Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (4): 733-736. doi: 10.19723/j.issn.1671-167X.2019.04.024
Previous Articles Next Articles
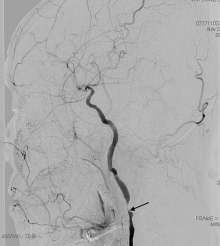
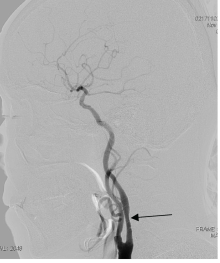
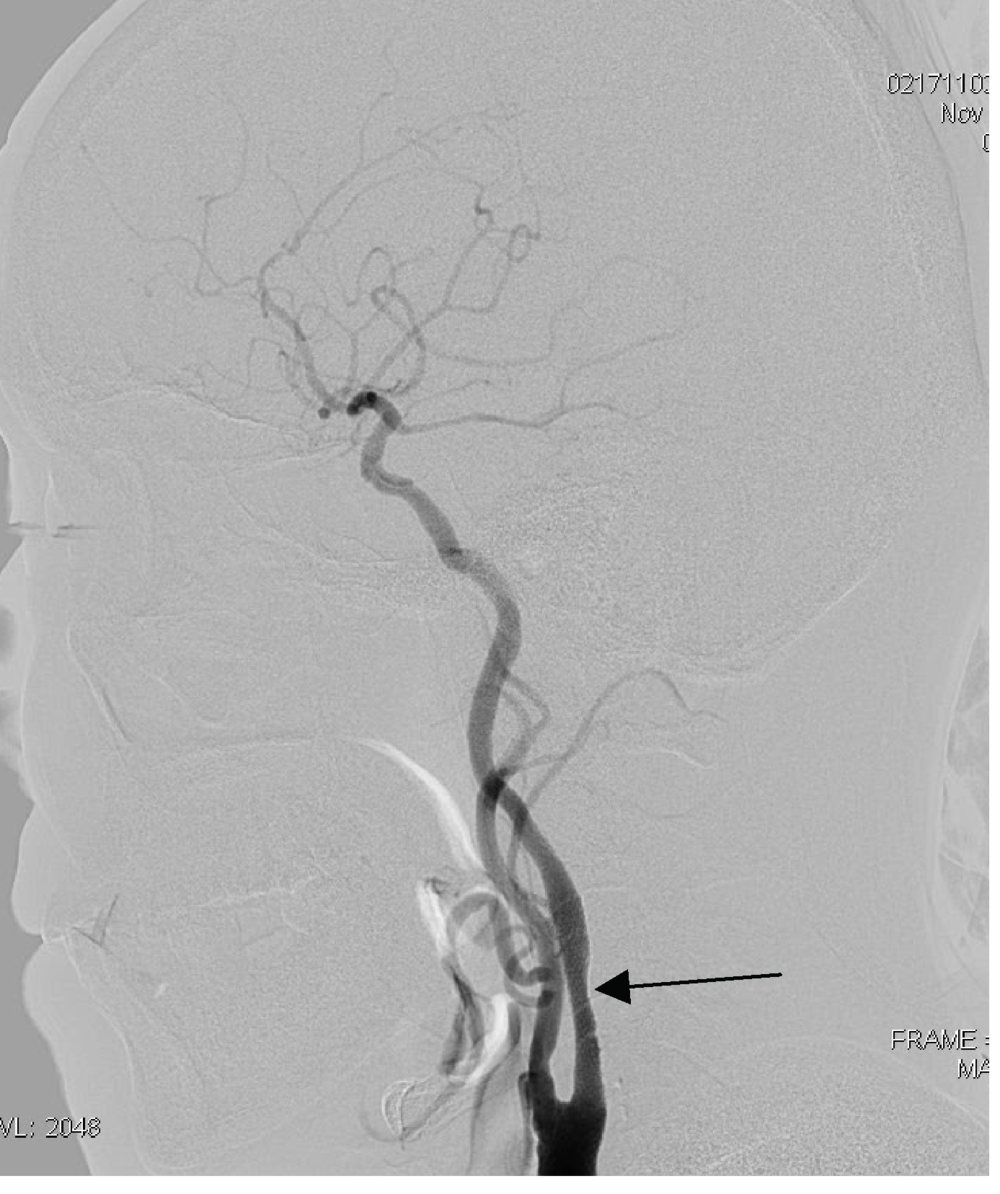
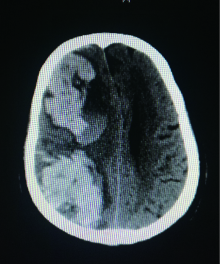
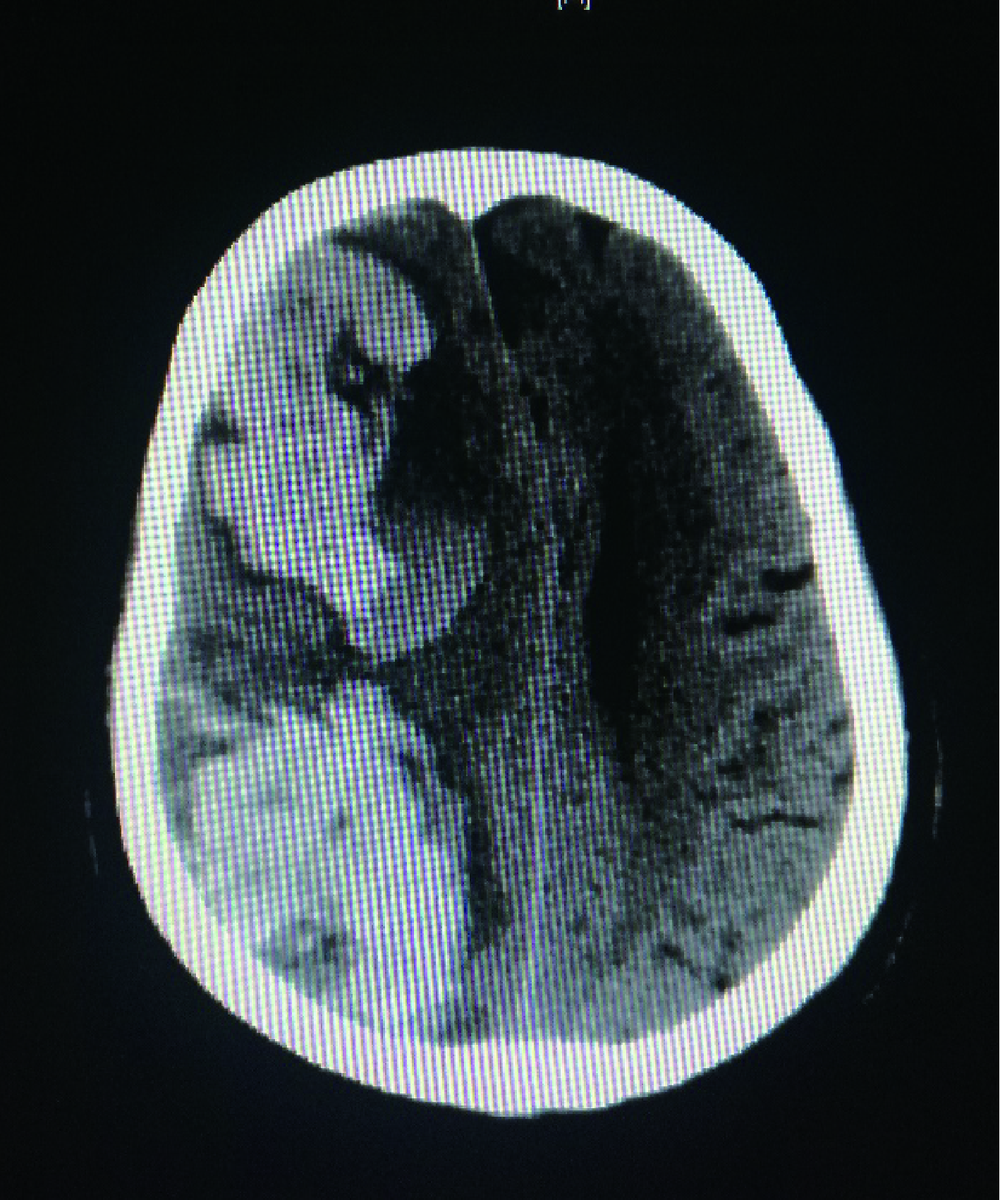
Cerebral hyper perfusion syndrome after carotid artery stenting
Zi-chang JIA1,Huan-ju BIAN2,Jin-tao HAN1,Hai-yan ZHAO3,Jing-yuan LUAN1,Chang-ming WANG1,Xuan LI1,△( )
)
- 1.Department of Interventional Radiology and Vascular Surgery, Peking University Third Hospital, Beijing 100191, China
2. Department of Neurology,Guanxian Hospital,Guanxian 252500, Shandong, China
3.Department of Neurology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R619
| [1] | Fazekas G, Kasza G, Arató E , et al. Cerebral hyper perfusion syndrome and blood pressure control[J]. Orv Hetil, 2015,156(26):1049-1053. |
| [2] | Bouri S, Thapar A, Shalhoub J , et al. Hypertension and the post-carotid endarterectomy cerebral hyperperfusion syndrome[J]. Eur J Vasc Endovasc Surg, 2011,41(2):229-237. |
| [3] | North American Symptomatic Carotid Endarterectomy Trial. Methods,patient characteristics,and progress[J]. Stroke, 1991,22(6):711-720. |
| [4] | 黄家星, 林文华, 刘丽萍 , 等. 缺血性卒中侧支循环评估与干预中国专家共识[J]. 中国卒中杂志, 2013,8(4):285-293. |
| [5] | Ogasawara K, Sakai N, Kuroiwa T . Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients[J]. J Neurosurg, 2007,107(6):1130-1136. |
| [6] | Fujimura M, Niizuma K, Endo H , et al. Quantitative analysis of early postoperative cerebral blood flow contributes to the prediction and diagnosis of cerebral hyperperfusion syndrome after revas-cularization surgery for moyamoya disease[J]. Neurol Res, 2015,37(2):131-138. |
| [7] | Kitagawa K . Carotid stenosis, baroreceptor sensitivity and cerebral autoregulation: implication for cerebral hyperperfusion syndrome[J]. Circ J, 2010,74(10):2058-2059. |
| [8] | Macfarlane R, Moskowitz MA, Sakas DE , et al. The role of neuroeffector mechanisms in cerebral hyperperfusion syndromes[J]. J Neurosurg, 1991,75(6):845-855. |
| [9] | Moulakakis KG, Mylonas SN, Sfyroeras GS , et al. Hyper perfusion syndrome after carotid revascularization[J]. J Vasc Surg, 2009,49(4):1060-1068. |
| [10] | Mo DP, Luo G, Wang B , et al. Staged carotid artery angioplasty and stenting for patients with high-grade carotid stenosis with high risk of developing hyperperfusion injury: a retrospective analysis of 44 cases[J]. Stroke Vasc Neurol, 2016,1(4):147-153. |
| [11] | Wu F, Huang L, Lu G , et al. Two-stage cerebral hemodynamic changes in staged carotid angioplasty and stenting[J]. J Stroke Cerebrovasc Dis, 2016,25(12):2814-2820. |
| [1] | ZHOU Bo-lin,LI Wei-shi,SUN Chui-guo,QI Qiang,CHEN Zhong-qiang,ZENG Yan. Risk factors for multiple debridements of the patients with deep incisional surgical site infection after spinal surgery [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 286-292. |
| [2] | Wei ZHANG,Pei-xun ZHANG. Analysis of prophylactic effect of extended-duration anticoagulant drugs in elderly patients undergoing hip fracture [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 501-504. |
| [3] | WANG Bo-jie, GUO Chao, LI Chun-jing, MU Dong-liang. Prevalance of peri-anesthesia allergy and its related risk factor: a retrospective survey from 2012-2017 [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 193-199. |
| [4] | WANG Yu, MENG Yi-sen, FAN Yu, CHEN Cheng, YU Wei, HAO Han, HAN Wen-ke, HAO Jin-rui, JIN Jie, ZHOU Li-qun. Effect of gum chewing on bowel function recovery in patients after radical cystectomy with urinary diversion [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 822-824. |
| [5] | LIU Kun, XU Zong-yuan, MENG Jun-song, FU Guang-bo, GU Suo, GU Min. Impact of preoperative nutritional risk on complications after radical cystectomy [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 800-803. |
| [6] | LI Hong-Liang, ZHU Xi, ME Gai-Qi, WANG Zong-Yu. Vertebral artery injury caused by internal jugular vein catheterization: two casereports [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 355-357. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 484
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 1425
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||