Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 811-813. doi: 10.19723/j.issn.1671-167X.2021.04.033
Previous Articles Next Articles
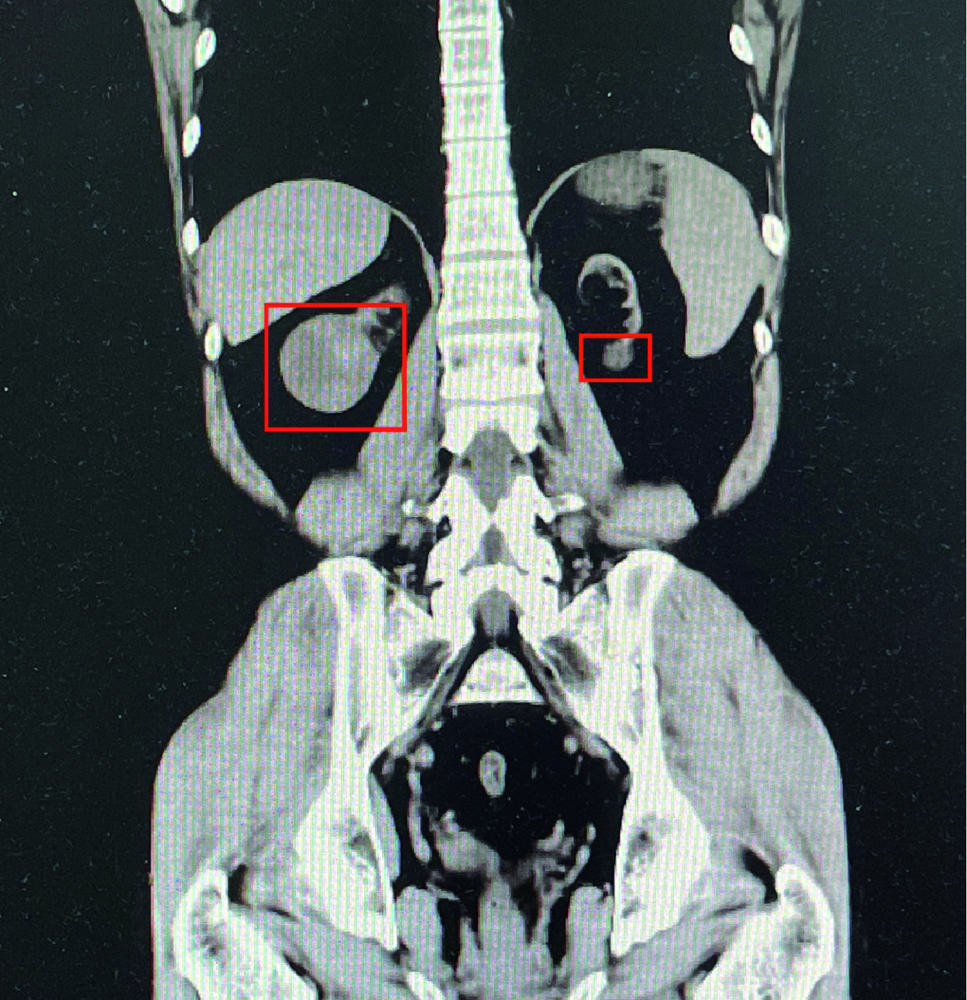
Bilateral papillary renal cell carcinoma following kidney transplantation: A case report
HONG Peng1,TIAN Xiao-jun1,ZHAO Xiao-yu1,YANG Fei-long1,LIU Zhuo1,LU Min2,ZHAO Lei1,Δ( ),MA Lu-lin1,Δ(
),MA Lu-lin1,Δ( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.11
| [1] |
Briggs JD. Causes of death after renal transplantation [J]. Nephrol Dial Transplant, 2001, 16(8):1545-1549.
doi: 10.1093/ndt/16.8.1545 |
| [2] |
Végso G, Tóth M, Hídvégi M, et al. Malignancies after renal transplantation during 33 years at a single center [J]. Pathol Oncol Res, 2007, 13(1):63-69.
doi: 10.1007/BF02893443 |
| [3] |
Kasiske BL, Snyder JJ, Gilbertson DT, et al. Cancer after kidney transplantation in the United States [J]. Am J Transplant, 2004, 4(6):905-913.
doi: 10.1111/ajt.2004.4.issue-6 |
| [4] |
Collett D, Mumford L, Banner NR, et al. Comparison of the incidence of malignancy in recipients of different types of organ: a UK registry audit [J]. Am J Transplant, 2010, 10(8):1889-1896.
doi: 10.1111/j.1600-6143.2010.03181.x pmid: 20659094 |
| [5] |
Engels EA, Pfeiffer RM, Fraumeni JF, et al. Spectrum of cancer risk among US solid organ transplant recipients [J]. JAMA, 2011, 306(17):1891-1901.
doi: 10.1001/jama.2011.1592 pmid: 22045767 |
| [6] | 张健, 马麟麟, 解泽林, 等. 我国肾移植术后新发恶性肿瘤总结分析 [J]. 中华器官移植杂志, 2014, 35(12):705-710. |
| [7] |
Karami S, Yanik EL, Moore LE, et al. Risk of renal cell carcinoma among kidney transplant recipients in the United States [J]. Am J Transplant, 2016, 16(12):3479-3489.
doi: 10.1111/ajt.13862 pmid: 27160653 |
| [8] |
Apel H, Walschburger-Zorn K, Häberle L, et al. De novo malignancies in renal transplant recipients: experience at a single center with 1 882 transplant patients over 39 yr [J]. Clin Transplant, 2013, 27(1):E30-E36.
doi: 10.1111/ctr.2013.27.issue-1 |
| [9] |
Choyke PL. Acquired cystic kidney disease [J]. Eur Radiol, 2000, 10(12):1716-1721.
doi: 10.1007/s003300000601 |
| [10] |
Hoshida Y, Nakanishi H, Shin M, et al. Renal neoplasias in patients receiving dialysis and renal transplantation: clinico-pathological features and p53 gene mutations [J]. Transplantation, 1999, 68(3):385-390.
pmid: 10459542 |
| [11] |
Leveridge M, Musquera M, Evans A, et al. Renal cell carcinoma in the native and allograft kidneys of renal transplant recipients [J]. J Urol, 2011, 186(1):219-223.
doi: 10.1016/j.juro.2011.03.032 pmid: 21575970 |
| [12] |
Ishikawa I, Honda R, Yamada Y, et al. Renal cell carcinoma detected by screening shows better patient survival than that detected following symptoms in dialysis patients [J]. Ther Apher Dial, 2004, 8(6):468-473.
pmid: 15663546 |
| [13] |
Klatte T, Seitz C, Waldert M, et al. Features and outcomes of renal cell carcinoma of native kidneys in renal transplant recipients [J]. BJU Int, 2010, 105(9):1260-1265.
doi: 10.1111/bju.2010.105.issue-9 |
| [14] |
Gigante M, Neuzillet Y, Patard JJ, et al. Renal cell carcinoma (RCC) arising in native kidneys of dialyzed and transplant patients: are they different entities [J]. BJU Int, 2012, 110(11Pt B):E570-E573.
doi: 10.1111/bju.2012.110.issue-11b |
| [15] | Wang B, Gong H, Zhang X, et al. Bilatetal synchronous sporadic renal cell carcinoma: retroperitoneoscopic strategies and intermediate outcomes of 60 patients [J]. PLoS One, 2016, 11(5):e154578. |
| [16] |
Rothman J, Crispen PL, Wong YN, et al. Pathologic concordance of sporadic synchronous bilateral renal mases [J]. Urology, 2008, 72(1):138-142.
doi: 10.1016/j.urology.2008.01.043 pmid: 18336882 |
| [17] |
Becker F, Siemer S, Tzavaras A, et al. Long-term survival in bilateral renal cell carcinoma: a retrospective single-institutional analysis of 101 patients after surgical treatment [J]. Urology, 2008, 72(2):349-353.
doi: 10.1016/j.urology.2008.04.001 pmid: 18485459 |
| [18] |
Lowrance WT, Yee DS, Maschino AC, et al. Developments in the surgical management of sporadic synchronous bilateral renal tumours [J]. BJU Int, 2010, 105(8):1093-1097.
doi: 10.1111/j.1464-410X.2009.08844.x pmid: 19751262 |
| [1] | Handong DING, Qin WANG, Guiyi LIAO, Zongyao HAO. Diagnosis and treatment of gastrointestinal bleeding after kidney transplantation [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 902-907. |
| [2] | Wenbo YANG,Lei YU,Weiyu ZHANG,Tao XU,Qiang WANG. Effect and safety of self-draining ureteral stent with thread in kidney transplant reci-pients [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 656-660. |
| [3] | Ying ZHOU,Ning ZHAO,Hongyuan HUANG,Qingxiang LI,Chuanbin GUO,Yuxing GUO. Application of double-layer soft tissue suture closure technique in the surgical treatment of patients with mandible medication-related osteonecrosis of the jaw of early and medium stages [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 51-56. |
| [4] | Bin CHEN,Chao WU,Bin LIU,Tao YU,Zhen-yu WANG. Prognosis of patients with spinal intramedullary cavernous hemangioma by different treatments [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 652-657. |
| [5] | Er-shu BO,Peng HONG,Yu ZHANG,Shao-hui DENG,Li-yuan GE,Min LU,Nan LI,Lu-lin MA,Shu-dong ZHANG. Clinicopathological features and prognostic analysis of papillary renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 615-620. |
| [6] | Qiu-yu LI,Qin CHENG,Zhi-ling ZHAO,Ni-ni DAI,Lin ZENG,Lan ZHU,Wei GUO,Chao LI,Jun-hong WANG,Shu LI,Qing-gang GE,Ning SHEN. Severe acute respiratory syndrome coronavirus 2 infection in renal transplant recipients: A case report [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 780-784. |
| [7] | Jie YANG,Ran ZHANG,Yu-nan LIU,Dian-can WANG. Plunging ranula presenting as a giant retroauricular mass: A case report [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 193-195. |
| [8] | Kai MA,Xing-ke QU,Qing-quan XU,Liu-lin XIONG,Xiong-jun YE,Li-zhe AN,Wei-nan CHEN,Xiao-bo HUANG. Endoscopic treatment for ureterovesical junction stenosis in patients with kidney transplantation: 13 cases report [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1155-1158. |
| [9] | Rong YANG,Qing-xiang LI,Chi MAO,Xin PENG,Yang WANG,Yu-xing GUO,Chuan-bin GUO. Multimodal image fusion technology for diagnosis and treatment of the skull base-infratemporal tumors [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 53-58. |
| [10] | DING Zhen-shan,QIU Min,XU Zi-cheng,XIAO Ruo-tao,GE Li-yuan,MA Lu-lin. Clinicopathological analysis of patients with papillary renal cell carcinoma complicated by tumor thrombus [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 805-810. |
| [11] | ZHAO Lei, MA Lu-lin, ZHANG Hong-xian, HOU Xiao-fei, LIU Lei, FU Yan, KOU Yun-geng, SONG Yi-meng. Technical improvement in retroperitoneal laparoscopic living donor nephrectomy: report of 193 cases [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 867-871. |
| [12] | ZHANG Hong-xian, ZHAO Lei, MA Lu-lin, HOU Xiao-fei, LIU Lei, DENG Shao-hui. Retroperitoneal laparoscopic nephrectomy with autotransplantation for severe iatrogenic ureteral injury [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 622-626. |
| [13] | LIU Yu-Qing, LU Jian, ZHAO Lei, HOU Xiao-Fei, MA Lu-Lin. Prognostic factors for intravesical recurrence after surgery for upper tract urothelial carcinoma in renal transplant recipients [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 605-610. |
| [14] | LIU Lei, MA Lu-Lin, ZHAO Lei, ZHANG Hong-Xian, HOU Xiao-Fei. Ureteral stricture following renal transplantation: risk factors and surgical management [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 548-551. |
|
||