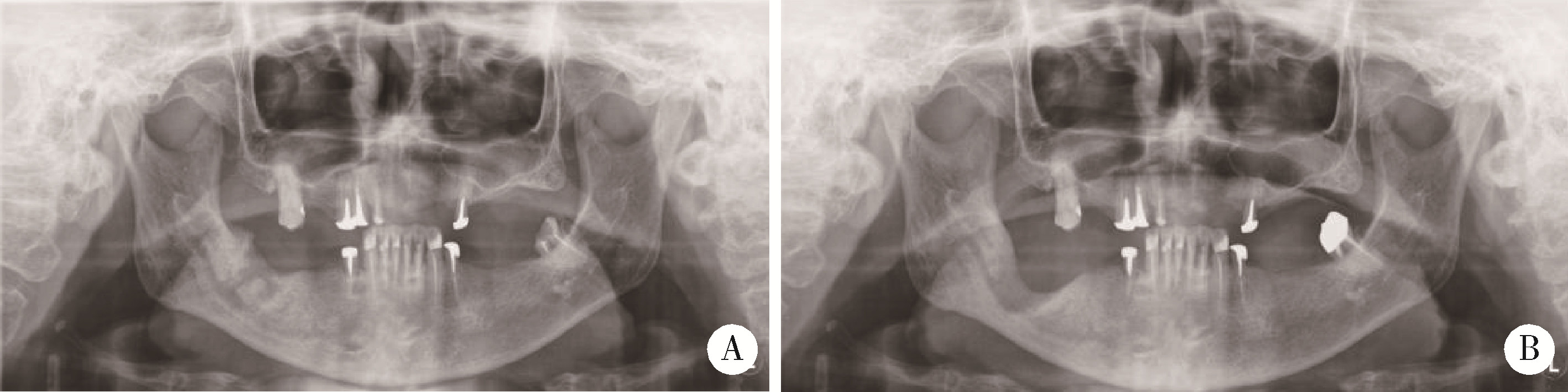
Application of double-layer soft tissue suture closure technique in the surgical treatment of patients with mandible medication-related osteonecrosis of the jaw of early and medium stages
Ying ZHOU,Ning ZHAO,Hongyuan HUANG,Qingxiang LI,Chuanbin GUO,Yuxing GUO*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R782
| 1 |
Marx RE . Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: A growing epidemic[J]. J Oral Maxillofac Surg, 2003, 61 (9): 1115- 1117.
doi: 10.1016/S0278-2391(03)00720-1 |
| 2 |
Ruggiero SL , Dodson TB . American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw: 2014 update[J]. J Oral Maxillofac Surg, 2014, 72 (10): 1938- 1956.
doi: 10.1016/j.joms.2014.04.031 |
| 3 |
郭玉兴, 王佃灿, 王洋, 等. 二膦酸盐药物治疗乳腺癌骨转移发生颌骨坏死的临床特点[J]. 北京大学学报(医学版), 2016, 48 (1): 80- 83.
doi: 10.3969/j.issn.1671-167X.2016.01.014 |
| 4 |
Ruggiero SL , Dodson TB , Aghaloo T , et al. American association of oral and maxillofacial surgeons' position paper on medication-related osteonecrosis of the jaws: 2022 update[J]. J Oral Maxillofac Surg, 2022, 80 (5): 920- 943.
doi: 10.1016/j.joms.2022.02.008 |
| 5 |
Yarom N , Shapiro CL , Peterson DE , et al. Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO clinical practice guideline[J]. J Clin Oncol, 2019, 37 (25): 2270- 2290.
doi: 10.1200/JCO.19.01186 |
| 6 |
Carlson ER . Management of antiresorptive osteonecrosis of the jaws with primary surgical resection[J]. J Oral Maxillofac Surg, 2014, 72 (4): 655- 657.
doi: 10.1016/j.joms.2013.12.007 |
| 7 |
Abu-ld MH , Warnke PH , Gottschalk J , et al. "Bis-phossy jaws"-high and low risk factors for bisphosphonate-induced osteonecrosis of the jaw[J]. J Craniomaxillofac Surg, 2008, 36 (2): 95- 103.
doi: 10.1016/j.jcms.2007.06.008 |
| 8 |
Wilde F , Heufelder M , Winter K , et al. The role of surgical therapy in the management of intravenous bisphosphonates-related osteonecrosis of the jaw[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2011, 111 (2): 153- 163.
doi: 10.1016/j.tripleo.2010.04.015 |
| 9 |
Hayashida S , Soutome S , Yanamoto S , et al. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: A multicenter retrospective study with propensity score matching analysis[J]. J Bone Miner Res, 2017, 32 (10): 2022- 2029.
doi: 10.1002/jbmr.3191 |
| 10 |
Williamson RA . Surgical management of bisphosphonate induced osteonecrosis of the jaws[J]. Int J Oral Maxillofac Surg, 2010, 39 (3): 251- 255.
doi: 10.1016/j.ijom.2009.11.014 |
| 11 |
Lopes RN , Rabelo GD , Rocha AC , et al. Surgical therapy for bisphosphonate-related osteonecrosis of the jaw: Six-year experience of a single institution[J]. J Oral Maxillofac Surg, 2015, 73 (7): 1288- 1295.
doi: 10.1016/j.joms.2015.01.008 |
| 12 | 何悦, 陈珩, 安金刚, 等. 药物相关性颌骨坏死临床诊疗专家共识[J]. 中国口腔颌面外科杂志, 2023, 21 (4): 313- 325. |
| 13 |
Altay MA , Radu A , Pack SE , et al. Medication-related osteonecrosis of the jaw: An institution' s experience[J]. Cranio, 2020, 38 (5): 333- 341.
doi: 10.1080/08869634.2018.1528711 |
| 14 |
安金刚, 吕晓鸣, 贾宽宽, 等. 下颌下腺转位在下颌骨3期药物相关性颌骨坏死手术中的应用[J]. 中华口腔医学杂志, 2021, 56 (5): 441- 446.
doi: 10.3760/cma.j.cn112144-20210203-00058 |
| 15 |
Caldroney S , Ghazali N , Dyalram D , et al. Surgical resection and vascularized bone reconstruction in advanced stage medication-related osteonecrosis of the jaw[J]. Int J Oral Maxillofac Surg, 2017, 46 (7): 871- 876.
doi: 10.1016/j.ijom.2017.01.023 |
| 16 |
Klingelhöffer C , Zeman F , Meier J , et al. Evaluation of surgical outcome and influencing risk factors in patients with medication-related osteonecrosis of the jaws[J]. J Craniomaxillofac Surg, 2016, 44 (10): 1694- 1699.
doi: 10.1016/j.jcms.2016.08.001 |
| 17 |
Mücke T , Koerdt S , Jung M , et al. The role of mylohyoid flap in the treatment of bisphosphonate-related osteonecrosis of the jaws[J]. J Craniomaxillofac Surg, 2016, 44 (4): 369- 373.
doi: 10.1016/j.jcms.2015.12.017 |
| 18 |
Lemound J , Muecke T , Zeller AN , et al. Nasolabial flap improves healing in medication-related osteonecrosis of the jaw[J]. J Oral Maxillofac Surg, 2018, 76 (4): 877- 885.
doi: 10.1016/j.joms.2017.09.021 |
| [1] | Bin CHEN,Chao WU,Bin LIU,Tao YU,Zhen-yu WANG. Prognosis of patients with spinal intramedullary cavernous hemangioma by different treatments [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 652-657. |
| [2] | Yu-xing GUO,Jian-yun ZHANG,Dian-can WANG,Chuan-bin GUO. Analysis of pathological characteristics of medication-related osteonecrosis of the jaw and discussion of clinical treatment strategies based on the pathological analysis results [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1190-1195. |
| [3] | HONG Peng,TIAN Xiao-jun,ZHAO Xiao-yu,YANG Fei-long,LIU Zhuo,LU Min,ZHAO Lei,MA Lu-lin. Bilateral papillary renal cell carcinoma following kidney transplantation: A case report [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 811-813. |
| [4] | Jie YANG,Ran ZHANG,Yu-nan LIU,Dian-can WANG. Plunging ranula presenting as a giant retroauricular mass: A case report [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 193-195. |
| [5] | Rong YANG,Qing-xiang LI,Chi MAO,Xin PENG,Yang WANG,Yu-xing GUO,Chuan-bin GUO. Multimodal image fusion technology for diagnosis and treatment of the skull base-infratemporal tumors [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 53-58. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 205
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 293
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||