Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (4): 702-707. doi: 10.19723/j.issn.1671-167X.2023.04.022
Previous Articles Next Articles
Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma
Han LU1,Jian-yun ZHANG2,Rong YANG1,Le XU1,Qing-xiang LI1,Yu-xing GUO1,*( ),Chuan-bin GUO1,*(
),Chuan-bin GUO1,*( )
)
- 1. Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
2. Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R739.8
| 1 |
Montero PH , Patel SG . Cancer of the oral cavity[J]. Surg Oncol Clin N Am, 2015, 24 (3): 491- 508.
doi: 10.1016/j.soc.2015.03.006 |
| 2 |
Fives C , Nae A , Roche P , et al. Impact of mandibular invasion on prognosis in oral squamous cell carcinoma four centimeters or less in size[J]. Laryngoscope, 2017, 127 (4): 849- 854.
doi: 10.1002/lary.26211 |
| 3 |
Fried D , Mullins B , Weissler M , et al. Prognostic significance of bone invasion for oral cavity squamous cell carcinoma considered T1/T2 by American joint committee on cancer size criteria[J]. Head Neck, 2014, 36 (6): 776- 781.
doi: 10.1002/hed.23367 |
| 4 | 万艳, 尚政军. 牙龈癌的流行病学危险因素研究[J]. 临床口腔医学杂志, 2013, 29 (7): 402- 404. |
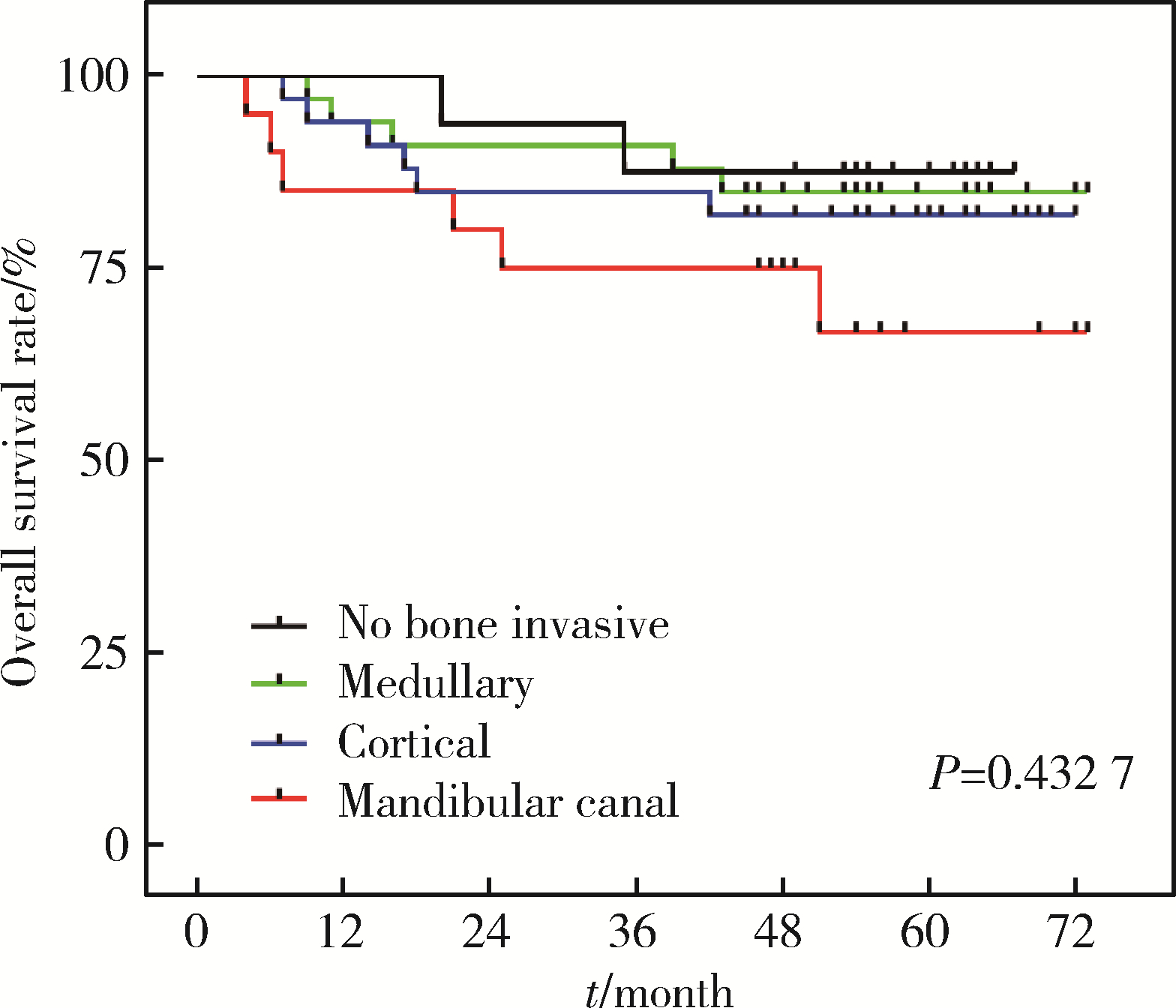
| 5 | Yoshida S , Shimo T , Murase Y , et al. The prognostic implications of bone invasion in gingival squamous cell carcinoma[J]. Anticancer Res, 2018, 38 (2): 955- 962. |
| 6 |
Ebrahimi A , Murali R , Gao K , et al. The prognostic and staging implications of bone invasion in oral squamous cell carcinoma[J]. Cancer, 2011, 117 (19): 4460- 4467.
doi: 10.1002/cncr.26032 |
| 7 |
Lee KC , Chuang SK , Philipone EM , et al. Which clinicopathologic factors affect the prognosis of gingival squamous cell carcinoma: A population analysis of 4 345 cases[J]. J Oral Maxillofac Surg, 2019, 77 (5): 986- 993.
doi: 10.1016/j.joms.2019.01.007 |
| 8 |
Okura M , Yanamoto S , Umeda M , et al. Prognostic and staging implications of mandibular canal invasion in lower gingival squamous cell carcinoma[J]. Cancer Med, 2016, 5 (12): 3378- 3385.
doi: 10.1002/cam4.899 |
| 9 | Brierley J , Gospodarowicz MK , Wittekind C . TNM classification of malignant tumours[M]. 8ed Chichester, West Sussex, UK & Hoboken, NJ: John Wiley & Sons, Inc, 2017. |
| 10 |
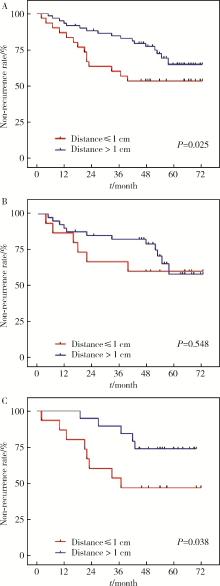
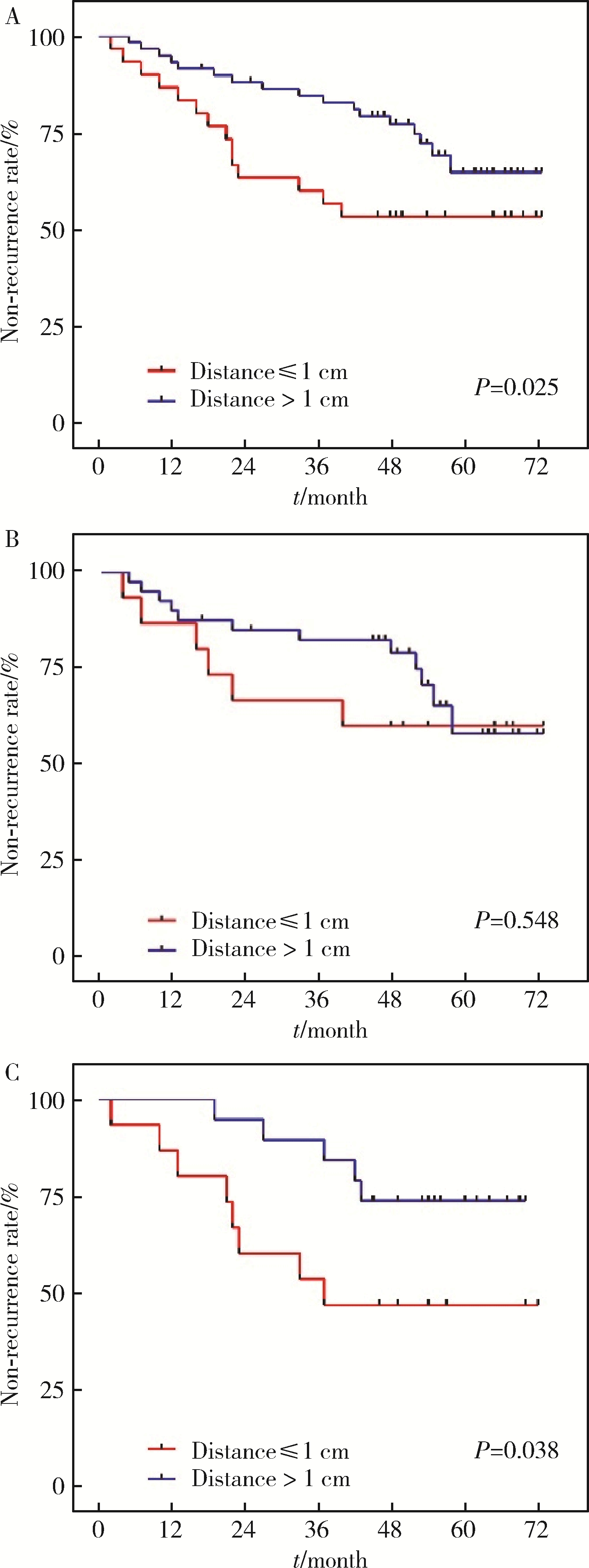
Smits RWH , Ten Hove I , Dronkers EAC , et al. Evaluation of bone resection margins of segmental mandibulectomy for oral squamous cell carcinoma[J]. Int J Oral Maxillofac Surg, 2018, 47 (8): 959- 964.
doi: 10.1016/j.ijom.2018.03.006 |
| 11 |
Ahmad JG , Namin AW , Jorgensen JB , et al. Mandibular invasion by oral squamous cell carcinoma: Clinicopathologic features of 74 cases[J]. Otolaryngol Head Neck Surg, 2019, 160 (6): 1034- 1041.
doi: 10.1177/0194599818821859 |
| 12 | Singh A , Mair M , Singhvi H , et al. Incidence, predictors and impact of positive bony margins in surgically treated T4 stage cancers of the oral cavity[J]. Oral Oncol, 2019, 90 (3): 8- 12. |
| 13 |
Cariati P , Serrano AC , Solis JF , et al. Intraoperative cytological examination of bone medullary. A useful technique to predict the extension of bone invasion in segmental mandibulectomy[J]. Am J Otolaryngol, 2019, 40 (5): 743- 746.
doi: 10.1016/j.amjoto.2019.07.005 |
| 14 |
Haase C , Lethaus B , Knuchel-Clarke R , et al. Development of a rapid analysis method for bone resection margins for oral squamous cell carcinoma by immunoblotting[J]. Head Neck Pathol, 2018, 12 (2): 210- 220.
doi: 10.1007/s12105-017-0856-4 |
| 15 |
Niu LX , Feng ZE , Wang DC , et al. Prognostic factors in mandi-bular gingival squamous cell carcinoma: A 10-year retrospective study[J]. Int J Oral Maxillofac Surg, 2017, 46 (2): 137- 143.
doi: 10.1016/j.ijom.2016.09.014 |
| 16 |
Nieberler M , Haussler P , Kesting MR , et al. Intraoperative cell isolation for a cytological assessment of bone resection margins in patients with head and neck cancer[J]. Br J Oral Maxillofac Surg, 2017, 55 (5): 510- 516.
doi: 10.1016/j.bjoms.2017.02.006 |
| 17 |
Nieberler M , Haussler P , Kesting MR , et al. Clinical impact of intraoperative cytological assessment of bone resection margins in patients with head and neck carcinoma[J]. Ann Surg Oncol, 2016, 23 (11): 3579- 3586.
doi: 10.1245/s10434-016-5208-1 |
| 18 |
Gou L , Yang W , Qiao X , et al. Marginal or segmental mandibulectomy: treatment modality selection for oral cancer: A systematic review and meta-analysis[J]. Int J Oral Maxillofac Surg, 2018, 47 (1): 1- 10.
doi: 10.1016/j.ijom.2017.07.019 |
| 19 |
Namin AW , Bollig CA , Harding BC , et al. Implications of tumor size, subsite, and adjuvant therapy on outcomes in pT4aN0 oral cavity carcinoma[J]. Otolaryngol Head Neck surg, 2020, 162 (5): 683- 692.
doi: 10.1177/0194599820904679 |
| 20 | 李传真, 郭传瑸. 口腔颌面部鳞癌原发灶部位对颈淋巴结转移区域的影响[J]. 北京大学学报(医学版), 2014, 46 (3): 469- 473. |
| 21 |
Brockhoff HC , Kim RY , Braun TM , et al. Correlating the depth of invasion at specific anatomic locations with the risk for regional metastatic disease to lymph nodes in the neck for oral squamous cell carcinoma[J]. Head Neck, 2017, 39 (5): 974- 979.
doi: 10.1002/hed.24724 |
| 22 |
Wang Y , Li Q , Xu L , et al. Cancer stemness of CD10-positive cells regulated by Hedgehog pathway promotes the resistance to cisplatin in oral squamous cell carcinoma[J]. Oral Dis, 2021, 27 (6): 1403- 1411.
doi: 10.1111/odi.13673 |
| 23 |
Li Q , Wang Y , Xu L , et al. High level of CD10 expression is associated with poor overall survival in patients with head and neck cancer[J]. Int J Oral Maxillofac Surg, 2021, 50 (7): 857- 864.
doi: 10.1016/j.ijom.2020.07.037 |
| 24 |
Nassiri AM , Campbell BR , Mannion K , et al. Survival outcomes in T4aN0M0 mandibular gingival squamous cell carcinoma treated with surgery alone[J]. Otolaryngol Head Neck Surg, 2019, 160 (5): 870- 875.
doi: 10.1177/0194599818821892 |
| 25 |
Hasegawa T , Yanamoto S , Otsuru M , et al. Multi-center retrospective study of the prognosis and treatment outcomes of Japanese oral squamous cell carcinoma patients with single lymph node metastasis and extra nodal extension[J]. J Surg Oncol, 2018, 117 (8): 1736- 1743.
doi: 10.1002/jso.25083 |
| 26 |
Lubek J , El-Hakim M , Salama AR , et al. Gingival carcinoma: Retrospective analysis of 72 patients and indications for elective neck dissection[J]. Br J Oral Maxillofac Surg, 2011, 49 (3): 182- 185.
doi: 10.1016/j.bjoms.2010.04.005 |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [3] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [4] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [5] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [6] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [7] | Junqi SU,Xiaoying WANG,Zhiqiang SUN. Establishment and verification of a prognostic nomogram for survival of tongue squamous cell carcinoma patients who underwent cervical dissection [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 120-130. |
| [8] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [9] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [10] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [11] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [12] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [13] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
| [14] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [15] | Qian SU,Xin PENG,Chuan-xiang ZHOU,Guang-yan YU. Clinicopathological characteristics and prognosis of non-Hodgkin lymphoma in oral and maxillofacial regions: An analysis of 369 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 13-21. |
|
||