Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (3): 458-467. doi: 10.19723/j.issn.1671-167X.2022.03.010
Previous Articles Next Articles
Long short-term memory and Logistic regression for mortality risk prediction of intensive care unit patients with stroke
Yu-han DENG1,Yong JIANG2,3,Zi-yao WANG1,Shuang LIU1,Yu-xin WANG1,Bao-hua LIU1,*( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. China National Clinical Research Center for Neurological Diseases, Department of Neurology, Beijing Tian Tan Hospital, Capital Medical University, Beijing 100050, China
3. Beijing Advanced Innovation Center for Big Data-Based Precision Medicine (Beihang University & Capital Medical University), Beijing 100070, China
CLC Number:
- R743.3
| 1 |
Katan M , Luft A . Global burden of stroke[J]. Semin Neurol, 2018, 38 (2): 208- 211.
doi: 10.1055/s-0038-1649503 |
| 2 |
Rochmah TN , Rahmawati IT , Dahlui M , et al. Economic burden of stroke disease: A systematic review[J]. Int J Environ Res Public Health, 2021, 18 (14): 7552.
doi: 10.3390/ijerph18147552 |
| 3 |
Sarti C , Rastenyte D , Cepaitis Z , et al. International trends in mortality from stroke, 1968 to 1994[J]. Stroke, 2000, 31 (7): 1588- 1601.
doi: 10.1161/01.STR.31.7.1588 |
| 4 |
Handschu R , Haslbeck M , Hartmann A , et al. Mortality prediction in critical care for acute stroke: Severity of illness-score or coma-scale?[J]. J Neurol, 2005, 252 (10): 1249- 1254.
doi: 10.1007/s00415-005-0853-5 |
| 5 |
Ryan L , Lam C , Mataraso S , et al. Mortality prediction model for the triage of COVID-19, pneumonia, and mechanically ventilated ICU patients: A retrospective study[J]. Ann Med Surg (Lond), 2020, 59, 207- 216.
doi: 10.1016/j.amsu.2020.09.044 |
| 6 |
Nemati S , Holder A , Razmi F , et al. An interpretable machine learning model for accurate prediction of sepsis in the ICU[J]. Crit Care Med, 2018, 46 (4): 547- 553.
doi: 10.1097/CCM.0000000000002936 |
| 7 |
LeCun Y , Bengio Y , Hinton G . Deep learning[J]. Nature, 2015, 521 (7553): 436- 444.
doi: 10.1038/nature14539 |
| 8 |
Cheng JZ , Ni D , Chou YH , et al. Computer-aided diagnosis with deep learning architecture: Applications to breast lesions in US images and pulmonary nodules in CT scans[J]. Sci Rep, 2016, 6, 24454.
doi: 10.1038/srep24454 |
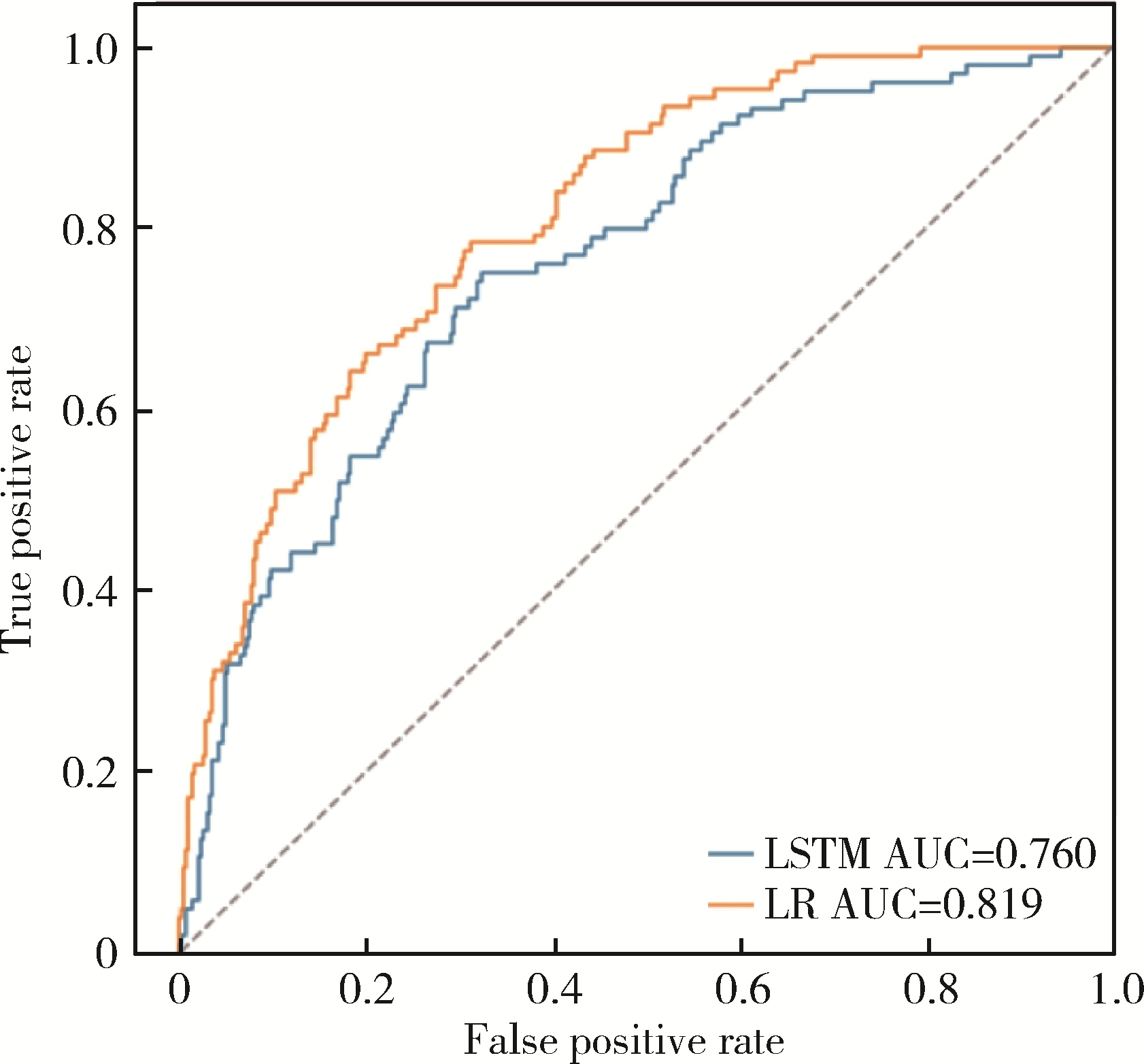
| 9 |
Kooi T , Litjens G , van Ginneken B , et al. Large scale deep learning for computer aided detection of mammographic lesions[J]. Med Image Anal, 2017, 35, 303- 312.
doi: 10.1016/j.media.2016.07.007 |
| 10 | Choi E , Bahadori MT , Schuetz A , et al. Doctor AI: Predicting clinical events via recurrent neural networks[J]. JMLR Workshop Conf Proc, 2016, 56, 301- 318. |
| 11 |
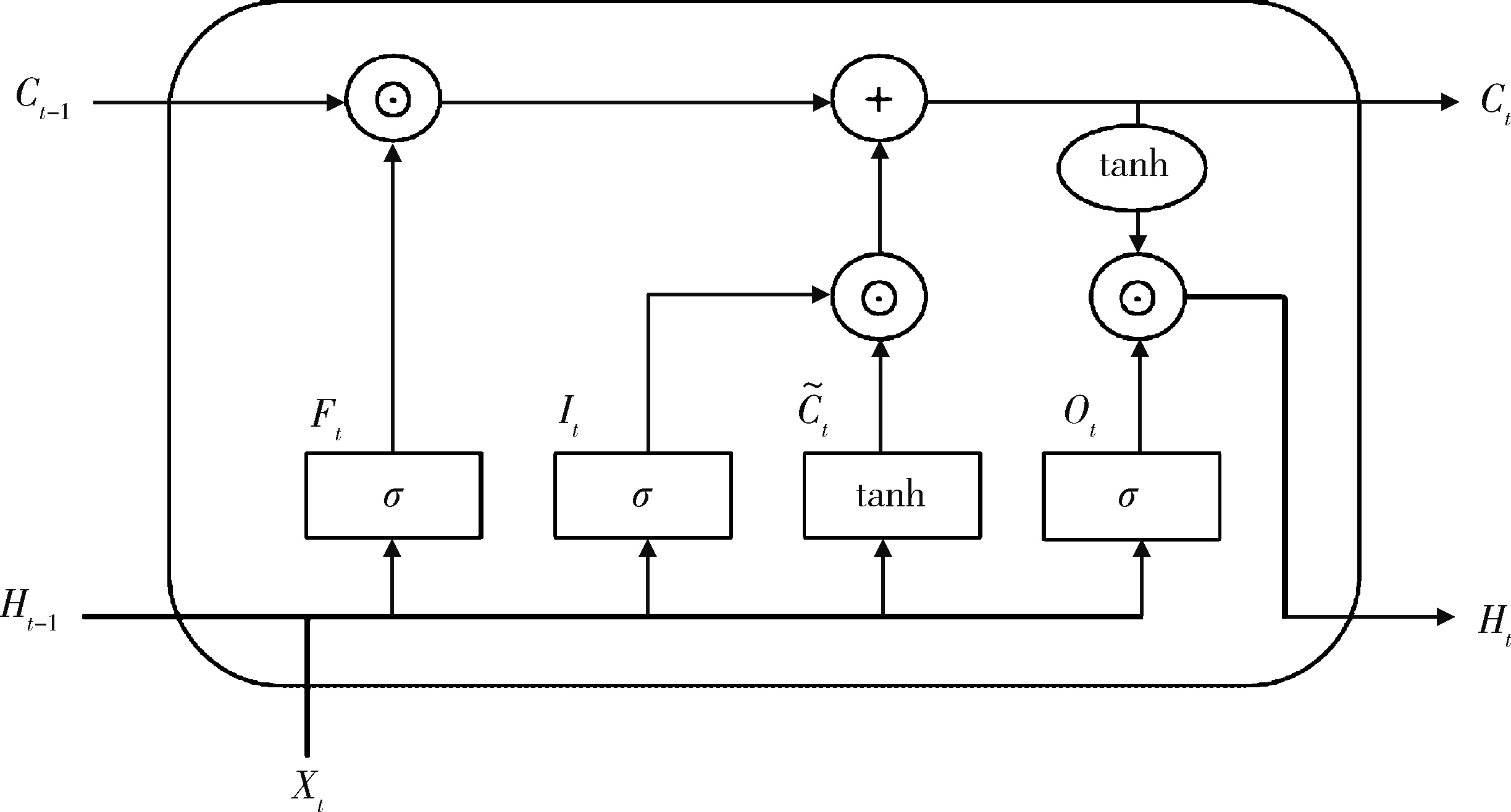
Hochreiter S , Schmidhuber J . Long short-term memory[J]. Neural Comput, 1997, 9 (8): 1735- 1780.
doi: 10.1162/neco.1997.9.8.1735 |
| 12 |
Thorsen-Meyer HC , Nielsen AB , Nielsen AP , et al. Dynamic and explainable machine learning prediction of mortality in patients in the intensive care unit: A retrospective study of high-frequency data in electronic patient records[J]. Lancet Digit Health, 2020, 2 (4): e179- e191.
doi: 10.1016/S2589-7500(20)30018-2 |
| 13 | Xia J , Pan S , Zhu M , et al. A long short-term memory ensemble approach for improving the outcome prediction in intensive care unit[J]. Comput Math Methods Med, 2019, 2019, 8152713. |
| 14 |
Maheshwari S , Agarwal A , Shukla A , et al. A comprehensive evaluation for the prediction of mortality in intensive care units with LSTM networks: Patients with cardiovascular disease[J]. Biomed Tech (Berl), 2020, 65 (4): 435- 446.
doi: 10.1515/bmt-2018-0206 |
| 15 |
Ho LV , Aczon M , Ledbetter D , et al. Interpreting a recurrent neural network's predictions of ICU mortality risk[J]. J Biomed Inform, 2021, 114, 103672.
doi: 10.1016/j.jbi.2021.103672 |
| 16 | 王琦琦, 于石成, 亓晓, 等. Logistic族回归及其应用[J]. 中华预防医学杂志, 2019, 53 (9): 955- 960. |
| 17 |
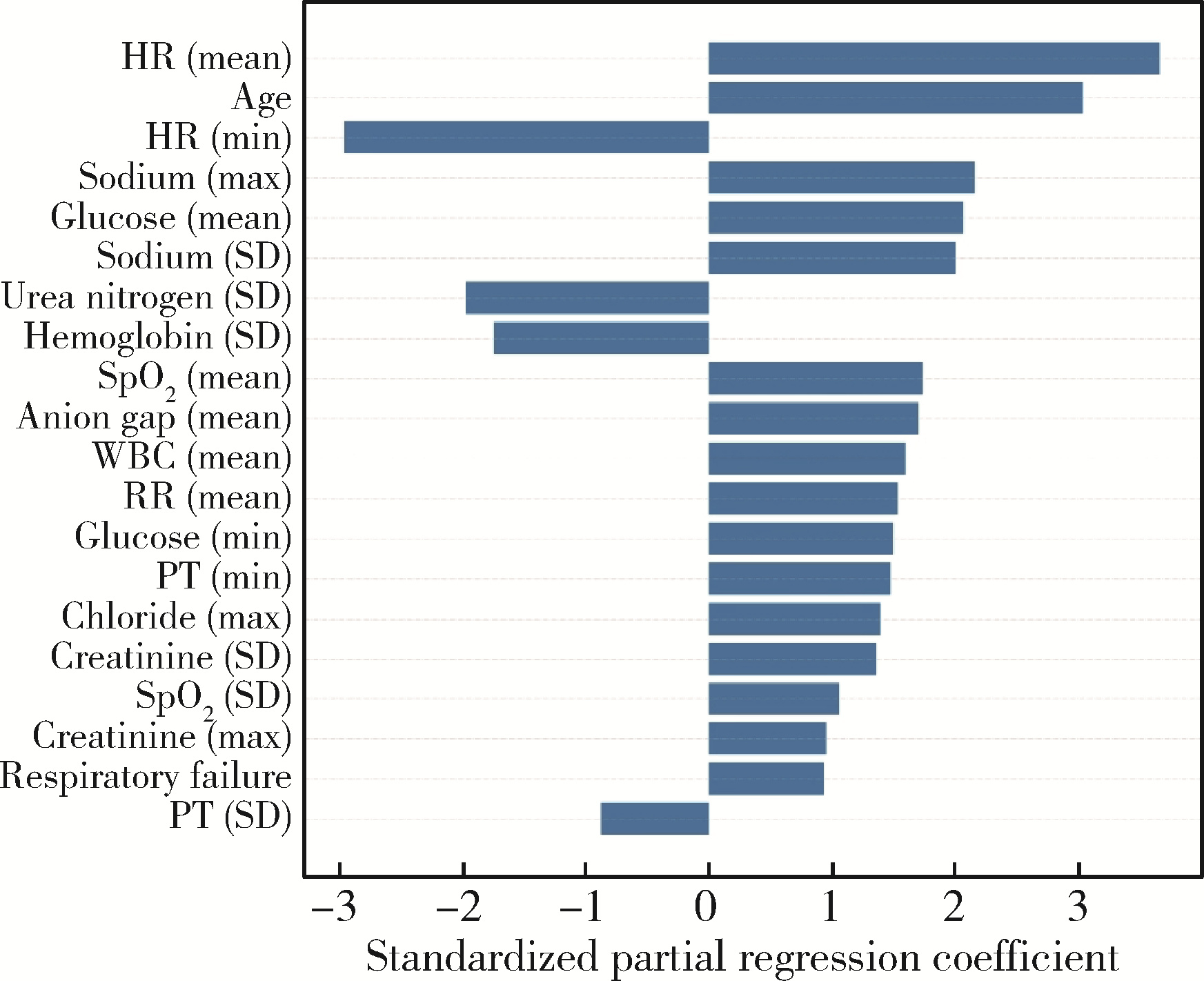
Jhou HJ , Chen PH , Yang LY , et al. Plasma anion gap and risk of in-hospital mortality in patients with acute ischemic stroke: Analysis from the MIMIC-Ⅳ database[J]. J Pers Med, 2021, 11 (10): 1004.
doi: 10.3390/jpm11101004 |
| 18 |
Zhao N , Hu W , Wu Z , et al. The red blood cell distribution width-albumin ratio: A promising predictor of mortality in stroke patients[J]. Int J Gen Med, 2021, 14, 3737- 3747.
doi: 10.2147/IJGM.S322441 |
| 19 | 邱锡鹏. 神经网络与深度学习[M]. 北京: 机械工业出版社, 2020: 141- 145. |
| 20 |
Kaji DA , Zech JR , Kim JS , et al. An attention based deep lear-ning model of clinical events in the intensive care unit[J]. PLoS One, 2019, 14 (2): e0211057.
doi: 10.1371/journal.pone.0211057 |
| 21 |
Lopez Bernal J , Soumerai S , Gasparrini A . A methodological framework for model selection in interrupted time series studies[J]. J Clin Epidemiol, 2018, 103, 82- 91.
doi: 10.1016/j.jclinepi.2018.05.026 |
| 22 |
Yu Y , Si X , Hu C , et al. A review of recurrent neural networks: LSTM cells and network architectures[J]. Neural Comput, 2019, 31 (7): 1235- 1270.
doi: 10.1162/neco_a_01199 |
| 23 |
Gandin I , Scagnetto A , Romani S , et al. Interpretability of time-series deep learning models: A study in cardiovascular patients admitted to intensive care unit[J]. J Biomed Inform, 2021, 121, 103876.
doi: 10.1016/j.jbi.2021.103876 |
| 24 |
Weimar C , Ziegler A , Konig IR , et al. Predicting functional outcome and survival after acute ischemic stroke[J]. J Neurol, 2002, 249 (7): 888- 895.
doi: 10.1007/s00415-002-0755-8 |
| 25 | Koyama T , Uchiyama Y , Domen K . Outcome in stroke patients is associated with age and fractional anisotropy in the cerebral peduncles: A multivariate regression study[J]. Prog Rehabil Med, 2020, 5, 20200006. |
| 26 |
Duarte E , Marco E , Muniesa JM , et al. Early detection of non-ambulatory survivors six months after stroke[J]. NeuroRehabilitation, 2010, 26 (4): 317- 323.
doi: 10.3233/NRE-2010-0568 |
| 27 |
Fuentes B , Castillo J , San Jose B , et al. The prognostic value of capillary glucose levels in acute stroke[J]. Stroke, 2009, 40 (2): 562- 568.
doi: 10.1161/STROKEAHA.108.519926 |
| 28 |
Baird TA , Parsons MW , Phanh T , et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome[J]. Stroke, 2003, 34 (9): 2208- 2214.
doi: 10.1161/01.STR.0000085087.41330.FF |
| 29 |
Förstermann U , Münzel T . Endothelial nitric oxide synthase in vascular disease: From marvel to menace[J]. Circulation, 2006, 113 (13): 1708- 1714.
doi: 10.1161/CIRCULATIONAHA.105.602532 |
| 30 |
Virley D , Hadingham SJ , Roberts JC , et al. A new primate model of focal stroke: Endothelin-1-induced middle cerebral artery occlusion and reperfusion in the common marmoset[J]. J Cereb Blood Flow Metab, 2004, 24 (1): 24- 41.
doi: 10.1097/01.WCB.0000095801.98378.4A |
| 31 |
Martini SR , Kent TA . Hyperglycemia in acute ischemic stroke: A vascular perspective[J]. J Cereb Blood Flow Metab, 2007, 27 (3): 435- 451.
doi: 10.1038/sj.jcbfm.9600355 |
| 32 |
You S , Zheng D , Zhong C , et al. Prognostic significance of blood urea nitrogen in acute ischemic stroke[J]. Circ J, 2018, 82 (2): 572- 578.
doi: 10.1253/circj.CJ-17-0485 |
| 33 |
Cheng J , Sun J , Yao K , et al. A variable selection method based on mutual information and variance inflation factor[J]. Spectrochim Acta A Mol Biomol Spectrosc, 2022, 268, 120652.
doi: 10.1016/j.saa.2021.120652 |
| 34 | Ge W , Huh JW , Park YR , et al. An interpretable ICU mortality prediction model based on Logistic regression and recurrent neural networks with LSTM units[J]. AMIA Annu Symp Proc, 2018, 2018, 460- 469. |
| 35 |
Koppe G , Meyer-Lindenberg A , Durstewitz D . Deep learning for small and big data in psychiatry[J]. Neuropsychopharmacology, 2021, 46 (1): 176- 190.
doi: 10.1038/s41386-020-0767-z |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [3] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [4] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [5] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [6] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [7] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [8] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [9] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [10] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [11] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [12] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [13] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [14] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
| [15] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
|
||