Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (1): 95-99. doi: 10.19723/j.issn.1671-167X.2022.01.015
Previous Articles Next Articles
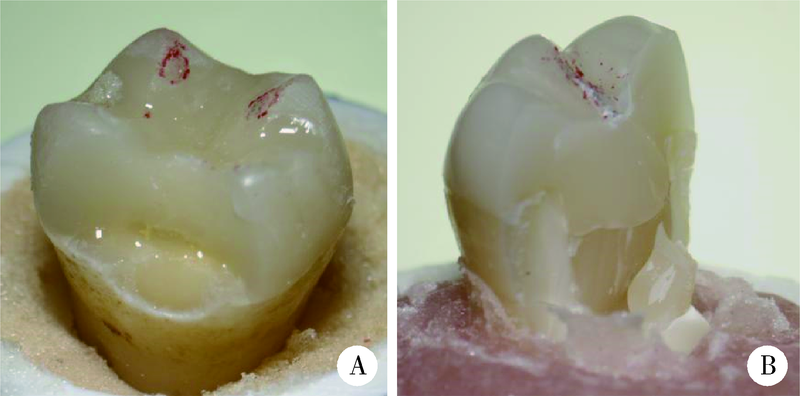
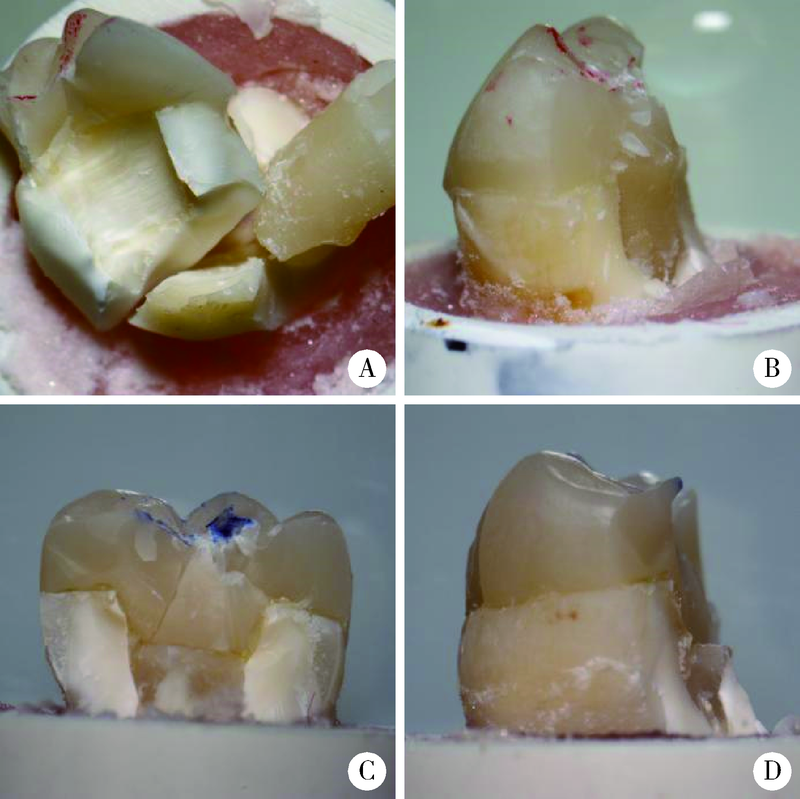
Effects of the resin base and retention depth on fracture resistance of molars restored with nano-ceramic endocrowns
LI Zhi1,XU Yong-xiang2,BAO Xu-dong1,△( ),WANG Xiao-yan1,△(
),WANG Xiao-yan1,△( )
)
- 1. Department of Cariology and Endodontology, Peking University School and Hospital of Stomatology, Beijing 100081, China
2. Department of Dental Materials, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digtal Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R783
| [1] |
Bindl A, Mormann WH. Clinical evaluation of adhesively placed cerec endo-crowns after 2 years: Preliminary results[J]. J Adhes Dent, 1999, 1(3):255-265.
pmid: 11725673 |
| [2] |
Biacchi GR, Mello B, Basting RT. The endocrown: An alternative approach for restoring extensively damaged molars[J]. J Esthet Restor Dent, 2013, 25(6):383-390.
doi: 10.1111/jerd.12065 |
| [3] |
Zarone F, Sorrentino R, Apicella D, et al. Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endocrowns compared to a natural tooth: A 3D static linear finite elements analysis[J]. Dent Mater, 2006, 22(11):1035-1044.
doi: 10.1016/j.dental.2005.11.034 |
| [4] | Gungor MB, Bal BT, Yilmaz H, et al. Fracture strength of CAD/CAM fabricated lithium disilicate and resin nano ceramic restorations used for endodontically treated teeth[J]. Dent Mater J, 2017, 36(2):135-141. |
| [5] |
Ghajghouj O, Faruk ST. Evaluation of fracture resistance and microleakage of endocrowns with different intracoronal depths and restorative materials luted with various resin cements[J]. Materials, 2019, 12(16):2528.
doi: 10.3390/ma12162528 |
| [6] |
Zhu J, Wang D, Rong Q, et al. Effect of central retainer shape and abduction angle during preparation of teeth on dentin and cement layer stress distributions in endocrown-restored mandibular molars[J]. Dent Mater J, 2020, 39(3):464-470.
doi: 10.4012/dmj.2019-050 |
| [7] |
El-Damanhoury HM, Haj-Ali RN, Platt JA. Fracture resistance and microleakage of endocrowns utilizing three CAD-CAM blocks[J]. Oper Dent, 2015, 40(2):201-210.
doi: 10.2341/13-143-L pmid: 25268039 |
| [8] |
Gresnigt MMM, Özcan M, Houten MLAVD, et al. Fracture strength, failure type and Weibull characteristics of lithium disilicate and multiphase resin composite endocrowns under axial and lateral forces[J]. Dent Mater, 2016, 32(5):607-614.
doi: 10.1016/j.dental.2016.01.004 pmid: 26935018 |
| [9] |
Taha D, Spintzyk S, Sabet A, et al. Assessment of marginal adaptation and fracture resistance of endocrown restorations utilizing different machinable blocks subjected to thermomechanical aging[J]. J Esthet Restor Dent, 2018, 30(4):319-328.
doi: 10.1111/jerd.2018.30.issue-4 |
| [10] |
Hayes A, Duvall N, Wajdowicz M, et al. Effect of endocrown pulp chamber extension depth on molar fracture resistance[J]. Oper Dent, 2017, 42(3):327-334.
doi: 10.2341/16-097-L pmid: 28467258 |
| [11] | de Kuijper M, Cune M, Tromp Y, et al. Cyclic loading and load to failure of lithium disilicate endocrowns: Influence of the restoration extension in the pulp chamber and the enamel outline[J/OL]. J Mech Behav Biomed Mater, 2020, 105: 103670 [2021-05-01]. https://doi.org/10.1016/j.jmbbm.2020.103670 . |
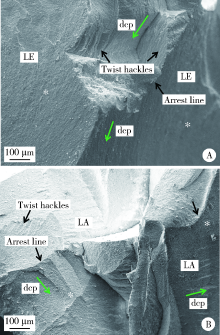
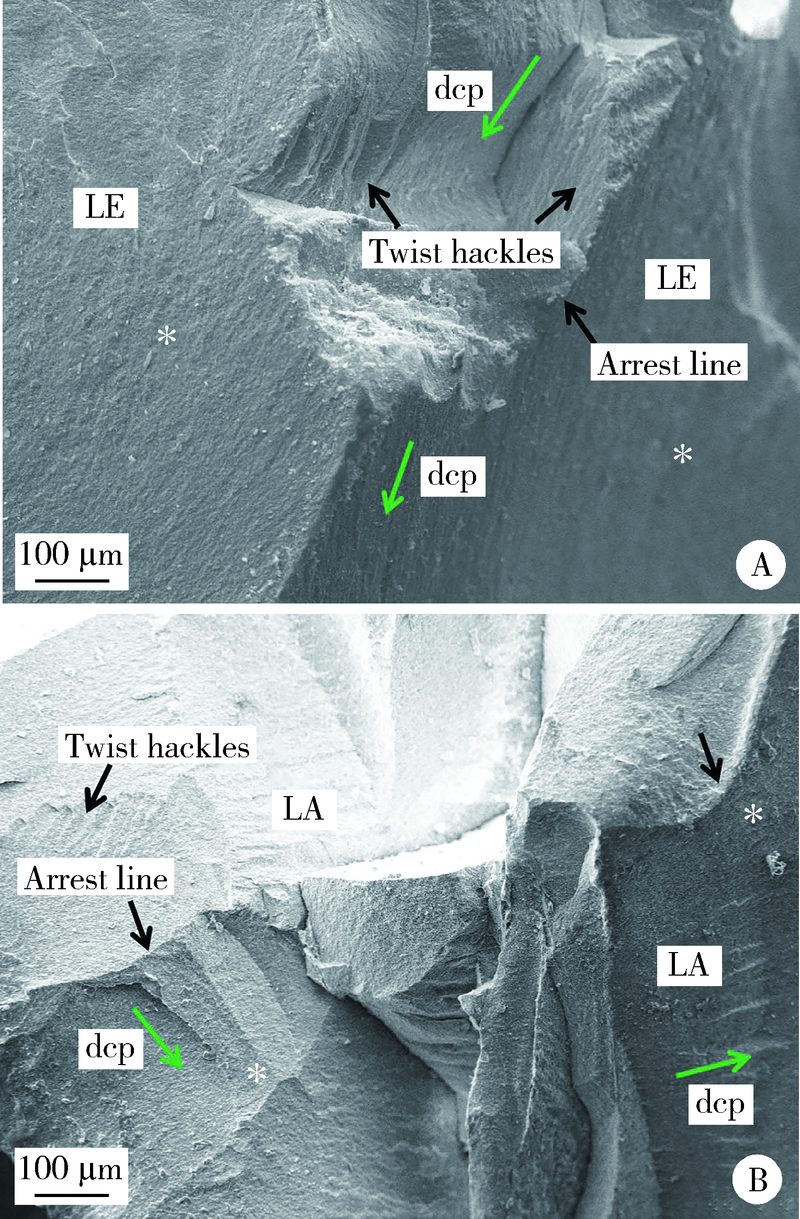
| [12] | 杜倩, 周敏波, 张新平, 等. 前牙全瓷冠饰瓷崩裂断口形貌分析[J]. 中华口腔医学杂志, 2012, 47(4):225-228. |
| [13] | 崔军, 刘学恒, 马练, 等. 渗透陶瓷双层结构的双轴抗弯强度及断裂模式研究[J]. 上海口腔医学, 2010, 19(2):192-195. |
| [14] |
Scherrer S, Quinn J, Quinn G, et al. Failure analysis of ceramic clinical cases using qualitative fractography[J]. Int J Prosthodont, 2006, 19(2):185-192.
pmid: 16602369 |
| [15] |
Saratti C, Rocca G, Durual S, et al. Fractography of clinical failures of indirect resin composite endocrown and overlay restorations[J]. Dent Mater, 2021, 37(6):e341-e359.
doi: 10.1016/j.dental.2021.02.002 pmid: 33627233 |
| [16] |
Zheng Z, He Y, Ruan W, et al. Biomechanical behavior of endocrown restorations with different CAD-CAM materials: A 3D finite element and in vitro analysis[J]. J Prosthet Dent, 2021, 125(6):890-899.
doi: 10.1016/j.prosdent.2020.03.009 |
| [17] |
Tribst JPM, Dal Piva AMD, Madruga CFL, et al. Endocrown restorations: Influence of dental remnant and restorative material on stress distribution[J]. Dent Mater, 2018, 34(10):1466-1473.
doi: 10.1016/j.dental.2018.06.012 |
| [18] | Sun T, Shao B, Liu Z Effects of the lining material, thickness and coverage on residual stress of class Ⅱ molar restorations by multilayer technique[J/OL]. Comput Meth Programs Biomed, 2021, 202: 105995 [2021-05-01]. https://www.sciencedirect.com/science/article/pii/S0169260721000705 . |
| [19] |
Gaintantzopoulou MD, El-Damanhoury HM. Effect of preparation depth on the marginal and internal adaptation of computer-aided design/computer-assisted manufacture endocrowns[J]. Oper Dent, 2016, 41(6):607-616.
pmid: 27379835 |
| [20] |
Dejak B, Młotkowski A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication-FEA[J]. Dent Mater, 2020, 36(7):854-864.
doi: 10.1016/j.dental.2020.04.007 |
| [1] | TIAN Shi-yu, BAI Wei, LIANG Yu-hong. Impact of apical preparation diameter on fracture resistance of mandibular premolar roots [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 92-095. |
|
||