Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (3): 548-555. doi: 10.19723/j.issn.1671-167X.2019.03.026
Previous Articles Next Articles
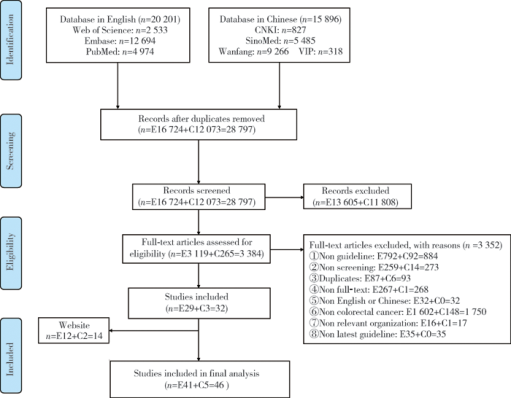
Quality assessment of global guidelines on colorectal cancer screening
Le GAO1,Shu-qing YU1,Ji-chun YANG1,Jun-ling MA2,Si-yan ZHAN1,3,Feng SUN1△( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Department of Cancer Epidemiology, Peking University Cancer Hospital & Institute, Beijing 100142, China;
3. Center of Evidence-based Medicine and Clinical Research, Peking University, Beijing 100191, China
CLC Number:
- R181.2
| [1] | World Health Organization.Cancer [EB/OL]. [2018/12/13] . |
| [2] |
Chen WQ, Zeng HM, Zheng RS , et al. Cancer incidence and mortality in china, 2007[J]. Chin J Cancer Res, 2012,24(1):1-8.
doi: 10.1007/s11670-012-0001-6 |
| [3] | 郑荣寿, 张思维, 吴良有 , 等. 中国肿瘤登记地区2008年恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2012,21(1):1-12. |
| [4] | 陈万青, 张思维, 郑荣寿 , 等. 中国2009年恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2013,22(1):2-12. |
| [5] | 陈万青, 张思维, 曾红梅 , 等. 中国2010年恶性肿瘤发病与死亡[J]. 中国肿瘤, 2014,23(1):1-10. |
| [6] | 陈万青, 郑荣寿, 曾红梅 , 等. 2011年中国恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2015,24(1):1-10. |
| [7] | 陈万青, 郑荣寿, 张思维 , 等. 2012年中国恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2016,25(1):1-8. |
| [8] | 陈万青, 郑荣寿, 张思维 , 等. 2013年中国恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2017,26(1):1-7. |
| [9] | Institute of Medicine(US). Committee to Advise the Public Health Service on Clinical Practice Guidelines. Field MJ, Lohr KN. Clinical practice guidelines: directions for a new program[M]. Washington, DC: National Academies Press, 1990. |
| [10] | Institute of Medicine(US) . Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Graham R, Man-cher M, Wolman D , et al. Clinical practice guidelines we can trust [M]. Washington, DC: National Academies Press, 2011. |
| [11] |
Shekelle PG . Clinical practice guidelines: what’s next?[J]. JAMA, 2018,320(8):757-758.
doi: 10.1001/jama.2018.9660 |
| [12] | 胡晶, 詹思延 . 中国临床实践指南制定的现状与建议[J]. 中国循证心血管医学杂志, 2013,5(3):217-218. |
| [13] | 林夏, 杨克虎, 陈耀龙 , 等. 中国临床实践指南的现状与思考[J]. 中国循证医学杂志, 2017,17(5):497-500. |
| [14] | 李江, 苏凯, 李放 , 等. 肺癌筛查领域指南方法学质量的系统评价[J]. 中国肺癌杂志, 2016,19(10):692-699. |
| [15] | 李江, 唐威, 李霓 , 等. 乳腺癌筛查指南方法学质量和报告质量的系统评价[J]. 中国循证医学杂志, 2018,18(6):629-636. |
| [16] |
Ebell MH, Thai TN, Royalty KJ . Cancer screening recommendations: an international comparison of high income countries[J]. Public Health Rev, 2018,39(1):7.
doi: 10.1186/s40985-018-0080-0 |
| [17] | 胡晶, 陈茹, 谢雁鸣 , 等. 科学和规范的改编临床实践指南[J]. 中国循证儿科杂志, 2012,7(3):226-230. |
| [18] | 张珊瑚 . 产后出血临床指南的循证评价及实用优化研究[D]. 甘肃: 兰州大学, 2014. |
| [19] | WHO. WHO handbook for guideline development[M]. 2nd ed. Geneva: World Health Organization, 2014. |
| [20] |
Brouwers MC, Kho ME, Browman GP , et al. AGREE Ⅱ: advancing guideline development, reporting, and evaluation in health care[J]. Prev Med, 2010,51(5):421-424.
doi: 10.1016/j.ypmed.2010.08.005 |
| [21] | 韦当, 王聪尧, 肖晓娟 , 等. 指南研究与评价(AGREEⅡ)工具实例解读[J]. 中国循证儿科杂志, 2013,8(4):316-319. |
| [22] | 乔舰 . 组内相关系数的理论基础及建模应用[J]. 统计与信息论坛, 2016,31(11):44-48. |
| [23] |
Bacchus CM, Dunfield L, Gorber SC , et al. Recommendations on screening for colorectal cancer in primary care[J]. CMAJ, 2016,188(5):340-348.
doi: 10.1503/cmaj.151125 |
| [24] |
Bibbins-Domingo K, Grossman DC, Curry SJ , et al. Screening for colorectal cancer: US preventive services task force recommendation statement[J]. JAMA, 2016,315(23):2564-2575.
doi: 10.1001/jama.2016.5989 |
| [25] | 王振军, 付李缘 . 大肠癌筛查共识与争议[J]. 临床外科杂志, 2018,26(10):721-723. |
| [26] | 陈宏达, 卢明, 代敏 . 我国结直肠癌人群筛查参与率现状及影响因素探讨[J]. 华西医学, 2018,33(12):1-5. |
| [27] |
Leddin D, Lieberman DA, Tse F , et al. Clinical practice guideline on screening for colorectal cancer in individuals with a family history of nonhereditary colorectal cancer or adenoma: The Cana-dian Association of Gastroenterology Banff Consensus[J]. Gastroenterology, 2018,155(5):1325-1347.
doi: 10.1053/j.gastro.2018.08.017 |
| [28] |
Sung JJ, Ng SC, Chan FK , et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening[J]. Gut, 2015,64(1):121-132.
doi: 10.1136/gutjnl-2013-306503 |
| [29] |
Lee BI, Hong SP, Kim SE , et al. Korean guidelines for colorectal cancer screening and polyp detection[J]. Clin Endosc, 2012,45(1):25-43.
doi: 10.5946/ce.2012.45.1.25 |
| [1] | Ya-nan ZHAO,Hui-yun FAN,Xiang-yu WANG,Ya-nan LUO,Rong ZHANG,Xiao-ying ZHENG. Early death and causes of death of patients with autism spectrum disorders: A systematic review [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 375-383. |
| [2] | Jia-min WANG,Qiu-ping LIU,Ming-lu ZHANG,Chao GONG,Shu-dan LIU,Wei-ye CHEN,Peng SHEN,Hong-bo LIN,Pei GAO,Xun TANG. Effectiveness of different screening strategies for type 2 diabete on preventing cardiovascular diseases in a community-based Chinese population using a decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 450-457. |
| [3] | MU Dong-liang,XUE Cheng,AN Bin,WANG Dong-xin. Epidural block associated with improved long-term survival after surgery for colorectal cancer: A retrospective cohort study with propensity score matching [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1152-1158. |
| [4] | LIU Qiu-ping,CHEN Xi-jin,WANG Jia-min,LIU Xiao-fei,SI Ya-qin,LIANG Jing-yuan,SHEN Peng,LIN Hong-bo,TANG Xun,GAO Pei. Effectiveness of different screening strategies for cardiovascular diseases prevention in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 460-466. |
| [5] | Hang-ci ZHENG,Xiao-tong LI,Peng MEN,Xiang MA,Qiang WANG,Yao-long CHEN,Suo-di ZHAI. Selecting and defining the clinical questions and outcomes of Guideline for the Emergency Treatment of Anaphylaxis [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 715-718. |
| [6] | Bao-qi ZENG,Shu-qing YU,Yao CHEN,Wei ZHAI,Bin LIU,Si-yan ZHAN,Feng SUN. Safety of biological valves for aortic valve replacement: A systematic review and meta-analysis [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 547-556. |
| [7] | SI Ya-qin, TANG Xun, ZHANG Du-dan, HE Liu, CAO Yang, WANG Jin-wei, LI Na, LIU Jian-jiang, GAO Pei, HU Yong-hua. Effectiveness of different screening strategies for primary prevention of cardiovascular diseases in a rural northern Chinese population [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 443-449. |
| [8] | GAO Ming-Yue, YANG Min, KUANG Wei-Hong, QIU Pei-Yuan. Factors and validity analysis of Mini-Mental State Examination in Chinese elderly people [J]. Journal of Peking University(Health Sciences), 2015, 47(3): 443-449. |
|
||