Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (6): 1144-1151. doi: 10.19723/j.issn.1671-167X.2021.06.023
Previous Articles Next Articles
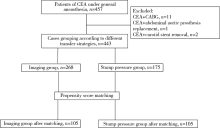
Effect of different shunt strategies on cerebral infarction after carotid endarterectomy
BAI Peng1,WANG Tao2,ZHOU Yang1,TAO Li-yuan3,LI Gang1,LI Zheng-qian1,GUO Xiang-yang1,△( )
)
- 1. Department of Anesthesiology, Peking University Third Hospital, Beijing 100191, China
2. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
3. Clinical Epidemiology Research Center, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R651.12
| [1] |
Petty GW, Brown RD Jr, Whisnant JP, et al. Ischemic stroke subtypes: A population-based study of incidence and risk factors[J]. Stroke, 1999, 30(12):2513-2516.
pmid: 10582970 |
| [2] |
Kret MR, Young B, Moneta GL, et al. Results of routine shunting and patch closure during carotid endarterectomy[J]. Am J Surg, 2012, 203(5):613-617.
doi: 10.1016/j.amjsurg.2011.12.005 |
| [3] |
Aburahma AF, Mousa AY, Stone PA. Shunting during carotid endarterectomy[J]. J Vasc Surg, 2011, 54(5):1502-1510.
doi: 10.1016/j.jvs.2011.06.020 pmid: 21906905 |
| [4] |
Samson RH, Cline JL, Showalter DP, et al. Contralateral carotid artery occlusion is not a contraindication to carotid endarterectomy even if shunts are not routinely used[J]. J Vasc Surg, 2013, 58(4):935-940.
doi: 10.1016/j.jvs.2013.04.011 |
| [5] |
Aburahma AF, Stone PA, Hass SM, et al. Prospective rando-mized trial of routine versus selective shunting in carotid endarterectomy based on stump pressure[J]. J Vasc Surg, 2010, 51(5):1133-1138.
doi: 10.1016/j.jvs.2009.12.046 pmid: 20347544 |
| [6] | Rerkasem K, Rothwell PM. Routine or selective carotid artery shunting for carotid endarterectomy and different methods of monitoring in selective shunting[J]. Stroke, 2010, 41(1):e53-e54 |
| [7] |
Lichtman JH, Jones MR, Leifheit EC, et al. Carotid endarterectomy and carotid artery stenting in the US medicare population, 1999-2014[J]. JAMA, 2017, 318(11):1035-1046.
doi: 10.1001/jama.2017.12882 pmid: 28975306 |
| [8] |
Wiske C, Arhuidese I, Malas M, et al. Comparing the efficacy of shunting approaches and cerebral monitoring during carotid endarterectomy using a national database[J]. J Vasc Surg, 2018, 68(2):416-425.
doi: S0741-5214(18)30035-1 pmid: 29571621 |
| [9] |
Banga PV, Varga A, Csobay-Novák C, et al. Incomplete circle of Willis is associated with a higher incidence of neurologic events during carotid eversion endarterectomy without shunting[J]. J Vasc Surg, 2018, 68(6):1764-1771.
doi: 10.1016/j.jvs.2018.03.429 |
| [10] | 中华医学会外科学分会血管外科学组. 颈动脉狭窄诊治指南[J]. 中国血管外科杂志, 2017, 9(3):169-175. |
| [11] |
Kolkert JLP, Groenwold RHH, Leijdekkers VJ, et al. Cost-effectiveness of two decision strategies for shunt use during carotid endarterectomy[J]. World J Surg, 2017, 41(11):2959-2967.
doi: 10.1007/s00268-017-4085-5 pmid: 28623598 |
| [12] | 李攀峰, 王兵, 崔文军, 等. 对侧颈动脉狭窄程度对颈动脉内膜剥脱术中转流管应用的影响[J]. 实用医学杂志, 2015, 31(10):1639-1641. |
| [13] |
Huibers A, Calvet D, Kennedy F, et al. Mechanism of procedural stroke following carotid endarterectomy or carotid artery stenting within the International Carotid Stenting Study (ICSS) randomised trial[J]. Eur J Vasc Endovasc Surg, 2015, 50(3):281-288.
doi: 10.1016/j.ejvs.2015.05.017 |
| [14] |
Spagnoli LG, Mauriello A, Sangiorgi G, et al. Extracranial thrombotically active carotid plaque as a risk factor for ischemic stroke[J]. JAMA, 2004, 292(15):1845-1852.
pmid: 15494582 |
| [15] | 刁永鹏, 刘昌伟, 宋小军, 等. 颈动脉内膜剥脱术治疗老年颈动脉狭窄患者的危险因素分析[J]. 中华普通外科杂志, 2014, 29(6):448-451. |
| [1] | Chang-feng FAN,Ya-ping HUANG,Xia LI,Yun CHEN,Zhen LI,Shu-dong QIAO. Posterior inferior cerebellar artery infarction with episodic postural diplopia as the initial symptom: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 762-765. |
| [2] | Ying LIU,Ran HUO,Hui-min XU,Zheng WANG,Tao WANG,Hui-shu YUAN. Correlations between plaque characteristics and cerebral blood flow in patients with moderate to severe carotid stenosis using magnetic resonance vessel wall imaging [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 646-651. |
| [3] | Zi-chang JIA,Xuan LI,Mei ZHENG,Jing-yuan LUAN,Chang-ming WANG,Jin-tao HAN. Hybrid treatment for symptomatic long-segment chronic internal carotid artery occlusion without stump [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 177-180. |
| [4] | Hai-yan ZHAO,Dong-sheng FAN,Jin-tao HAN. Management of severe internal carotid stenosis with unruptured intracranial aneurysm [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 829-834. |
| [5] | LI Jin-yong, SUN Hong-liang, YE Zhi-dong, FAN Xue-qiang, LIU Peng. Carotid plaque composition and volume evaluated by multi-detector computed tomography angiography [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 833-839. |
| [6] | HAN Jin-tao, LI Xuan, HE Qing-yuan, ZHAO Hai-yan, YE Shan, DONG Guo-xiang, LUAN Jing-yuan, WANG Chang-ming. Endovascular treatment in cerebral artery tandem lesions [J]. Journal of Peking University(Health Sciences), 2016, 48(1): 149-153. |
|
||