1 资料与方法
1.1 病例选择
1.2 数据收集与随访
1.3 统计学分析
2 结果
表1 患者手术方式与围手术期数据Table 1 Surgical methods and perioperative data of the patients |
| Operation | Operation time/min | Estimated blood loss/mL | Postoperative hospitalization days/d | Follow up/months |
| Total | 186.0 (21.0-372.0) | 30.0 (0-1 000.0) | 6.0 (2.0-18.0) | 14.2 (6.1-107.1) |
| Ureteroureterostomy | 145.0 (129.0-155.0) | 20.0 (5.0-30.0) | 5.0 (3.0-6.0) | 12.1 (6.6-45.7) |
| Pyeloplasty | 176.0 (113.0-198.0) | 20.0 (20.0-20.0) | 7.0 (4.0-7.0) | 19.8 (12.8-20.6) |
| Ureteral reimplantation | 122.5 (92.0-219.0) | 20.0 (0-70.0) | 4.0 (3.0-6.0) | 8.9 (6.3-22.3) |
| Appendiceal graft ureteroplasty | 168.0 (131.0-276.0) | 30.0 (10.0-100.0) | 6.0 (4.0-10.0) | 20.2 (6.8-35.6) |
| Oral graft ureteroplasty | 170.0 (130.0-270.0) | 30.0 (10.0-200.0) | 5.0 (4.0-8.0) | 10.0 (6.1-37.7) |
| Ileal ureter | 230.0 (170.0-372.0) | 50.0 (10.0-1 000.0) | 9.5 (5.0-18.0) | 19.6 (6.4-107.1) |
| Balloon dilation | 70.0 (21.0-82.0) | 0 (0-0) | 2.0 (2.0-3.0) | 56.5 (13.7-92.1) |
Data were M(min-max). |
表2 修复策略及临床结局Table 2 Reconstructive strategies and clinical outcomes |
| Operation | n | Location | Length of stricture/cm, M(min-max) | |||||||||
| Upper | Middle | Lower | Long/Multiple | |||||||||
| Ureteroureterostomy | 5 | 4 | 1 | 0 | 0 | 2.0 (1.0-3.0) | ||||||
| Pyeloplasty | 3 | 3 | 0 | 0 | 0 | 1.0 (1.0-3.0) | ||||||
| Ureteral reimplantation | 10 | 0 | 0 | 10 | 0 | 5.0 (4.0-10.0) | ||||||
| Appendiceal graft ureteroplasty | 9 | 8 | 1 | 0 | 0 | 4.0 (2.5-5.5) | ||||||
| Oral graft ureteroplasty | 15 | 13 | 2 | 0 | 0 | 3.0 (2.0-5.0) | ||||||
| Ileal ureter replacement | 25 | 7 | 4 | 3 | 11 | 19.0 (4.5-30.0) | ||||||
| Balloon dilation | 4 | 1 | 1 | 2 | 0 | 0.75 (0.5-1.0) | ||||||
| Operation | Symptoms* | Degree of hydronephrosis | Renal function | Success rate/% | ||||||||
| Complete relief | Partial relief | Cured | Improved | Stable | Aggravated | Improved | Stable | Aggravated | ||||
| Ureteroureterostomy | 2 | 1 | 4 | 1 | 0 | 0 | 2 | 3 | 0 | 100 | ||
| Pyeloplasty | 2 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | 0 | 100 | ||
| Ureteral reimplantation | 2 | 2 | 2 | 4 | 4 | 0 | 4 | 6 | 0 | 100 | ||
| Appendiceal graft ureteroplasty | 4 | 4 | 4 | 3 | 2 | 0 | 4 | 5 | 0 | 100 | ||
| Oral graft ureteroplasty | 8 | 2 | 7 | 4 | 4 | 0 | 8 | 7 | 0 | 100 | ||
| Ileal ureter replacement | 10 | 6 | 9 | 7 | 8 | 1 | 11 | 13 | 1 | 96 | ||
| Balloon dilation | 2 | 2 | 1 | 1 | 1 | 1 | 2 | 2 | 0 | 75 | ||
*Only patients presented with symptoms before surgery were included. |
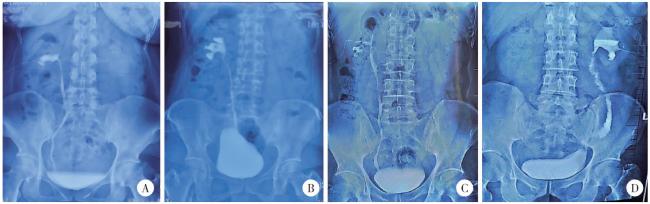
图2 结石相关输尿管狭窄的不同重建手术策略Figure 2 Different surgical strategies for stone related ureteral stricture A, ureteroureterostomy; B, ureteral reimplantation (psoas hitch); C, autologous mucosal graft ureteroplasty; D, ileal ureter replacement. |
表3 患者术后并发症及治疗Table 3 Postoperative complications and management |
| Grade | Complications | Operation and incidence rate | Management |
| Ⅰ | Urine leakage at the proximal anastomotic site | Ileal ureter (1/25) | Prolong the DJ stent drainage time |
| Obstruction | Ileal ureter (1/25) | Prolong the DJ stent drainage time | |
| Urinary tract infection | Ileal ureter (2/25) Appendiceal graft (1/9) | Oral antibiotic | |
| Ⅱ | Incomplete intestinal obstruction | Ileal ureter (1/25) | Nothing by mouth, gastrointestinal decompression, parenteral nutrition |
| Ⅲb | Incisional hernia | Ileal ureter (1/25) | Herniorrhaphy |
| Calculi | Ileal ureter (1/25) | Lithohtripsy |