1 资料与方法
1.1 患者一般资料
表1 患者基线特征Table 1 Patient baseline characteristics |
| Items | Case 1 | Case 2 |
| Age/years | 72 | 54 |
| Gender | Female | Female |
| Affected side | Bilateral | Bilateral |
| Etiology | Radiotherapy for cervical high-grade squamous intraepithelial lesion | Radiotherapy after cervical cancer surgery |
Symptom manifestation | Low back pain, intermittent fever, urinary frequency and urgency | Low back pain, intermittent fever, urinary frequency and urgency |
| Length of ureteral stricture/cm | Left 10.4, right 8.7 | Left 10.6, right 11.7 |
| Preoperative hydronephrosis degree | Bilateral moderate to severe hydronephrosis | Bilateral moderate to severe hydronephrosis |
| Past surgical history | Open pyelolithotomy on the left side | Hysterectomy and bilateral adnexectomy |
| Preoperative management | Nephrostomy for 2 months | Nephrostomy for 2 months |
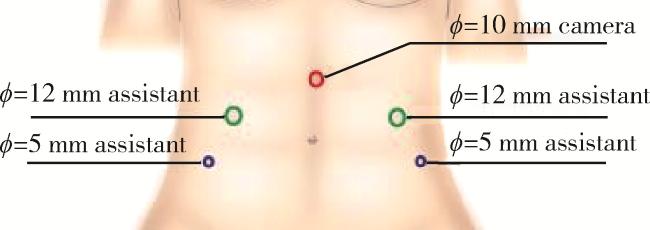
1.2 手术方法
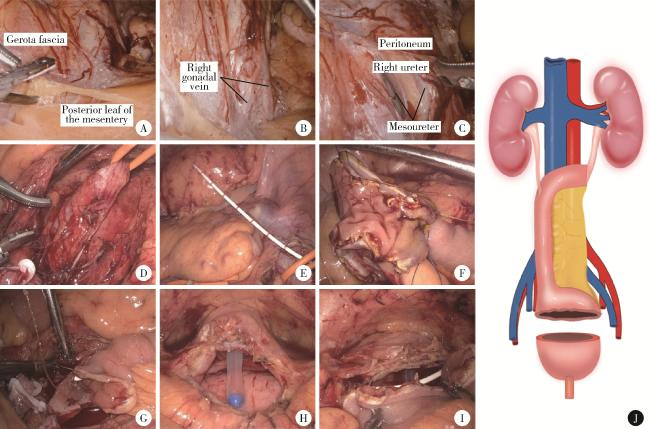
图2 完全3D腹腔镜回肠代双侧输尿管并膀胱扩大术手术步骤及模式图Figure 2 Surgical and schematic diagrams of total 3D laparoscopic ileal replacement of bilateral ureters with cystoplasty A, dissection into the plane between the retromesenteric leaf and prerenal fascia; B, incising the continuation of renal fascia followed by dissection and ligation of right gonadal vein; C, dissection of right ureter along the extra-mesenteric plane; D, mobilization and tagging of right ureter; E, performing precise measurement for ileal segment required for ureteral replacement; F, intracorporeal suturing of ileal bladder flap; G, clamp-free end-to-end anastomosis between right ureter and ileal conduit; H, transverse incision (4 cm) on bladder dome; I, continuous suture of ileal bladder flap to native bladder; J, schematic diagram of surgical procedure. |
1.3 术后处理
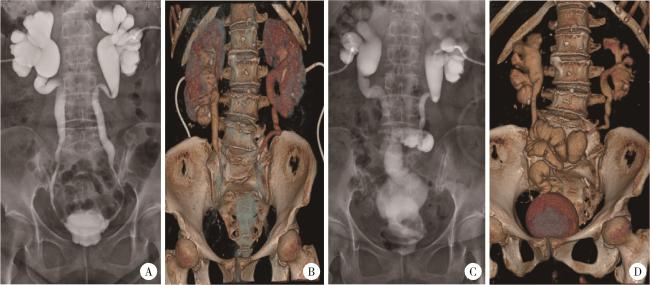
图3 术前及术后影像学检查Figure 3 Preoperative and postoperative imaging examinations A and B, preoperative nephrostogram and 3D CT reconstruction demonstrated bilateral long-segment ureteral strictures, contracted bladder with reduced capacity, and rigid, thickened bladder walls; C and D, two-month follow-up 3D CT reconstruction revealed good peristalsis in the ileal ureteral substitute segment. The bladder exhibited symmetrical morphology with smooth wall contour. |
1.4 随访计划
2 结果
表2 患者围手术期及术后随访情况Table 2 Perioperative and postoperative follow-up conditions of patients |
| Items | Case 1 | Case 2 |
| Surgical method | Total 3D laparoscopy | Total 3D laparoscopy |
| Surgical duration/min | 420 | 355 |
| Intraoperative blood loss/mL | 50 | 50 |
| Length of bowel resection/cm | 40 | 38 |
| Perioperative complications | None | None |
| Time to flatus passage after surgery/d | 4.5 | 3 |
| Hospital stay duration/d | 10 | 8 |
| Residual urine volume (preoperative/2 months postoperative)/mL | 45/50 | 60/55 |
| Bladder capacity (preoperative/2 months postoperative)/mL | 90/230 | 130/250 |
| 24-hour urination frequency (preoperative/2 months postoperative) | (16-18)/(9-10) | (12-14)/(8-9) |
| Nocturia frequency (preoperative/2 months postoperative) | (3-5)/(1-2) | (2-3)/(1-2) |
| Clean intermittent self-catheterization | No | No |
| Base excess/(mmol/L) | ||
| Preoperative | +0.8 | -1.2 |
| 2 months postoperative | -1.8 | -2.6 |
| 6 months postoperative | -2.2 | -2.4 |
| Serum creatinine/(μmol/L) | ||
| Preoperative | 118.11 | 179.63 |
| 1 day postoperative | 131.77 | 180.41 |
| 2 months postoperative | 125.31 | 100.03 |
| 6 months postoperative | 136.83 | 110.67 |
| 8 months postoperative | 138.40 | 107.89 |
| 10 months postoperative | 126.65 | - |
| Follow-up duration/months | 10 | 8 |