Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (4): 667-672. doi: 10.19723/j.issn.1671-167X.2024.04.020
Previous Articles Next Articles
Functional and oncologic outcomes of partial nephrectomy for cystic renal cell carcinoma: A single-center retrospective study
Fan SHU,Yichang HAO,Zhanyi ZHANG,Shaohui DENG,Hongxian ZHANG,Lei LIU,Guoliang WANG,Xiaojun TIAN,Lei ZHAO,Lulin MA,Shudong ZHANG*( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.11
| 1 |
Bray F , Ferlay J , Soerjomataram I , et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68 (6): 394- 424.
doi: 10.3322/caac.21492 |
| 2 | Kuroda N , Ohe C , Mikami S , et al. Multilocular cystic renal cell carcinoma with focus on clinical and pathobiological aspects[J]. Histol Histopathol, 2012, 27 (8): 969- 974. |
| 3 |
Wahal SP , Mardi K . Multilocular cystic renal cell carcinoma: A rare entity with review of literature[J]. J Lab Physicians, 2014, 6 (1): 50- 52.
doi: 10.4103/0974-2727.129093 |
| 4 |
Upfill-Brown A , Lenis AT , Faiena I , et al. Treatment utilization and overall survival in patients receiving radical nephroureterectomy versus endoscopic management for upper tract urothelial carcinoma: Evaluation of updated treatment guidelines[J]. World J Urol, 2019, 37 (6): 1157- 1164.
doi: 10.1007/s00345-018-2506-1 |
| 5 |
Yagisawa T , Takagi T , Yoshida K , et al. Surgical outcomes of robot-assisted laparoscopic partial nephrectomy for cystic renal cell carcinoma[J]. J Robot Surg, 2022, 16 (3): 649- 654.
doi: 10.1007/s11701-021-01292-7 |
| 6 |
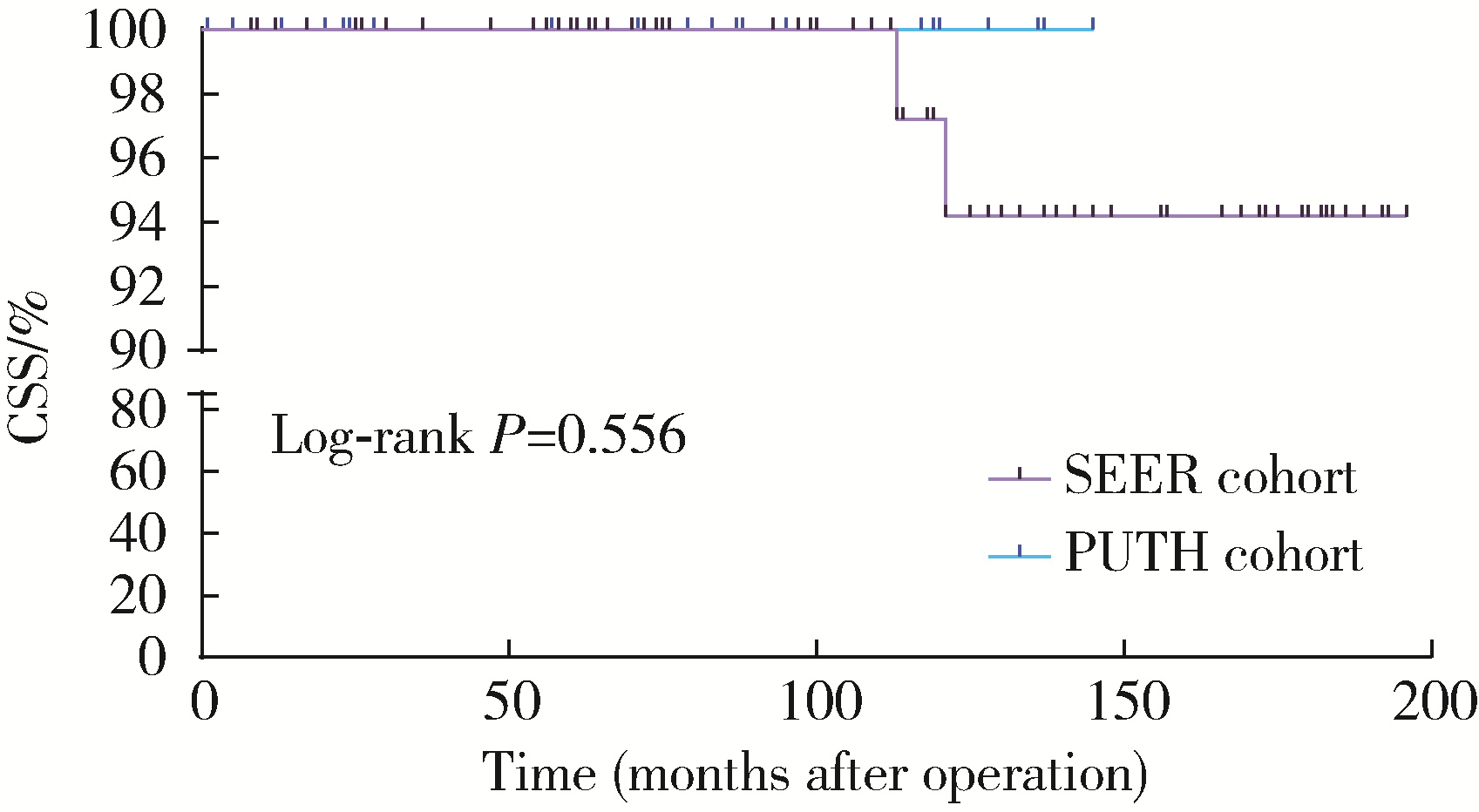
Lin W , Yang Z , Yan L , et al. Comparison of partial nephrectomy and radical nephrectomy for cystic renal cell carcinoma: A SEER-based and retrospective study[J]. Sci Rep, 2023, 13 (1): 8052.
doi: 10.1038/s41598-023-34950-x |
| 7 |
Wang L , Deng JY , Li KP , et al. Perioperative and oncological outcomes of robot-assisted laparoscopic partial nephrectomy for cystic and solid renal masses: Evidence from controlled trials[J]. Asian J Surg, 2024, 47 (1): 16- 24.
doi: 10.1016/j.asjsur.2023.08.048 |
| 8 |
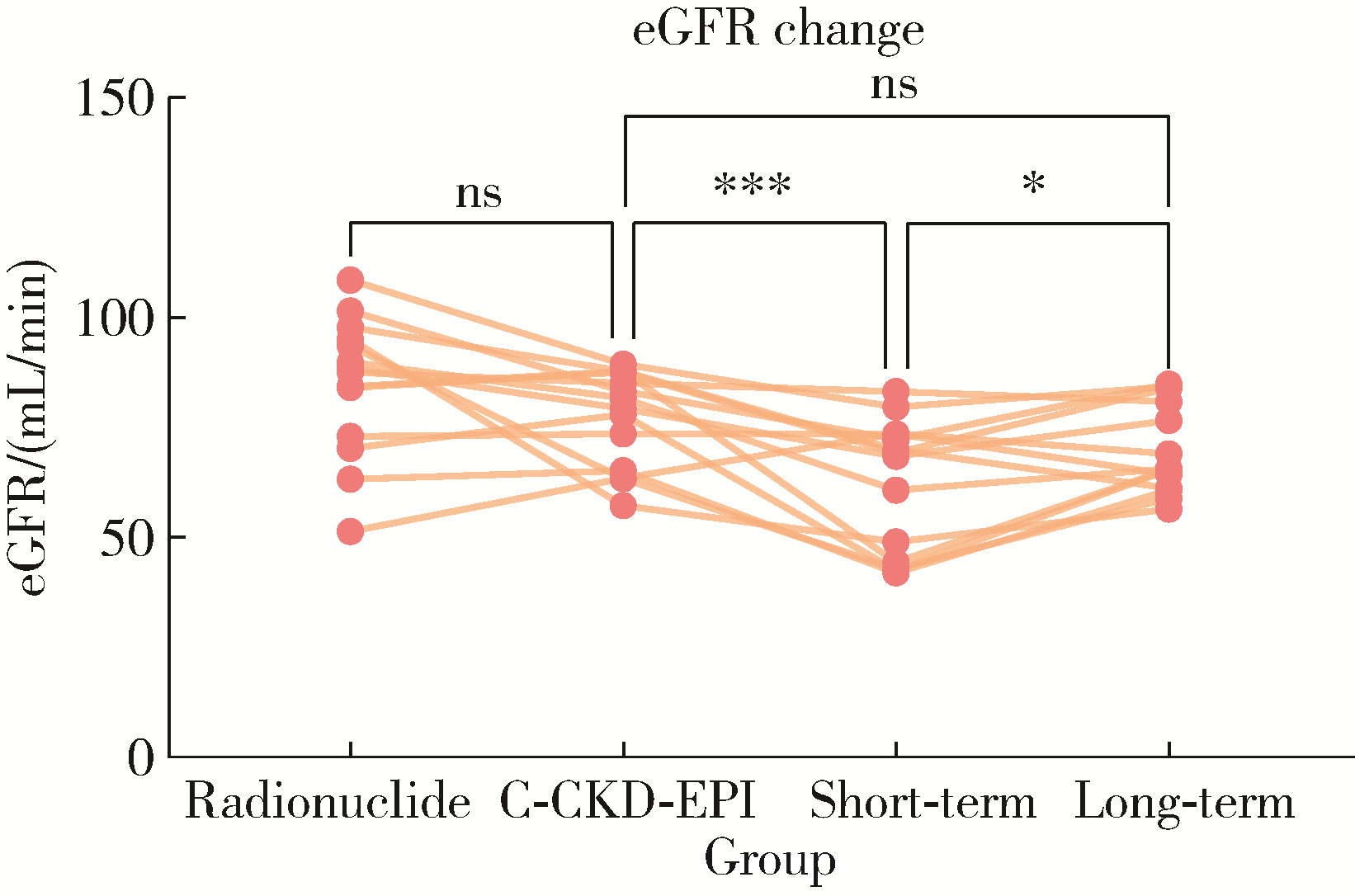
Yang M , Zou Y , Lu T , et al. Revised Equations to estimate glomerular filtration rate from serum creatinine and cystatin C in China[J]. Kidney Blood Press Res, 2019, 44 (4): 553- 564.
doi: 10.1159/000500460 |
| 9 |
Hartman DS , Davis CJ, Jr , Johns T , et al. Cystic renal cell carcinoma[J]. Urology, 1986, 28 (2): 145- 153.
doi: 10.1016/0090-4295(86)90109-3 |
| 10 |
Bielsa O , Lloreta J , Gelabert-Mas A . Cystic renal cell carcinoma: pathological features, survival and implications for treatment[J]. Br J Urol, 1998, 82 (1): 16- 20.
doi: 10.1046/j.1464-410x.1998.00689.x |
| 11 |
Corica FA , Iczkowski KA , Cheng L , et al. Cystic renal cell carcinoma is cured by resection: A study of 24 cases with long-term followup[J]. J Urol, 1999, 161 (2): 408- 411.
doi: 10.1016/S0022-5347(01)61903-7 |
| 12 |
Koga S , Nishikido M , Hayashi T , et al. Outcome of surgery in cystic renal cell carcinoma[J]. Urology, 2000, 56 (1): 67- 70.
doi: 10.1016/S0090-4295(00)00540-9 |
| 13 | Winters BR , Gore JL , Holt SK , et al. Cystic renal cell carcinoma carries an excellent prognosis regardless of tumor size[J]. Urol Oncol, 2015, 33 (12): 505. e509- 505. e513. |
| 14 | Tretiakova M , Mehta V , Kocherginsky M , et al. Predominantly cystic clear cell renal cell carcinoma and multilocular cystic renal neoplasm of low malignant potential form a low-grade spectrum[J]. Virchows Arch, 2018, 473 (1): 85- 93. |
| 15 | Lee J , Song C , Lee D , et al. Differential contribution of the factors determining long-term renal function after partial nephrectomy over time[J]. Urol Oncol, 2021, 39 (3): 196. e115- 196. e120. |
| 16 |
Park JJ , Jeong BC , Kim CK , et al. Postoperative outcome of cystic renal cell carcinoma defined on preoperative imaging: A retrospective study[J]. J Urol, 2017, 197 (4): 991- 997.
doi: 10.1016/j.juro.2016.10.055 |
| 17 |
Zhang S , Qin Z , Bi H , et al. A "3S+f" nephrometry score system to predict the clinical outcomes of laparoscopic nephron-sparing surgery[J]. Front Oncol, 2022, 12, 922082.
doi: 10.3389/fonc.2022.922082 |
| [1] | Kewei CHEN,Zhuo LIU,Shaohui DENG,Fan ZHANG,Jianfei YE,Guoliang WANG,Shudong ZHANG. Clinical diagnosis and treatment of renal angiomyolipoma with inferior vena cava tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 617-623. |
| [2] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [3] | QIU Min,WANG Lu,DENG Shao-hui,TA Peng-fei,GUO Wei,LU Jian,LIU Cheng,MA Lu-lin. Primary application of Gerota’s fascia suspension device in retroperitoneal laparoscopic partial nephrectomy [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 789-792. |
| [4] | Shu-dong ZHANG,Peng HONG,Bin-shuai WANG,Shao-hui DENG,Fan ZHANG,Li-yuan TAO,Cai-guang CAO,Zhen-hua HU,Lu-lin MA. Usefulness of the indocyanine green fluorescence imaging technique in laparoscopic partial nephrectomy [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 657-662. |
| [5] | LIANG Yin-hua, ZU Xiong-bing, CHENG Xu, LIU Long-fei. Retroperitoneal laparoscopic with renal pedicle rotation for partial nephrectomy of ventro-renal tumor [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 608-612. |
| [6] | LIU Meng, FU Zhan-Li, DI Li-Juan, ZHANG Jian-Hua, FAN Yan, ZHANG Xu-Chu, WANG Rong-Fu. Efficiency evaluation of diuretic renography in the operative or conservative treatments of unilateral ureteropelvic junction obstruction patients [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 638-642. |
|
||