Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (3): 471-478. doi: 10.19723/j.issn.1671-167X.2024.03.014
Previous Articles Next Articles
Influence of telemedicine on the operation of public hospitals in China
Kexin RAN,Yuhan LI,Wen FENG*( )
)
- Department of Health Policy and Management, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- R197
| 1 | 国家卫生部与国家人口计划生育委员会. 卫生计生委关于推进医疗机构远程医疗服务的意见[EB/OL]. [2014-08-21]. https://www.gov.cn/gongbao/content/2014/content_2792664.htm. |
| 2 | 国家卫生计生委办公厅. 国家卫生计生委办公厅关于印发远程医疗信息系统建设技术指南的通知[EB/OL]. [2014-12-10]. http://www.nhc.gov.cn/mohwsbwstjxxzx/s8555/201501/120c912de1c4474c95b345d001271368.shtml. |
| 3 |
Huang EY , Knight S , Guetter CR , et al.Telemedicine and telementoring in the surgical specialties: A narrative review[J].Am J Surg,2019,218(4):760-766.
doi: 10.1016/j.amjsurg.2019.07.018 |
| 4 |
Nesemann JM , Munoz M , Talero SL , et al.Telemedicine for screening eye disease in the remote Peruvian Amazon: Proof-of-concept[J].Trans R Soc Trop Med Hyg,2022,116(6):589-591.
doi: 10.1093/trstmh/trab175 |
| 5 |
占玉芬, 陈文军, 李艳.我院跨国式远程医疗的实践与探索[J].中华医院管理杂志,2019,35(3):213-215.
doi: 10.3760/cma.j.issn.1000-6672.2019.03.010 |
| 6 |
Lu W , Hou H , Ma R , et al.Influencing factors of patient satisfaction in teleconsultation: A cross-sectional study[J].Technol Forecast Soc,2021,168,120775.
doi: 10.1016/j.techfore.2021.120775 |
| 7 |
Yanicelli LM , Vegetti M , Goy CB , et al.SiTe iC: A telemoni-toring system for heart failure patients[J].Int J Med Inform,2020,141,104204.
doi: 10.1016/j.ijmedinf.2020.104204 |
| 8 | 汪晓珊. 喀什地区远程医疗的社会经济效益分析研究[D]. 新疆: 石河子大学, 2014. |
| 9 |
Chauhan A , Jakhar SK , Jabbour CJC .Implications for sustainable healthcare operations in embracing telemedicine services during a pandemic[J].Technol Forecast Soc,2022,176,121462.
doi: 10.1016/j.techfore.2021.121462 |
| 10 |
Kim DS , Chu H , Min BK , et al.Telemedicine center of Korean Medicine for treating patients with COVID-19: A retrospective analysis[J].Integr Med Res,2020,9(3):100492.
doi: 10.1016/j.imr.2020.100492 |
| 11 |
Gudi N , Konapur R , John O , et al.Telemedicine supported strengthening of primary care in WHO South East Asia region: Lessons from the COVID-19 pandemic experiences[J].BMJ Innovations,2021,7(3):580-585.
doi: 10.1136/bmjinnov-2021-000699 |
| 12 |
Lilly CM , Motzkus C , Rincon T , et al.ICU telemedicine program financial outcomes[J].Chest,2017,151(2):286-297.
doi: 10.1016/j.chest.2016.11.029 |
| 13 | 路阳, 汪晓珊, 邹小广, 等.新疆地区远程会诊系统应用的经济效益案例分析[J].中国卫生经济,2015,34(4):71-73. |
| 14 | 国家卫生计生委办公厅. 国家卫生计生委办公厅关于印发医院信息化建设应用技术指引(2017年版)的通知[EB/OL]. [2017-12-13]. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=aed4d45c 8f75467fb208b4707cceb0ad. |
| 15 |
Kim SA , Park WS , Chun TJ , et al.Association of the implementation of PACS with hospital revenue[J].J Digit Imaging,2002,15(4):247-253.
doi: 10.1007/s10278-002-0025-4 |
| 16 |
Lee J , Choi JY .Texas hospitals with higher health information technology expenditures have higher revenue: A longitudinal data analysis using a generalized estimating equation model[J].BMC Health Serv Res,2016,16,117.
doi: 10.1186/s12913-016-1367-9 |
| 17 |
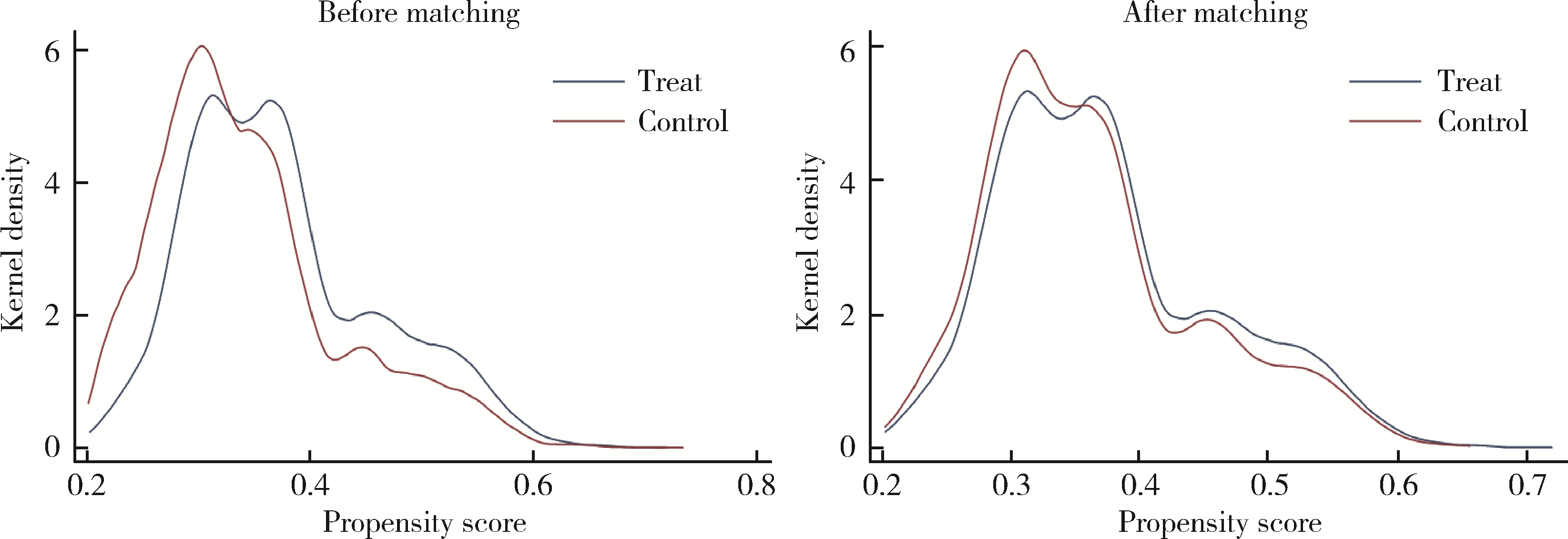
Rosenbaum PR , Rubin DB .The central role of the propensity score in observational studies for causal effects[J].Biometrika,1983,70(1):41-55.
doi: 10.1093/biomet/70.1.41 |
| 18 |
管德坤, 孙自学.新时期我国远程医疗发展驱动、阻碍因素及建设重点分析[J].中国医院,2020,24(4):56-58.
doi: 10.3969/j.issn.1671-9174.2020.04.005 |
| 19 | 陈强.高级计量经济学及Stata应用[M].北京: 高等教育出版社,2014. |
| 20 |
Zhao M , Hamadi H , Rob HD , et al.The relationship between health information technology laboratory tracking systems and hospital financial performance and quality[J].Hosp Top,2019,97(3):99-106.
doi: 10.1080/00185868.2019.1623735 |
| 21 |
Zhao M , Hamadi H , Xu J , et al.Telehealth and hospital perfor-mance: Does it matter?[J].J Telemed Telecare,2022,28(5):360-370.
doi: 10.1177/1357633X20932440 |
| 22 | 罗益佳, 周典, 徐慧, 等.基于史密斯模型的远程医疗政策执行分析[J].南京医科大学学报(社会科学版),2020,20(3):210-214. |
| 23 | 胡文秀.远程医疗对提升卫生服务水平的促进作用及对策建议[J].学习与实践,2018,(1):80-84. |
| 24 | 焦建鹏, 徐静, 王炳坤, 等.医联体远程医疗协作网建设与思考——以河南省人民医院为例[J].中国农村卫生事业管理,2022,42(7):511-514. |
| 25 | 孙倩倩, 周守君.我国远程医疗的现状、问题及发展对策[J].南京医科大学学报(社会科学版),2022,22(1):25-30. |
| 26 |
陈凤, 吴杨.远程医疗服务模式下提升医联体内基层卫生服务能力的实践[J].重庆医学,2020,49(10):1706-1708.
doi: 10.3969/j.issn.1671-8348.2020.10.036 |
| 27 | 李艳, 邹卿云, 尹传东, 等.农村边远地区远程医疗的社会效益和经济效益分析[J].中国卫生经济,2009,28(12):53-54. |
| 28 | 王淼, 晏雪鸣, 徐剑云, 等.跨区域专科远程医疗协同体系的建立与探索[J].现代医院,2022,22(6):915-918. |
| 29 | Omboni S .Telemedicine during the COVID-19 in Italy: A missed opportunity?[J].Telemed J E Health,2020,26(8):973-975. |
| 30 | Khodadad-Saryazdi A .Exploring the telemedicine implementation challenges through the process innovation approach: A case study research in the French healthcare sector[J].Technovation,2021,107,102273. |
| [1] | JING Ri-ze, ZHANG Hu-yang, XU Ting-ting, ZHANG Lu-yu, FANG Hai. Study on the efficiency of tertiary public hospitals and its influencing factors in Beijing [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 408-415. |
|
||