Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 1082-1087. doi: 10.19723/j.issn.1671-167X.2023.06.020
Previous Articles Next Articles
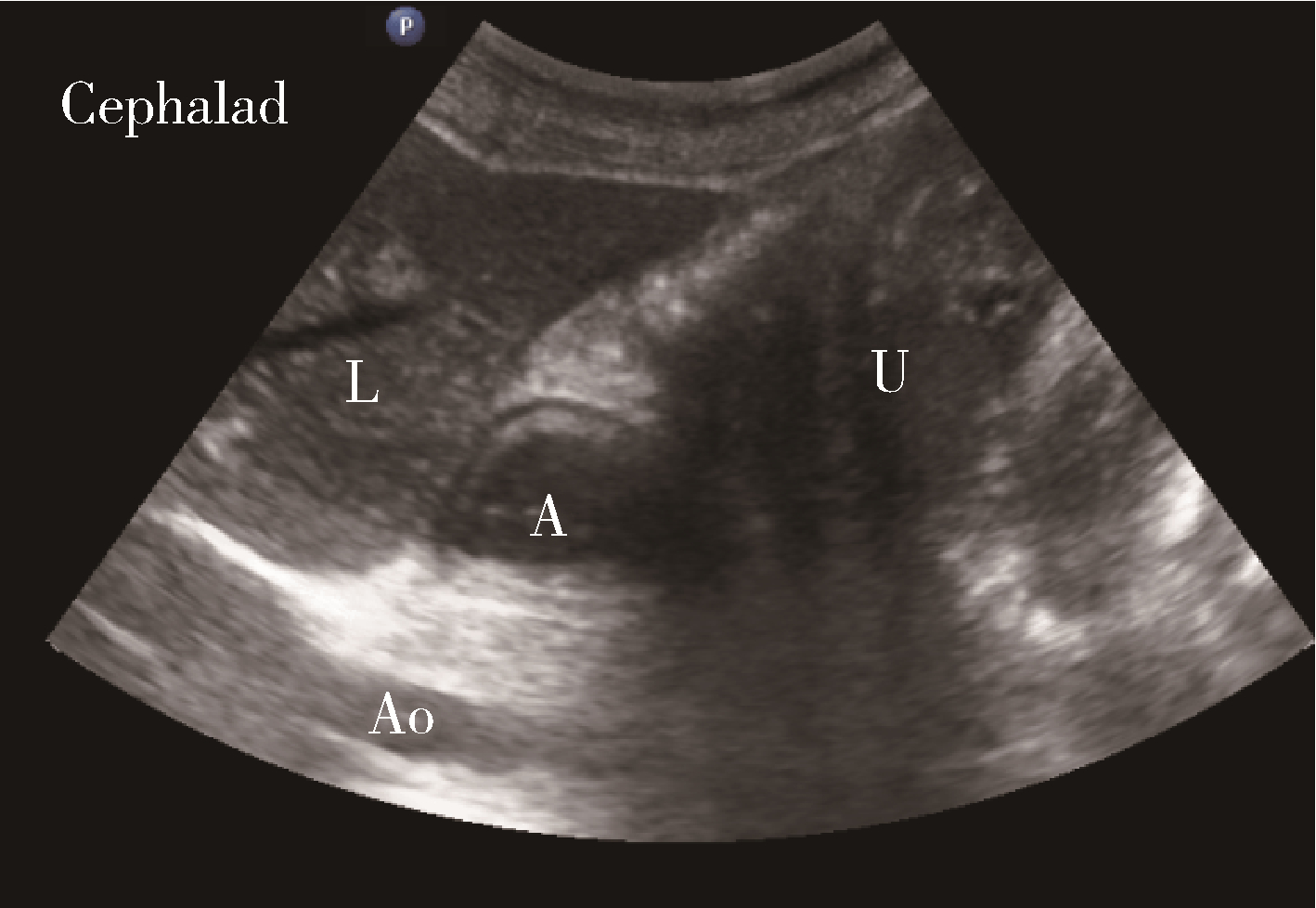
Evaluation of gastric emptying after drinking carbohydrates before cesarean section by gastric ultrasonography
Yue WEI1,Lan YAO1,Xi LU1,Jun WANG1,Li LIN2,Kun-peng LIU1,*( )
)
- 1. Department of Anesthesiology, Peking University International Hospital, Beijing 102206, China
2. Department of Obstetrics and Gynecology, Peking University International Hospital, Beijing 102206, China
CLC Number:
- R614.3
| 1 |
Nygren J , Thacker J , Carli F , et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendation[J]. Clin Nutr, 2012, 31 (6): 801- 816.
doi: 10.1016/j.clnu.2012.08.012 |
| 2 |
Bouvet L , Mazoit JX , Chassard D , et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume[J]. Anesthesiology, 2011, 114 (5): 1086- 1092.
doi: 10.1097/ALN.0b013e31820dee48 |
| 3 |
Perlas A , Davis L , Khan M , et al. Gastric sonography in the fasted surgical patient: A prospective descriptive study[J]. Anesth Analg, 2011, 113 (1): 93- 97.
doi: 10.1213/ANE.0b013e31821b98c0 |
| 4 |
Perlas A , Mitsakakis N , Liu L , et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination[J]. Anesth Analg, 2013, 116 (2): 357- 363.
doi: 10.1213/ANE.0b013e318274fc19 |
| 5 |
van de Putte P , Perlas A . Ultrasound assessment of gastric content and volume[J]. Br J Anaesth, 2014, 113 (1): 12- 22.
doi: 10.1093/bja/aeu151 |
| 6 |
Gola W , Domagala M , Cugowski A . Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period[J]. Anaesthesiol Intensive Ther, 2018, 50 (4): 297- 302.
doi: 10.5603/AIT.a2018.0029 |
| 7 |
Apfelbaum JL , Hawkins JL , Agarkar M , et al. Practice guidelines for obstetric anesthesia: An updated report by the American Society of Anesthesiologists task force on obstetric anesthesia and the Society for Obstetric Anesthesia and Perinatology[J]. Anesthesiology, 2016, 124 (2): 270- 300.
doi: 10.1097/ALN.0000000000000935 |
| 8 | 刘平, 干卓坤. 超声评估胃容量及胃内容物性质的研究[J]. 中国医学影像学杂志, 2016, 24 (4): 285- 288. |
| 9 |
Kruisselbrink R , Arzola C , Endersby R , et al. Intra- and interrater reliability of ultrasound assessment of gastric volume[J]. Anesthesiology, 2014, 121 (1): 46- 51.
doi: 10.1097/ALN.0000000000000193 |
| 10 |
Perlas A , Chan VW , Lupu CM , et al. Ultrasound assessment of gastric content and volume[J]. Anesthesiology, 2009, 111 (1): 82- 89.
doi: 10.1097/ALN.0b013e3181a97250 |
| 11 |
Arzola C , Cubillos J , Perlas A , et al. Interrater reliability of qua-litative ultrasound assessment of gastric content in the third trimester of pregnancy[J]. Br J Anaesth, 2014, 113 (6): 1018- 1023.
doi: 10.1093/bja/aeu257 |
| 12 |
Arzola C , Perlas A , Siddiqui NT , et al. Bedside gastric ultrasonography in term pregnant women before elective cesarean deli-very: A prospective cohort study[J]. Anesth Analg, 2015, 121 (3): 752- 758.
doi: 10.1213/ANE.0000000000000818 |
| 13 |
Roukhomovsky M , Zieleskiewicz L , Diaz A , et al. Ultrasound examination of the antrum to predict gastric content volume in the third trimester of pregnancy as assessed by MRI: A prospective cohort study[J]. Eur J Anaesthesiol, 2018, 35 (5): 379- 389.
doi: 10.1097/EJA.0000000000000749 |
| 14 |
Popivanov P , Irwin R , Walsh M , et al. Gastric emptying of carbohydrate drinks in term parturients before elective caesarean deli-very: An observational study[J]. Int J Obstet Anesth, 2020, 41, 29- 34.
doi: 10.1016/j.ijoa.2019.07.010 |
| 15 | 王以瑞, 符新春, 郑芝, 等. 口服碳水化合物溶液的容量与足月产妇胃排空时间的关系[J]. 中华医学杂志, 2018, 98 (26): 2083- 2087. |
| 16 |
Amaral CK , Benevides ML , Benevides MM , et al. Ultrasound assessment of gastric antrum in term pregnant women before elective cesarean section[J]. Rev Bras Anestesio, 2019, 69 (3): 266- 271.
doi: 10.1016/j.bjan.2019.03.001 |
| 17 |
Hakak S , McCaul CL , Crowley L . Ultrasonographic evaluation of gastric contents in term pregnant women fasted for six hours[J]. Int J Obstet Anesth, 2018, 34, 15- 20.
doi: 10.1016/j.ijoa.2018.01.004 |
| 18 |
Shiraishi T , Kurosaki D , Nakamura M , et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: A magnetic resonance imaging-based analysis[J]. Anesth Analg, 2017, 124 (4): 1174- 1178.
doi: 10.1213/ANE.0000000000001886 |
| [1] | Yue WEI,Xi LU,Jing ZHANG,Kun-peng LIU,Yong-jun WANG,Lan YAO. Effect of preoperative carbohydrates intake on the gastric volume and the risk of reflux aspiration in patients positioning in trendelenburg undergoing gynecological laparoscopic procedures [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 893-898. |
| [2] | Yun-fei XING,Chun-yi LIU,Wen-ying MENG,Jie ZHANG,Ming-yuan JIAO,Lei JIN,Lei JIN. Relationship between micronutrients supplementation during periconceptional period and serum concentration of vitamin E in the 1st trimester of gestational period [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 434-442. |
| [3] | SUN Ying, JIN Lei. Blood manganese levels among pregnant women and the associated factors in three counties of northern China [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 463-468. |
|
||