Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (3): 450-457. doi: 10.19723/j.issn.1671-167X.2022.03.009
Previous Articles Next Articles
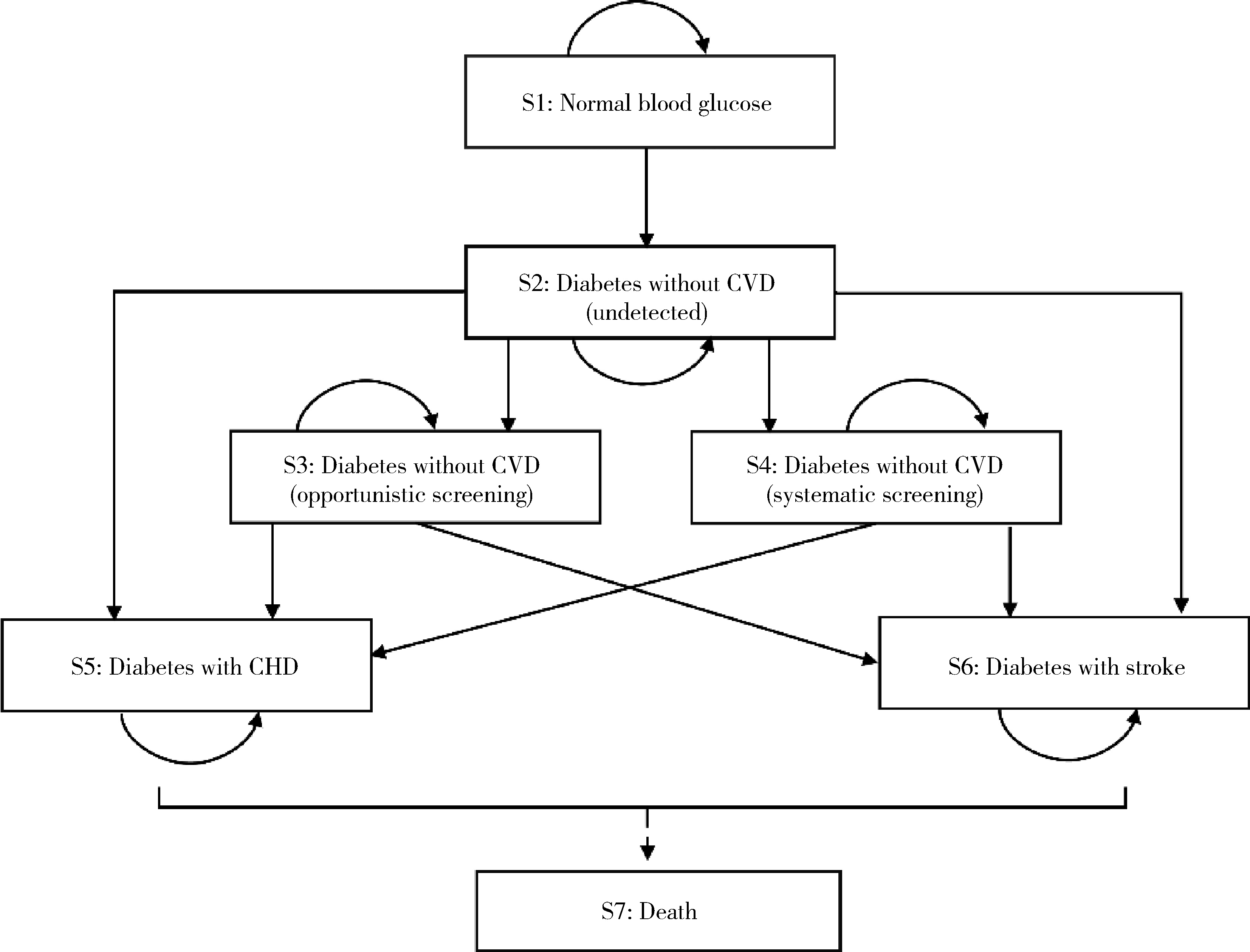
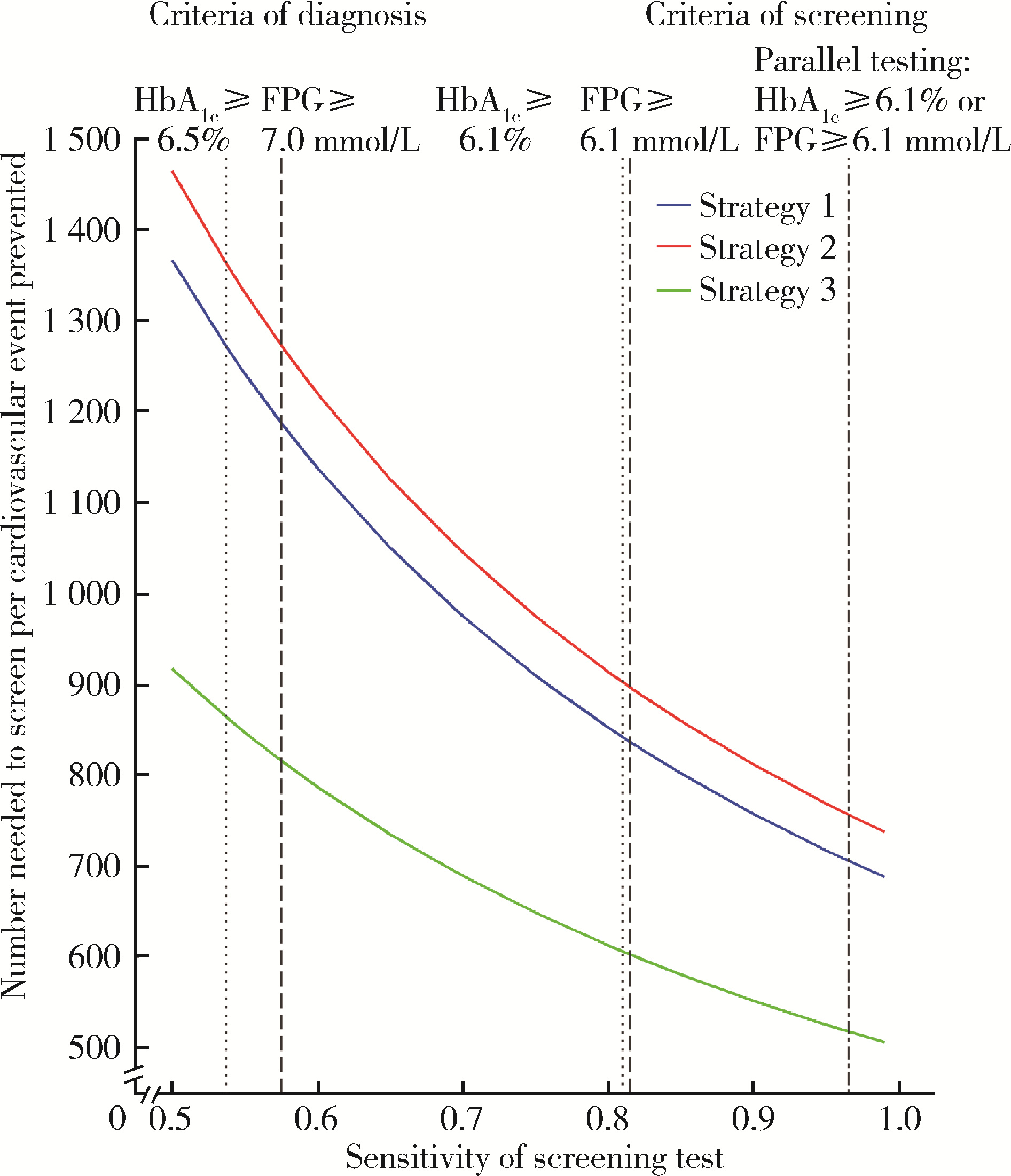
Effectiveness of different screening strategies for type 2 diabete on preventing cardiovascular diseases in a community-based Chinese population using a decision-analytic Markov model
Jia-min WANG1,Qiu-ping LIU1,Ming-lu ZHANG1,Chao GONG1,Shu-dan LIU1,Wei-ye CHEN1,Peng SHEN2,Hong-bo LIN2,Pei GAO1,3,*( ),Xun TANG1,*(
),Xun TANG1,*( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Yinzhou District Center for Disease Control and Prevention, Ningbo 315101, Zhejiang, China
3. Center for Real-World Evidence Evaluation, Clinical Research Institute, Peking University, Beijing 100191, China
CLC Number:
- R181.3+8
| 1 |
Visseren FLJ , Mach F , Smulders YM , et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice[J]. Eur Heart J, 2021, 42 (34): 3227- 3337.
doi: 10.1093/eurheartj/ehab484 |
| 2 |
Liss D T , Uchida T , Wilkes CL , et al. General health checks in adult primary care: A review[J]. JAMA, 2021, 325 (22): 2294- 2306.
doi: 10.1001/jama.2021.6524 |
| 3 | 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志, 2021, 13 (4): 315- 409. |
| 4 | American Diabetes Association Professional Practice Committee . Classification and diagnosis of diabetes: Standards of medical care in diabetes: 2022[J]. Diabetes Care, 2021, 45 (Suppl 1): S17- S38. |
| 5 |
US Preventive Services Task Force . Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement[J]. JAMA, 2021, 326 (8): 736- 743.
doi: 10.1001/jama.2021.12531 |
| 6 |
Wang L , Peng W , Zhao Z , et al. Prevalence and treatment of diabetes in China, 2013-2018[J]. JAMA, 2021, 326 (24): 2498- 2506.
doi: 10.1001/jama.2021.22208 |
| 7 |
Lin H , Tang X , Shen P , et al. Using big data to improve cardiovascular care and outcomes in China: A protocol for the Chinese electronic health records research in Yinzhou (CHERRY) study[J]. BMJ Open, 2018, 8 (2): e019698.
doi: 10.1136/bmjopen-2017-019698 |
| 8 |
Kaptoge S , Pennells L , De Bacquer D , et al. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions[J]. Lancet Global Health, 2019, 7 (10): e1332- e1345.
doi: 10.1016/S2214-109X(19)30318-3 |
| 9 |
Porta M , Curletto G , Cipullo D , et al. Estimating the delay between onset and diagnosis of type 2 diabetes from the time course of retinopathy prevalence[J]. Diabetes Care, 2014, 37 (6): 1668- 1674.
doi: 10.2337/dc13-2101 |
| 10 |
Gillies CL , Lambert PC , Abrams KR , et al. Different strategies for screening and prevention of type 2 diabetes in adults: cost effectiveness analysis[J]. BMJ, 2008, 336 (7654): 1180- 1185.
doi: 10.1136/bmj.39545.585289.25 |
| 11 |
Quan J , Li TK , Pang H , et al. Diabetes incidence and prevalence in Hong Kong, China during 2006-2014[J]. Diabetic Medicine, 2017, 34 (7): 902- 908.
doi: 10.1111/dme.13284 |
| 12 |
Bao Y , Ma X , Li H , et al. Glycated haemoglobin A1c for diagnosing diabetes in Chinese population: cross sectional epidemiological survey[J]. BMJ, 2010, 340, c2249.
doi: 10.1136/bmj.c2249 |
| 13 |
Stratton IM , Adler AI , Neil HA , et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study[J]. BMJ, 2000, 321 (7258): 405- 412.
doi: 10.1136/bmj.321.7258.405 |
| 14 |
Zhang Y , Sun J , Pang Z , et al. The impact of new screen-detected and previously known type 2 diabetes on health-related quality of life: A population-based study in Qingdao, China[J]. Qual Life Res, 2014, 23 (8): 2319- 2326.
doi: 10.1007/s11136-014-0674-z |
| 15 |
Zhang Y , Wu J , Chen Y , et al. EQ-5D-3L decrements by diabetes complications and comorbidities in China[J]. Diabetes Ther, 2020, 11 (4): 939- 950.
doi: 10.1007/s13300-020-00788-z |
| 16 |
Pan CW , Sun HP , Zhou HJ , et al. Valuing health-related quality of life in type 2 diabetes patients in China[J]. Med Decis Making, 2016, 36 (2): 234- 241.
doi: 10.1177/0272989X15606903 |
| 17 |
Feldman AL , Griffin SJ , Fharm E , et al. Screening for type 2 diabetes: Do screen-detected cases fare better[J]. Diabetologia, 2017, 60 (11): 2200- 2209.
doi: 10.1007/s00125-017-4402-4 |
| 18 |
Simmons RK , Echouffo-Tcheugui JB , Sharp SJ , et al. Screening for type 2 diabetes and population mortality over 10 years (ADDITION-Cambridge): A cluster-randomised controlled trial[J]. Lancet, 2012, 380 (9855): 1741- 1748.
doi: 10.1016/S0140-6736(12)61422-6 |
| 19 |
Kahn R , Alperin P , Eddy D , et al. Age at initiation and frequency of screening to detect type 2 diabetes: A cost-effectiveness analysis[J]. Lancet, 2010, 375 (9723): 1365- 1374.
doi: 10.1016/S0140-6736(09)62162-0 |
| 20 |
Chung S , Azar KMJ , Baek M , et al. Reconsidering the age thresholds for type Ⅱ diabetes screening in the U.S.[J]. Am J Prev Med, 2014, 47 (4): 375- 381.
doi: 10.1016/j.amepre.2014.05.012 |
| 21 |
Wang Y , Zhao L , Gao L , et al. Health policy and public health implications of obesity in China[J]. Lancet Diabetes Endocrinol, 2021, 9 (7): 446- 461.
doi: 10.1016/S2213-8587(21)00118-2 |
| 22 |
Hoerger TJ , Hicks KA , Sorensen SW , et al. Cost-effectiveness of screening for pre-diabetes among overweight and obese U.S. adults[J]. Diabetes Care, 2007, 30 (11): 2874- 2879.
doi: 10.2337/dc07-0885 |
| [1] | Peiheng ZHANG, Ying GAO, Honghua WU, Jian ZHANG, Junqing ZHANG. Fulminant type 1 diabetes mellitus with acute pancreatitis: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 923-927. |
| [2] | Tianjing ZHOU,Qiuping LIU,Minglu ZHANG,Xiaofei LIU,Jiali KANG,Peng SHEN,Hongbo LIN,Xun TANG,Pei GAO. Comparison of initiation of antihypertensive therapy strategies for primary prevention of cardiovascular diseases in Chinese population: A decision-analytic Markov modelling study [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 441-447. |
| [3] | Yujia MA,Ranli LU,Zechen ZHOU,Xiaoyi LI,Zeyu YAN,Yiqun WU,Dafang CHEN. Association between insomnia and type 2 diabetes: A two-sample Mendelian rando-mization study [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 174-178. |
| [4] | Lei BAO,Xia-xia CAI,Ming-yuan ZHANG,Lei-lei REN. Effect of vitamin D3 on mild cognitive impairment in type 2 diabetic mice and its possible mechanism [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 587-592. |
| [5] | Xiao-yue ZHANG,Yu-xin LIN,Ying JIANG,Lan-chao ZHANG,Mang-yan DONG,Hai-yi CHI,Hao-yu DONG,Li-jun MA,Zhi-jing LI,Chun CHANG. Mediating effect of self-efficacy on self-management ability and self-management behavior in patients with type 2 diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 450-455. |
| [6] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [7] | Ming-lu ZHANG,Qiu-ping LIU,Chao GONG,Jia-min WANG,Tian-jing ZHOU,Xiao-fei LIU,Peng SHEN,Hong-bo LIN,Xun TANG,Pei GAO. Comparison of aspirin treatment strategies for primary prevention of cardiovascular diseases: A decision-analytic Markov modelling study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 480-487. |
| [8] | Yang-yang CHEN,Yu-bo ZHOU,Jing YANG,Yu-meng HUA,Peng-bo YUAN,Ai-ping LIU,Yuan WEI. Effects of gestational weight on the association between serum high sensitivity C reaction protein and gestational diabetes mellitus among twin gestations: A cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 427-433. |
| [9] | Chao GONG,Qiu-ping LIU,Jia-min WANG,Xiao-fei LIU,Ming-lu ZHANG,Han YANG,Peng SHEN,Hong-bo LIN,Xun TANG,Pei GAO. Effectiveness of statin treatment strategies for primary prevention of cardiovascular diseases in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 443-449. |
| [10] | WU Jun-hui,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,QIN Xue-ying,WANG Meng-ying,WANG Xiao-wen,WANG Jia-ting,HU Yong-hua. Incidence and risk factors of ischemic stroke in patients with type 2 diabetes among urban workers in Beijing, China [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 249-254. |
| [11] | XU Xin-ran,HUO Peng-cheng,HE Lu,MENG Huan-xin,ZHU Yun-xuan,JIN Dong-si-qi. Comparison of initial periodontal therapy and its correlation with white blood cell level in periodontitis patients with or without diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 48-53. |
| [12] | GUO Zi-ning, LIANG Zhi-sheng, ZHOU Yi, ZHANG Na, HUANG Jie. Genetic study of cardiovascular disease subtypes defined by International Classification of Diseases [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 453-459. |
| [13] | LIU Qiu-ping,CHEN Xi-jin,WANG Jia-min,LIU Xiao-fei,SI Ya-qin,LIANG Jing-yuan,SHEN Peng,LIN Hong-bo,TANG Xun,GAO Pei. Effectiveness of different screening strategies for cardiovascular diseases prevention in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 460-466. |
| [14] | GUO Hong-ping,ZHAO Ai,XUE Yong,MA Liang-kun,ZHANG Yu-mei,WANG Pei-yu. Relationship between nutrients intake during pregnancy and the glycemic control effect in pregnant women with gestational diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 467-472. |
| [15] | WU Jun-hui,CHEN Hong-bo,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,WANG Meng-ying,WANG Si-yue,WANG Xiao-wen,WANG Jia-ting,YU Huan,HU Yong-hua. Prevalence and risk factors of osteoarthritis in patients with type 2 diabetes in Beijing, China from 2015 to 2017 [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 518-522. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 388
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 800
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||