Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (3): 414-421. doi: 10.19723/j.issn.1671-167X.2019.03.007
Previous Articles Next Articles
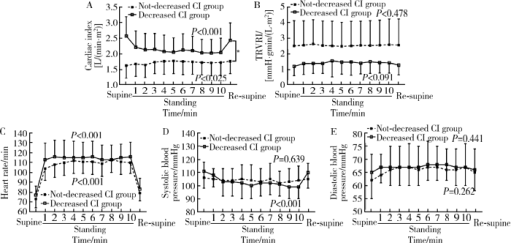
Hemodynamic changes in standing-up test of children and adolescents with postural tachycardia syndrome
Chun-yan TAO1,Hong-xia LI1,Xue-ying LI2,Chao-shu TANG3,Hong-fang JIN1,Jun-bao DU1△( )
)
- 1. Department of Pediatrics, Peking University First Hospital, Beijing 100034, China
2. Department of Statistics, Peking University First Hospital, Beijing 100034, China
3. Department of Physiology and Pathophysiology, Peking University School of Basic Medical Sciences, Beijing 100191, China
4. Key Laboratory of Molecular Cardiovascular Science, the Ministry of Education, Beijing 100191, China
CLC Number:
- R725.4
| [1] |
Goodman BP . Evaluation of postural tachycardia syndrome (POTS)[J]. Auton Neurosci, 2018,215:12-19.
doi: 10.1016/j.autneu.2018.04.004 |
| [2] |
Johnson JN, Mack KJ, Kuntz NL , et al. Postural orthostatic tachycardia syndrome: a clinical review[J]. Pediatr Neurol, 2010,42(2):77-85.
doi: 10.1016/j.pediatrneurol.2009.07.002 |
| [3] | Stewart JM, Pianosi P, Shaban MA , et al. Postural hyperventilation as a cause of postural tachycardia syndrome: increased systemic vascular resistance and decreased cardiac output when upright in all postural tachycardia syndrome variants[J]. J Am Heart Assoc, 2018,7(13):e008854. |
| [4] |
Li H, Han Z, Chen S, et al. Total peripheral vascular resistance, cardiac output ,plasma C-type natriuretic peptide level in children with postural tachycardia syndrome[J]. J Pediatr, 2015, 166(6): 1385- 1389. e1-2.
doi: 10.1016/j.jpeds.2015.03.032 |
| [5] |
Zheng X, Chen Y, Du J . Recent advances in the understanding of the mechanisms underlying postural tachycardia syndrome in children: practical implications for treatment[J]. Cardiol Young, 2017,27(3):413-417.
doi: 10.1017/S1047951116002559 |
| [6] |
Medow MS, Stewart JM . The postural tachycardia syndrome[J]. Cardiol Rev, 2007,15(2):67-75.
doi: 10.1097/01.crd.0000233768.68421.40 |
| [7] | 中华医学会儿科学分会心血管学组, 《中华儿科杂志》编辑委员会, 北京医学会儿科学分会心血管学组, 等. 2016儿童晕厥诊断指南(2016年修订版)[J]. 中华儿科杂志, 2016,54(4):246-250. |
| [8] | 中华医学会儿科学分会心血管学组, 《中华儿科杂志》编辑委员会. 儿童晕厥诊断指南[J]. 中华儿科杂志, 2009,47(2):99-101. |
| [9] |
Garland EM, Celedonio JE, Raj SR . Postural tachycardia syndrome: beyond orthostatic intolerance[J]. Curr Neurol Neurosci Rep, 2015,15(9):60.
doi: 10.1007/s11910-015-0583-8 |
| [10] |
Stewart JM, Medow MS, Glover JL , et al. Persistent splanchnic hyperemia during upright tilt in postural tachycardia syndrome[J]. Am J Physiol Heart Circ Physiol, 2006,290(2):H665-H673.
doi: 10.1152/ajpheart.00784.2005 |
| [11] |
Fu Q, Vangundy TB, Galbreath MM , et al. Cardiac origins of the postural orthostatic tachycardia syndrome[J]. J Am Coll Cardiol, 2010,55(25):2858-2868.
doi: 10.1016/j.jacc.2010.02.043 |
| [12] | Jacob G, Biaggioni I, Mosqueda-Garcia R , et al. Relation of blood volume and blood pressure in orthostatic intolerance[J]. Am J Med Sci, 1998,315(2):95-100. |
| [13] |
Farquhar WB, Taylor JA, Darling SE , et al. Abnormal baroreflex responses in patients with idiopathic orthostatic intolerance[J]. Circulation, 2000,102(25):3086-3091.
doi: 10.1161/01.CIR.102.25.3086 |
| [14] |
Zhang Q, Liao Y, Tang C , et al. Twenty-four-hour urinary sodium excretion and postural orthostatic tachycardia syndrome[J]. J Pediatr, 2012,161(2):281-284.
doi: 10.1016/j.jpeds.2012.01.054 |
| [15] | 蔺婧, 刘平, 王瑜丽 , 等. 儿童体位性心动过速综合征治疗随访的单中心研究[J]. 中华实用儿科临床杂志, 2015,30(13):983-987. |
| [16] | 蔺婧, 刘平, 王瑜丽 , 等. 直立试验心率变化预测口服补液盐治疗体位性心动过速综合征的效果[J]. 中华儿科杂志, 2015,53(1):25-29. |
| [17] |
Li H, Wang Y, Liu P , et al. Body mass index (BMI) is associated with the therapeutic response to oral rehydration solution in children with postural tachycardia syndrome[J]. Pediatr Cardiol, 2016,37(7):1313-1318.
doi: 10.1007/s00246-016-1436-1 |
| [18] |
Lu W, Yan H, Wu S , et al. Hemocytometric measures predict the efficacy of oral rehydration for children with postural tachycardia syndrome[J]. J Pediatr, 2017,187:220-224.
doi: 10.1016/j.jpeds.2017.04.034 |
| [19] |
Raj SR, Robertson D . Blood volume perturbations in the postural tachycardia syndrome[J]. Am J Med Sci, 2007,334(1):57-60.
doi: 10.1097/MAJ.0b013e318063c6c0 |
| [20] | Karataş Z, Alp H, Sap F , et al. Usability of QTc dispersion for the prediction of orthostatic intolerance syndromes[J]. Eur J Paediatr Neurol, 2012,16(5):467-474. |
| [21] |
Wang Y, Zhang C, Chen S , et al. Frequency domain indices of heart rate variability are useful for differentiating vasovagal syncope and postural tachycardia syndrome in children[J]. J Pediatr, 2019,207:59-63.
doi: 10.1016/j.jpeds.2018.11.054 |
| [22] |
Lin J, Jin H, Du J . Assessment of therapeutic biomarkers in the treatment of children with postural tachycardia syndrome and vasovagal syncope[J]. Cardiol Young, 2014,24(5):792-796.
doi: 10.1017/S1047951114000316 |
| [23] |
Altun B, Arici M . Salt and blood pressure: time to challenge[J]. Cardiology, 2006,105(1):9-16.
doi: 10.1159/000088265 |
| [24] |
Hart EC, Joyner MJ, Wallin BG , et al. Sex, ageing and resting blood pressure: gaining insights from the integrated balance of neural and haemodynamic factors[J]. J Physiol, 2012,590(9):2069-2079.
doi: 10.1113/jphysiol.2011.224642 |
| [25] | Bevan JA . Control of peripheral vascular resistance: evidence based on the in vitro study of resistance arteries[J]. Clin Invest Med, 1987,10(6):568-572. |
| [1] | Xiuwen FEI,Si LIU,Bo WANG,Aimei DONG. Clinical characteristics and treatment in adults and children with histiocytic necroti-zing lymphadenitis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 533-540. |
| [2] | Xiao-jin YAN,Yun-fei LIU,Ning MA,Jia-jia DANG,Jing-shu ZHANG,Pan-liang ZHONG,Pei-jin HU,Yi SONG,Jun MA. Assessment of prevalence of malnutrition among Chinese primary and secondary school students and analysis of policy effect during the period of the Program for the Development of Chinese Children 2011-2020 [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 593-599. |
| [3] | Xiao-yi MI,Shan-shan HOU,Zi-yuan FU,Mo ZHOU,Xin-xuan LI,Zhao-xue MENG,Hua-fang JIANG,Hong Zhou. Reliability and validity of the Chinese version of adverse childhood experiences international questionnaire in parents of preschool children [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 408-414. |
| [4] | Meng-jie CUI,Qi MA,Man-man CHEN,Tao MA,Xin-xin WANG,Jie-yu LIU,Yi ZHANG,Li CHEN,Jia-nuo JIANG,Wen YUAN,Tong-jun GUO,Yan-hui DONG,Jun MA,Yi XING. Association between different growth patterns and metabolic syndrome in children and adolescents aged 7 to 17 years [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 415-420. |
| [5] | Jia-jia DANG,Shan CAI,Pan-liang ZHONG,Ya-qi WANG,Yun-fei LIU,Di SHI,Zi-yue CHEN,Yi-hang ZHANG,Pei-jin HU,Jing LI,Jun MA,Yi SONG. Association of outdoor artificial light at night exposure with overweight and obesity among children and adolescents aged 9 to 18 years in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 421-428. |
| [6] | Tao MA,Yan-hui LI,Man-man CHEN,Ying MA,Di GAO,Li CHEN,Qi MA,Yi ZHANG,Jie-yu LIU,Xin-xin WANG,Yan-hui DONG,Jun MA. Associations between early onset of puberty and obesity types in children: Based on both the cross-sectional study and cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 961-970. |
| [7] | Ya-xi CUI,Jun-bao DU,Qing-you ZHANG,Ying LIAO,Ping LIU,Yu-li WANG,Jian-guang QI,Hui YAN,Wen-rui XU,Xue-qin LIU,Yan SUN,Chu-fan SUN,Chun-yu ZHANG,Yong-hong CHEN,Hong-fang JIN. A 10-year retrospective analysis of spectrums and treatment options of orthostatic intolerance and sitting intolerance in children [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 954-960. |
| [8] | YAN Hui,PANG Lu,LI Xue-ying,YANG Wen-shuang,JIANG Shi-ju,LIU Ping,YAN Cun-ling. Incidence and cause of abnormal cholesterol in children aged 2-18 years in a single center [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 217-221. |
| [9] | CHEN Man-man,YANG Zhao-geng,SU Bin-bin,LI Yan-hui,GAO Di,MA Ying,MA Tao,DONG Yan-hui,MA Jun. Analysis on the law of height growth spurt in adolescence of children and adolescents in Zhongshan City [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 506-510. |
| [10] | LU Jin-hui, QIAN Jun, LIU He, ZHU Jun-xia. Clinical study on autologus platelet-rich fibrin aided revascularization of immature permanent teeth [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 672-679. |
| [11] | WU Peng-hui, XIE Yao, ZHAO Wei-hong, HUA Ying, SUN Qing, LI Shuo, WU Ye, LU Xin-tian. Clinical characteristics analysis of children with reversible posterior leukoen-cephalopathy syndrome during the treatment of hematological tumor [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 662-665. |
| [12] | CHEN Tian-qi, DONG Bin, ZHANG Wen-jing, GAO Di-si, DONG Yan-hui, MA Jun, MA Ying-hua. Association between speed and endurance performance with sleep duration in children and adolescents [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 429-435. |
| [13] | DONG Yan-hui, SONG Yi, DONG Bin, ZOU Zhi-yong, WANG Zheng-he, YANG Zhao-geng, WANG Xi-jie, LI Yan-hui, MA Jun. Association between the blood pressure status and nutritional status among Chinese students aged 7-18 years in 2014: based on the national blood pressure reference for Chinese children and adolescents [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 422-428. |
| [14] | WANG Nan, ZHAO Yu-ming. Retrospective study of dental treatment under general anesthesia of 62 disabled children and adolescents [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 293-299. |
| [15] | XU Wen-rui, LIAO Ying, JIN Hong-fang, ZHANG Qing-you, TANG Chao-shu, DU Jun-bao. Progress in diagnosis and management of syncope in children [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 756-759. |
|
||